Abstract
In fulminant myocarditis complicated by cardiogenic shock, early mechanical circulatory support (MCS) may prevent cardiomyopathy and death. We sought to examine the outcomes of patients with fulminant myocarditis supported with MCS. A retrospective review of patients with acute cardiogenic shock treated with MCS from 2007 to 2013 was conducted, and patients with a diagnosis of fulminant myocarditis were included in this series. At our center, 260 patients received MCS for acute cardiogenic shock, and 11 were implanted for fulminant myocarditis. Eight received the Centrimag biventricular assist device (BIVAD), and three received veno-arterial extracorporeal membrane oxygenator (VA ECMO), though 1 VA ECMO-supported patient was transitioned to BIVAD due to refractory shock. The mean acute support time was 14.7 ± 4.4 days. Two patients required long-term left ventricular assist devices and were further supported for 55 and 112 days. Eight patients recovered with a mean ejection fraction of 54 ± 7 %, and one was successfully transplanted. Eight patients survived to discharge (73 %) with mean follow-up: 292.6 ± 306.8 days. All three deaths were due to neurologic complications. MCS should be considered in patients with fulminant myocarditis complicated by shock. With aggressive medical therapy, early utilization of MCS carries promising outcomes.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Background
Myocarditis is an inflammatory condition affecting the myocardial muscle [1]. It is most commonly viral in origin, though autoimmune and nonspecific etiologies have also been reported. Its presentation varies from nonspecific constitutional symptoms to dyspnea in 71.7 %, chest pain in 31.9 %, and arrhythmic events in 17.9 % of patients [2]. Myocarditis is a known cause of dilated cardiomyopathy, particularly in young adults, and is cited as the etiology of heart failure in 9–10 % of patients in large prospective series [3,4]. Historically, myocarditis has been found in 8.6–12 % of post-mortem cases secondary to sudden cardiac death in young adults [5,6]. The Myocarditis Treatment Trial, which is one of the largest trials studying this cohort of patients, reports a 1-year mortality of 20 and a 56 % mortality at 4.3-years [7]. Patients may develop acute fulminant myocarditis with rapidly progressive circulatory collapse that is resistant to aggressive medical therapy and results in multi-organ system failure and in some cases death [8]. Of the patients that survive, a considerable percentage of patients are left with severe dilated cardiomyopathy and may ultimately require heart replacement therapy [7,9,10]. In patients with acute fulminant myocarditis, there is evidence that early utilization of MCS may prevent the development of irreversible cardiomyopathy, particularly in combination with appropriate medical therapy and neurohormonal blockade [11–14]. In this case series, we sought to examine the outcomes of patients with acute fulminant myocarditis who deteriorate due to cardiogenic shock and required acute mechanical circulatory support.
Methods
A retrospective review was conducted of all patients with cardiogenic shock treated with mechanical circulatory support (MCS) from 01 January 2007 to 30 June 2013 at our institution. All patients diagnosed with myocarditis or myopericarditis were enrolled to this analysis.
Diagnosis was based on either histopathological, clinical or the combination of both:
-
(1)
Histopathological evidence for active myocarditis as defined by [1]
-
(2)
Clinical diagnosis based on the combination of the clinical picture with supporting laboratory testing and imaging [18].
-
(a)
severe hemodynamic compromise requiring high-dose vasopressors or MCS [19]
-
(b)
an advanced heart failure syndrome or newly diagnosed dilated cardiomyopathy with global left ventricular dysfunction and/or a dilated left ventricular end-diastolic dimension greater than 4 cm [11,20]
-
(c)
elevated troponin levels [21]
-
(d)
electrocardiogram with ST elevations in non-coronary distributions, T wave inversions, or Q waves despite normal or non-obstructive coronary arteries [21]
-
(a)
Patients either received veno-arterial extracorporeal membrane oxygenator (VA ECMO) or the continuous flow Centrimag biventricular assist device (BIVAD; Thoratec, Pleasanton, CA, USA). Data was collected and analysis using Excel software (2007 Microsoft Corp., Redmond, WA, USA). Categorical variables were summarized by means and standard deviations.
