Abstract
Marfan syndrome (MFS) is a systemic disorder of the connective tissue with pleiotropic manifestations due to heterozygous FBN1 mutations and consequent upregulation of TGFβ signaling in affected tissues. Myxomatous thickening and elongation of the mitral valve (MV) leaflets commonly occur in this condition. Investigation of murine models of this disease has led to improved understanding of the mechanisms that underlie many of the phenotypic features of MFS, including MV disease. Loeys–Dietz syndrome (LDS) is a related disorder due to heterozygous mutations in the genes encoding subunits of the TGFβ receptor, and it may also involve the MV leaflets with similar elongation and thickening of the MV leaflets. Although the genetic basis and pathogenesis of nonsyndromic MV prolapse has been elusive to date, insights derived from monogenic disorders like MFS and LDS can be informative with regard to novel gene discovery and investigation into the pathogenesis of MV disease. This manuscript will review the prevalence of MV disease in MFS, its pathogenic basis as determined in mice with Fbn1 mutations, and ongoing studies that seek to better understand MV disease in the context of fibrillin-1 deficiency or excessive TGFβ signaling.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Marfan syndrome (MFS) is a systemic disorder of the connective tissue principally characterized by its cardinal manifestations of long bone overgrowth, ocular lens dislocation, and aneurysm of the aortic root. Prior to the development of noninvasive cardiovascular imaging technologies, the earliest descriptions of MFS focused more on its skeletal features. Antoine Marfan first reported a single interesting child with striking skeletal features [1]. He later reported 150 additional cases, earning the eponym for this condition that remains in use today [2]. Following from early observations of a correlation between aortic aneurysm and arachnodactyly, McKusick elegantly outlined the cardiovascular features of MFS in 1955, well before the widespread use of modern echocardiographic imaging of the heart and aorta [3, 4]. In this report, aortic disease was the primary focus, but mitral valve (MV) thickening and insufficiency were well described. He noted that precordial systolic murmurs commonly occur in affected individuals, and he also highlighted the occurrence of endocarditis in people with MFS [4]. Bowers subsequently described six cases of primary MV disease in individuals diagnosed with MFS but who did not have substantial aortic regurgitation or left ventricular dilation that could secondarily lead to MV insufficiency [5]. She highlighted the presence of a “ground substance” in the MV leaflets that was similar in appearance to the myxoid degeneration of the aortic root in patients with MFS, speculating appropriately that the MV disease was due to the “expression of the inherent defect in the connective tissue in Marfan patients [5].”
MV Disease in Marfan Syndrome
MV prolapse is a criterion for the clinical diagnosis of MFS, and it is commonly seen in this condition, though not invariably so [6]. The recently revised Ghent criteria for the diagnosis of MFS emphasizes two cardinal features of this disorder, ectopia lentis (ocular lens dislocation) and aortic root aneurysm/dissection, and FBN1 mutation analysis while minimizing the impact of several less specific manifestations such as MV prolapse [6]. Although premature calcification of the mitral valve was considered a minor criterion for the diagnosis in the original Ghent criteria, it is no longer included [7]. The diagnosis of MFS should now be established with one of these four scenarios: (1) aortic root enlargement (Z score ≥2) and ectopia lentis, (2) aortic root enlargement (Z score ≥2) and a clear FBN1 mutation, (3) aortic root enlargement (Z score ≥2) and systemic features of MFS resulting in a score ≥7 points, or (4) ectopia lentis and an FBN1 mutation that is known to associate with typical aortic disease in MFS [6]. In the third of these four scenarios, MV disease contributes to the score for systemic features with the addition of one point. Other systemic features included in this category are the traditional skeletal manifestations of MFS, pneumothorax, dural ectasia, dermal striae, and severe myopia [6]. The diminished influence of MV disease in the diagnostic criteria for MFS is not a reflection of a lack of importance but rather of its lack of specificity for this condition.
The typical abnormality of the MV when it is affected in MFS involves redundant prolongation of one or both leaflets, often accompanied by myxomatous thickening with billowing in a pattern similar to Barlow's disease [8] (Fig. 1). A retrospective review and comparison of MV morphology at the time of MV surgery in MFS and myxomatous nonsyndromic MV disease reported that individuals with MFS presented at an earlier age (41 vs. 57 years, respectively; P ≤ 0.0001) and that the anterior MV leaflet was longer in MFS than in nonsyndromic MV disease (40 vs. 33 mm, respectively; P ≤ 0.0007) [9]. As with many phenotypic characteristics of MFS, the presence and severity of MV prolapse, thickening, and regurgitation often vary within families segregating the same FBN1 gene mutation [10, 11].
Several studies have reported disparate prevalence of MV prolapse among individuals with MFS. Pyeritz and Wappel reported in a cohort of 166 individuals with MFS that 52% had auscultatory evidence of MV insufficiency and 68% had echocardiographic evidence of MV abnormalities, primarily consisting of MV prolapse [12]. Chordal rupture was uncommon in this cohort [12]. More recently, Taub and colleagues reported their analysis of a cohort of 90 individuals with MFS, investigating the prevalence and spectrum of MV abnormalities [13]. Upon rigorous assessment by echocardiography, only 28% had MV prolapse, predominantly with bileaflet involvement and thickening. Within this cohort of individuals with MFS, the group with MV prolapse also had larger aortic root dimensions [13]. In contrast, a large international database