Results
Patients
Two hundred and sixty patients received MCS for acute cardiogenic shock from 01 January 2007 to 30 June 2013. Eleven patients met the criteria for diagnosis of active myocarditis and were enrolled in this analysis. The mean age at the time of device implantation was 48-years old (range, 23–71) and 9 out of the 11 patients were male. A summary of the baseline characteristic is described in Table 1. Nine patients specifically fulfilled the histopathologic definition as confirmed by myocardial biopsy. Of the two patients without myocardial biopsy, one fulfilled the clinical definition of myocarditis with serology-proven mycoplasma myocarditis, and the other patient had clinical myopericarditis with an electrocardiogram demonstrating diffuse ST segment elevation and PR depressions and myocardial involvement exhibited by a peak troponin of 19 ng/mL. Five of the 11 patients had a combined myocardial and pericardial process, while six patients had an isolated myocardial process.
Severity of Patients
Only 1 patient was directly admitted to our center, while the other ten patients were transferred from community hospitals due to refractory shock for advanced heart failure management (mean 1.60 ± 1.42 days).
Overall, 8 of the 11 patients were treated with an intra-aortic balloon pump (IABP) prior to MCS support. Four out of the 10 transferred patients were already supported with an IABP upon arrival and four more received an IABP upon arrival to our center. One patient was transferred due to persistent right heart failure despite Tandem Heart BIVAD support.
The mean time from presentation to the emergency department to the onset of cardiogenic shock was 1.45 ± 1.44 days. Nine of the 11 patients were already in cardiogenic shock by the time they presented to our center. Vasoactive medications were also utilized, and two patients were treated with inotropes alone, while six patients were treated with a combination of inotropes and pressors, though one of the six patients had refractory arrhythmia resulting in early discontinuation of inotropes. Prior to MCS implantation all of the patients were in severe cardiogenic shock as defined by a low cardiac index (less than 2 L/min/m2), end-organ dysfunction (renal or liver dysfunction), and/or severe hypotension, with a systolic blood pressure of less that 80–90 mmHg or a mean arterial pressure that is 30 mmHg less than baseline. A summary of all of the patients' hemodynamics and the end-organ function prior to device implantation is presented in Table 2. Two patients developed acute anuric renal failure and required renal replacement therapy prior to MCS, while another patient developed renal failure and required renal replacement therapy post-operatively. Three patients had evidence of shock liver with aspartate aminotransferase (AST) and alanine aminotransferase (ALT) peaking at 783 and 6,331 U/L, respectively.
Transthoracic echocardiography demonstrated severe left ventricular dysfunction in ten patients with mean ejection fraction of 22 ± 14 %. One patient had severe myopericarditis-induced cardiogenic shock (with tamponade physiology) and initially had a preserved biventricular function, which deteriorated following pericardiocentesis.
Mechanical Circulatory Support Type and Outcome
The mean time from onset of shock to MCS implantation was 10.9 ± 11.7 h. Eight patients received the Centrimag BIVAD, and three patients received VA ECMO. One patient was supported with VA ECMO for 38 h, but due to worsening shock, required transition to Centrimag BIVAD. All Centrimag BIVADs were centrally cannulated with the following LVAD configurations: four out of eight with left ventricle to aorta cannulation, two out of eight left atrium to aorta cannulation, and two out of eight left atrium and left ventricle to aorta cannulation (Y-shape cannulation; Fig. 1). The RVAD was cannulated right atrium to pulmonary artery in all but one patient, who was cannulated right ventricle to pulmonary artery. All Centrimag-supported patients had a core biopsy taken from the left ventricular apex during the device implantation. None of the patients experienced cannula dislodgment despite undergoing device implantation during active inflammation.
VA ECMO was implanted at bedside with a peripheral cannulation strategy in all three patients due to rapidly deteriorating shock. Venous cannulation was via the femoral vein and arterial cannulation was via the femoral artery. In all cases, the IABP was removed shortly after VA ECMO implantation. No preventive vent technique was utilized acutely, and none of the patients required subsequent implantation of a decompression device, such as an Impella (Abiomed, Danvers, MA, USA). One patient, as previously described, was transition from VA ECMO to Centrimag BIVAD due to persistent shock, LV dilatation, and RV failure.
During the period on mechanical support, 7 out of the 11 patients were initially on inotropes, which were weaned in an average of 2.8 ± 2.9 days. The patients with Centrimag BIVAD support had a mean support time of 14.7 ± 4.4 days, and two patients were transitioned from Centrimag BIVAD to a long-term HeartMate II left ventricular assist device (LVAD; Thoratec, Pleasanton, CA, USA). The patients receiving VA ECMO were supported for only 7.0 ± 1.4 days.
During acute device support, all 11 patients were treated with Heparin with a goal activated partial thromboplastin time (aPTT) of 60–80 s. The two patients that were transitioned to long-term LVADs were bridged with heparin during the acute phase and then were maintained on Aspirin 81 mg and Warfarin with a goal international normalized ratio (INR) of 2–2.5. All patients received multiple blood products during the operative room and post-operative period with the mean transfusion requirements as follows: packed red blood cells 9.5 ± 9.3 units, platelets 8.1 ± 13.7 units, fresh frozen plasma 5.9 ± 6.3 units, and cryopercipitate 2.3 ± 4.2 units.
Myocarditis Pathology and Treatment During Support
Nine out of the 11 patients had biopsy-proven acute myocarditis, and all nine had core biopsies taken during Centrimag BIVAD placement (Fig. 2). Four patients had acute inflammatory myocarditis, two had fulminant lymphocytic myocarditis, one had giant cell myocarditis (GCM), one had Churg-Strauss eosinophilic myocarditis (CS), and one had nonspecific acute myocardial inflammation. The two patients who received VA ECMO did not have tissue diagnosis due to hemodynamic instability which prevented their transfer to the catheterization lab for biopsy.
Utilization of immunosuppressive therapies varied primarily based on the tissue diagnosis and clinical status of the patients. Five patients in our series received empiric methylprednisonolone due to rapidly deteriorating shock. Two of these patients had tissue diagnosis of autoimmune myocarditis and received an extensive course of steroids but did not demonstrate myocardial recovery (GCM and CS) and were listed for heart transplantation. The remaining three patients (two with lymphocytic myocarditis and one with mononuclear cell myocarditis) recovered their left ventricular (LV) function despite only an abbreviated steroid course. Cyclophosphamide therapy was only administered to the patient with GCM, but as mentioned, this patient did not recover.
Nine patients were started on neurohormonal blockade during MCS. Six patients received beta-blockers during their time on acute support, with a mean dose of metoprolol of 125 mg/day (ranging from metoprolol 12.5 mg every 12 h to 50 mg every 6 h) and a mean dose of carvedilol of 37.3 mg/day (ranging from carvedilol 3.125 mg every 12 h to 31.25 mg every 12 h). Beta-blockers were initiated an average of 4 days post-MCS implantation and peak dose was reached at 8 days post MCS implantation. Patient received an average of 13 days of beta-blocker therapy prior to explantation of the acute MCS device. Three patients were started on Angiotensin Converting Enzyme inhibitors (ACE inhibitors), and no patients were treated with angiotensin receptor blockers (ARBs) during acute support. The typical starting agent was captopril with mean dose of 34 mg/day (ranging from captopril 6.25 mg every 8 h to 18.75 mg every 8 h) and one patient was transitioned to lisinopril with mean dose of 15 mg/day. Four patients were treated with aldosterone antagonists, with the most common agent spironolactone 25 mg daily. Reasons for not starting these medications were hypotension in the case of beta-blockers and ACE inhibitors, and hyperkalemia or renal failure in the case of ACE inhibitors and aldosterone antagonists. Three out of the nine patients received all three agents (beta-blockers, ace inhibitors/ARBs, and aldosterone antagonists), and all three of these patients had reasonable recovery of their cardiac function.
At 90-days following acute device explantation, eight patients were on a stable dose of beta-blocker, with four patients on carvedilol (6.25 mg twice daily to 25 mg twice daily, mean dose 15 mg twice daily) and four patients on metoprolol (ranging from metoprolol tartrate 25 mg twice daily to metoprolol succinate 50 mg daily, mean dose of 70 mg/day). Three patients were on lisinopril 5 mg daily, and four patients were on spironolactone 25 mg daily at 90-days post explantation.
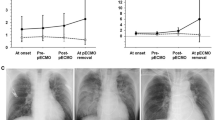
Outcome
Of the 11 patients in this series, eight patients survived to hospital discharge following acute myocarditis complicated cardiogenic shock (seven Centrimag BIVAD and one VA ECMO; Fig. 3). Three patients died, and all deaths were secondary to neurologic complications. Among the patients that died, two suffered anoxic brain injury prior to support implantation, and only one patient died secondary to a complication that occurred during BIVAD support. This patient (GCM) had a hemorrhagic stroke while waiting for heart transplantation supported with the Centrimag BIVAD for 15 days. His aPTT had been stable within the therapeutic range of 60–80 s during the days leading up to the event, but he was noted to have a LV apical thrombus on an echocardiogram days prior to the event. The patient eventually died due to brain stem herniation. Of note, this patient had the “Y-shaped” left atrial and ventricular cannulation, and the apical thrombus formed on the LV apical cannula. The other patient who had similar cannulation also was noted to have an apical thrombus upon echocardiographic imaging prior to device explantation but had no clinically significant thromboembolic sequelae.
Eight of the 11 patients recovered their cardiac function, with a mean left ventricular ejection fraction of 53.2 % and normal right ventricular function. All of the recovered patients (seven Centrimag and one VA ECMO) were successfully decannulated and explanted. One of the Centrimag-supported patients, despite full myocardial recovery suffered irreversible anoxic brain injury prior to Centrimag BIVAD implantation and the family withdrew supportive respiratory care several days after the device was explanted. Both patients that had transitioned to HeartMate II LVAD were successfully explanted, one at 55 days and the other at 112 days following LVAD implantation.
Mean follow-up in the surviving patients was 292.6 ± 306.8 days. Seven of the eight recovered patients were alive without heart failure symptoms and a mean EF was 54 ± 7 % (range 45–60 %). The patient that survived without recovery was successfully transplanted and was doing well 8 months post-transplantation (Fig. 3).
Discussion
In this paper, we report our experience with MCS as a treatment for fulminant myocarditis complicated by acute cardiogenic shock. Eight of the 11 patients survived to discharge from the hospital, and of these, seven had recovered LV function while one patient was bridged to successful heart transplantation. In our case series, both VA ECMO as well as Centrimag BIVAD served as options for hemodynamic stabilization, though Centrimag was used in a majority of cases (82 %). We did not observe any cannula-related complications during the time on MCS despite implantation during a time of acute, active inflammation. Myocarditis complicated by acute cardiogenic shock can be supported with MCS with excellent outcomes and a high rate of myocardial recovery.
MCS has become the cornerstone of treatment for cardiogenic shock regardless of the etiology. Evidence is mounting that the early utilization of MCS results in improved outcomes in patients with cardiogenic shock from multiple etiologies, including, but not limited to myocardial infarction, non-ischemic cardiomyopathy, and arrhythmia. Over time, device technology has improved, and several different MCS devices are being approved to treat the “crash and burn” INTERMACS 1 profile patients. When considering mechanical support for a patient in cardiogenic shock, multiple factors must be considered. First, does the patient need emergent bedside support or is there time for transfer to the operating room? Secondly, does the patient need biventricular support, supported by signs consistent with significant right heart failure including elevated central venous pressure out of proportion to left-sided filling pressures, liver congestion/failure and inadequate LV filling? Thirdly, is long-term support anticipated based on the patients clinical situation?
Overall acute MCS devices can be divided into two groups based on implantation: (1) percutaneous MCS and (2) surgical MCS, though some devices have the advantage of being implanted by both techniques. Among the device options are Tandem Heart (CardiacAssist Inc, Pittsburg, PA, USA), Impella 3.5 (Abiomed, Danvers, MA, USA), Veno-arterial Extra Corporeal Membrane Oxygenation (VA ECMO) or Centrimag Ventricular Assist Device (BIVAD; Thoratec, Pleasanton, CA, USA) (Table 3). In our experience, the majority of the patients had biventricular involvement and required biventricular support. When hemodynamics permitted, our device of choice was the surgically implanted Centrimag BIVAD. Recently, our group has reported favorable outcomes in the patients supported with the Centrimag BIVAD for cardiogenic shock from various etiologies [22]. Here, we further demonstrate it within the fulminant myocarditis population. Seven of the nine patients supported with the Centrimag BIVAD survived to be discharge from the hospital, and six of them had full myocardial recovery. Currently, the Centrimag BIVAD can be used only for a short to intermediate support time, but in patients that would require prolonged MCS, transition to a long-term LVAD is technically feasible, safe, and does not carry increased mortality [23]. In the current case series, two patients required prolonged support and both were successfully transition to HeartMate II LVAD with an uncomplicated post-operative course. Both patients recovered their left ventricular function and were successfully explanted.
In the patients too unstable for transfer to the operating room, VA ECMO has proved to be a relatively fast and durable strategy to stabilize these patients and bridge them until cardiac recovery, transfer to a tertiary center or transition to the next level of support [24,25]. In our case series, no patients were transferred on VA ECMO, and three patients underwent implantation with peripheral cannulation at bedside due to acute hemodynamic instability.
While the expected outcome for patients with myocarditis differ based on the etiology, one should determine whether the patient will require only short-term support or will likely need bridging with a longer-term device. Fulminant viral myocarditis and hemodynamic compromise at presentation are associated with excellent recovery if early, aggressive intervention with medications and mechanical circulatory support is initiated [11]. As we saw in our patient cohort, 8 of the 11 patients with acute fulminant myocarditis had recovery of biventricular function, and seven of them survived to be discharged home without advanced heart failure therapy. Preserved ejection fraction [26], smaller left ventricular end-diastolic (LVEDD) and left atrial dimensions [27] are associated with a higher likelihood of spontaneous recovery. In our cohort, the two patients with fulminant lymphocytic myocarditis had both preserved left ventricular and left atrial dimensions and both patients recovered. Only two patients had dilated LVEDD (the CS and mycoplasma myocarditis) and those two patients did not recover.
While immunosuppression was not used in a majority of cases, the role for immunosuppressant use in acute myocarditis continues to remain unclear. Several reports demonstrate that immunosuppression may be beneficial in the treatment of myocarditis, particularly in cases of autoimmune myocarditis. The Giant Cell Myocarditis Study Group Investigators showed that the use of corticosteroids with cyclosporine, azathioprine, or both was associated with a 12.3-month mean survival as compared to 3 months in the no immunosuppression group [28]. In cases of inflammatory myocarditis with no obvious pathogen or autoimmune process, the results are more controversial. The TIMIC group showed improvement in left ventricular function in 88 % of patients treated with prednisone and azathioprine who had virus negative inflammatory cardiomyopathy [29]. The Myocarditis Treatment Trial, on the other hand, did not differentiate the etiology of myocarditis in the treatment arm and only showed a slight improvement in ejection fraction in patients with active myocarditis who were treated with cyclosporine, azathioprine, and prednisolone as compared to placebo [7]. Maisch et al. demonstrate that in the literature, the results of immunosuppression in myocarditis trials are mixed, though many of these studies do not differentiate the etiology of myocarditis [30]. These studies underscore the importance of identifying the etiology of myocarditis prior to considering immunosuppression. Five patients in our series received empiric steroids due to rapidly deteriorating shock. Of these patients, two had biopsy-proven autoimmune myocarditis (Giant cell and Churg Strauss) and did not recover their cardiac function despite immunosuppression. The other three patients received empiric steroids that were discontinued once the biopsy results showed inflammatory cells. When suspecting an autoimmune process, particularly giant cell, early immunosuppressive therapy should be given due to the rapidly progressive deterioration in clinical status associated with giant cell myocarditis and the observed improvement in survival with treatment, though some of these patients may require long-term MCS or heart transplantation within 1 year [31,32].
Early utilization and tolerance of neurohormonal blockade during MCS therapy are critical in patients with acute fulminant myocarditis and are associated with improved outcomes [33,34]. In our case series, 6 of the 11 patients were treated with neurohormaonal blockade during the device support period to augment the chance of recovery [33,35–41], while five more patients were treated with neurohormonal blockade after successful device explantation. There is mounting evidence demonstrating profound vasodilatory shock following cardiopulmonary bypass in patients treated with ACE inhibitors pre-operatively [42]. As a result, the clinical practice in our center is to initiate beta-blockade followed by aldosterone antagonists pre-operatively and to introduce ACE inhibitors or ARB's only after device explantation, and once renal function has stabilized.
Patients with acute fulminant myocarditis tend to be younger with minimal co-morbidities at the time of presentation. Early identification of the underlying process and early intervention with aggressive medical supportive care and the appropriate utilization of MCS can result in excellent outcomes for patients with myocarditis. The promising outcomes in our case series reinforce the importance of aggressive early intervention in this patient population.
Limitations
The main limitations of this study include its retrospective design and small sample size, as well as the fact that it reflects only a single center's experience. The patients in this study are primarily transferred to our tertiary care center for advanced therapy and thus are a select group of patients.
Conclusions
The early utilization of MCS should be considered in patients with fulminant myocarditis complicated by acute cardiogenic shock as a first-line therapy. The combination of aggressive medical therapy including inotropes, neurohormonal blockade, and when appropriate, immunosuppression with MCS carry a high chance of survival to myocardial recovery or survival to the next stage of treatment.
References
Richardson, P., McKenna, W., Bristow, M., Maisch, B., Mautner, B., O'Connell, J., Olsen, E., Thiene, G., Goodwin, J., Gyarfas, I., Martin, I., & Nordet, P. (1996). Report of the 1995 world health organization/international society and federation of cardiology task force on the definition and classification of cardiomyopathies. Circulation, 93, 841–842.
Hufnagel, G., Pankuweit, S., Richter, A., Schonian, U., & Maisch, B. (2000). The european study of epidemiology and treatment of cardiac inflammatory diseases (esetcid). First epidemiological results. Herz, 25, 279–285.
Felker, G. M., Hu, W., Hare, J. M., Hruban, R. H., Baughman, K. L., & Kasper, E. K. (1999). The spectrum of dilated cardiomyopathy. The johns hopkins experience with 1,278 patients. Medicine, 78, 270–283.
Hahn, E. A., Hartz, V. L., Moon, T. E., O'Connell, J. B., Herskowitz, A., McManus, B. M., & Mason, J. W. (1995). The myocarditis treatment trial: design, methods and patients enrollment. European Heart Journal, 16(Suppl O), 162–167.
Fabre, A., & Sheppard, M. N. (2006). Sudden adult death syndrome and other non-ischaemic causes of sudden cardiac death. Heart, 92, 316–320.
Doolan, A., Langlois, N., & Semsarian, C. (2004). Causes of sudden cardiac death in young australians. The Medical Journal of Australia, 180, 110–112.
Mason, J. W., O'Connell, J. B., Herskowitz, A., Rose, N. R., McManus, B. M., Billingham, M. E., & Moon, T. E. (1995). A clinical trial of immunosuppressive therapy for myocarditis. The myocarditis treatment trial investigators. The New England Journal of Medicine, 333, 269–275.
Grogan, M., Redfield, M. M., Bailey, K. R., Reeder, G. S., Gersh, B. J., Edwards, W. D., & Rodeheffer, R. J. (1995). Long-term outcome of patients with biopsy-proved myocarditis: comparison with idiopathic dilated cardiomyopathy. Journal of the American College of Cardiology, 26, 80–84.
Cooper, L. T., Jr. (2009). Myocarditis. The New England Journal of Medicine, 360, 1526–1538.
Maron, B. J., Doerer, J. J., Haas, T. S., Tierney, D. M., & Mueller, F. O. (2009). Sudden deaths in young competitive athletes: analysis of 1866 deaths in the united states, 1980-2006. Circulation, 119, 1085–1092.
McCarthy, R. E., 3rd, Boehmer, J. P., Hruban, R. H., Hutchins, G. M., Kasper, E. K., Hare, J. M., & Baughman, K. L. (2000). Long-term outcome of fulminant myocarditis as compared with acute (nonfulminant) myocarditis. The New England Journal of Medicine, 342, 690–695.
Acker, M. A. (2001). Mechanical circulatory support for patients with acute-fulminant myocarditis. The Annals of Thoracic Surgery, 71, S73–76. discussion S82-75.
Ginsberg, F., & Parrillo, J. E. (2013). Fulminant myocarditis. Critical Care Clinics, 29, 465–483.
Mirabel, M., Luyt, C. E., Leprince, P., Trouillet, J. L., Leger, P., Pavie, A., Chastre, J., & Combes, A. (2011). Outcomes, long-term quality of life, and psychologic assessment of fulminant myocarditis patients rescued by mechanical circulatory support. Critical Care Medicine, 39, 1029–1035.
Aretz, H. T. (1987). Myocarditis: the dallas criteria. Human Pathology, 18, 619–624.
Herskowitz, A., Ahmed-Ansari, A., Neumann, D. A., Beschorner, W. E., Rose, N. R., Soule, L. M., Burek, C. L., Sell, K. W., & Baughman, K. L. (1990). Induction of major histocompatibility complex antigens within the myocardium of patients with active myocarditis: a nonhistologic marker of myocarditis. Journal of the American College of Cardiology, 15, 624–632.
Maisch, B., Portig, I., Ristic, A., Hufnagel, G., & Pankuweit, S. (2000). Definition of inflammatory cardiomyopathy (myocarditis): on the way to consensus. A status report. Herz, 25, 200–209.
Elamm, C., Fairweather, D., & Cooper, L. T. (2012). Pathogenesis and diagnosis of myocarditis. Heart, 98, 835–840.
Lieberman, E. B., Hutchins, G. M., Herskowitz, A., Rose, N. R., & Baughman, K. L. (1991). Clinicopathologic description of myocarditis. Journal of the American College of Cardiology, 18, 1617–1626.
Dec, G. W., Jr., Palacios, I. F., Fallon, J. T., Aretz, H. T., Mills, J., Lee, D. C., & Johnson, R. A. (1985). Active myocarditis in the spectrum of acute dilated cardiomyopathies. Clinical features, histologic correlates, and clinical outcome. The New England Journal of Medicine, 312, 885–890.
Dec, G. W., Jr., Waldman, H., Southern, J., Fallon, J. T., Hutter, A. M., Jr., & Palacios, I. (1992). Viral myocarditis mimicking acute myocardial infarction. Journal of the American College of Cardiology, 20, 85–89.
Ota, T., Yerebakan, H., Akashi, H., Takayama, H., Uriel, N., Colombo, P. C., Jorde, U. P., Naka, Y. (2013). Continuous-flow left ventricular assist device exchange: clinical outcomes. The Journal of Heart and Lung Transplantation. doi:10.1016/j.healun.2013.07.003.
Gonzalez-Costello, J., Yang, J., Sims, D. B., Kossar, A. P., Murray, L. K., Colombo, P. C., Takayama, H., Mancini, D., Naka, Y., Jorde, U. P., & Uriel, N. (2012). Bridging cardiogenic shock patients with short-term ventricular support at a community hospital to long-term ventricular support at a tertiary hospital. The Journal of Heart and Lung Transplantation: The Official Publication of the International Society for Heart Transplantation, 31, 618–624.
Javidfar, J., Brodie, D., Takayama, H., Mongero, L., Zwischenberger, J., Sonett, J., & Bacchetta, M. (2011). Safe transport of critically ill adult patients on extracorporeal membrane oxygenation support to a regional extracorporeal membrane oxygenation center. ASAIO Journal, 57, 421–425.
Beurtheret, S., Mordant, P., Paoletti, X., Marijon, E., Celermajer, D. S., Leger, P., Pavie, A., Combes, A., & Leprince, P. (2013). Emergency circulatory support in refractory cardiogenic shock patients in remote institutions: a pilot study (the cardiac-rescue program). European Heart Journal, 34, 112–120.
Blauwet, L. A., & Cooper, L. T. (2010). Myocarditis. Progress in Cardiovascular Diseases, 52, 274–288.
Bossone, E., Shea, M. J., Nicklas, J. M., Abrams, G. D., & Das, S. K. (2000). Early spontaneous recovery of left ventricular function in patients with myocarditis. Italian Heart Journal: Official Journal of the Italian Federation of Cardiology, 1, 758–761.
Cooper, L. T., Jr., Berry, G. J., & Shabetai, R. (1997). Idiopathic giant-cell myocarditis–natural history and treatment. Multicenter giant cell myocarditis study group investigators. The New England Journal of Medicine, 336, 1860–1866.
Frustaci, A., Russo, M. A., & Chimenti, C. (2009). Randomized study on the efficacy of immunosuppressive therapy in patients with virus-negative inflammatory cardiomyopathy: the timic study. European Heart Journal, 30, 1995–2002.
Maisch, B., Herzum, M., Hufnagel, G., Bethge, C., & Schonian, U. (1995). Immunosuppressive treatment for myocarditis and dilated cardiomyopathy. European Heart Journal, 16(Suppl O), 153–161.
Cooper, L. T., Jr. (2005). Giant cell and granulomatous myocarditis. Heart Failure Clinics, 1, 431–437.
Cooper, L. T., Jr., Hare, J. M., Tazelaar, H. D., Edwards, W. D., Starling, R. C., Deng, M. C., Menon, S., Mullen, G. M., Jaski, B., Bailey, K. R., Cunningham, M. W., & Dec, G. W. (2008). Giant cell myocarditis treatment trial I. Usefulness of immunosuppression for giant cell myocarditis. The American Journal of Cardiology, 102, 1535–1539.
Godsel, L. M., Leon, J. S., & Engman, D. M. (2003). Angiotensin converting enzyme inhibitors and angiotensin ii receptor antagonists in experimental myocarditis. Current Pharmaceutical Design, 9, 723–735.
Xiao, J., Shimada, M., Liu, W., Hu, D., & Matsumori, A. (2009). Anti-inflammatory effects of eplerenone on viral myocarditis. European Journal of Heart Failure, 11, 349–353.
Yuan, Z., Shioji, K., Kihara, Y., Takenaka, H., Onozawa, Y., & Kishimoto, C. (2004). Cardioprotective effects of carvedilol on acute autoimmune myocarditis: anti-inflammatory effects associated with antioxidant property. American Journal of Physiology. Heart and Circulatory Physiology, 286, H83–90.
Kindermann, I., Kindermann, M., Kandolf, R., Klingel, K., Bultmann, B., Muller, T., Lindinger, A., & Bohm, M. (2008). Predictors of outcome in patients with suspected myocarditis. Circulation, 118, 639–648.
Reyes, M. P., Khatib, R., Khatib, G., Ho, K. L., Smith, F., & Kloner, R. A. (1998). Prolonged captopril therapy in murine viral myocarditis. Journal of Cardiovascular Pharmacology and Therapeutics, 3, 43–50.
Bahk, T. J., Daniels, M. D., Leon, J. S., Wang, K., & Engman, D. M. (2008). Comparison of angiotensin converting enzyme inhibition and angiotensin ii receptor blockade for the prevention of experimental autoimmune myocarditis. International Journal of Cardiology, 125, 85–93.
Seko, Y. (2006). Effect of the angiotensin ii receptor blocker olmesartan on the development of murine acute myocarditis caused by coxsackievirus b3. Clinical Science, 110, 379–386.
Sukumaran, V., Watanabe, K., Veeraveedu, P. T., Ma, M., Gurusamy, N., Rajavel, V., Suzuki, K., Yamaguchi, K., Kodama, M., & Aizawa, Y. (2011). Telmisartan ameliorates experimental autoimmune myocarditis associated with inhibition of inflammation and oxidative stress. European Journal of Pharmacology, 652, 126–135.
Godsel, L. M., Leon, J. S., Wang, K., Fornek, J. L., Molteni, A., & Engman, D. M. (2003). Captopril prevents experimental autoimmune myocarditis. Journal of Immunology, 171, 346–352.
Mekontso-Dessap, A., Houel, R., Soustelle, C., Kirsch, M., Thebert, D., & Loisance, D. Y. (2001). Risk factors for post-cardiopulmonary bypass vasoplegia in patients with preserved left ventricular function. The Annals of Thoracic Surgery, 71, 1428–1432.
Author information
Authors and Affiliations
Corresponding author
Additional information
Associate Editor DeLisa Fairweather oversaw the review of this article
Rights and permissions
About this article
Cite this article
Mody, K.P., Takayama, H., Landes, E. et al. Acute Mechanical Circulatory Support for Fulminant Myocarditis Complicated by Cardiogenic Shock. J. of Cardiovasc. Trans. Res. 7, 156–164 (2014). https://doi.org/10.1007/s12265-013-9521-9
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12265-013-9521-9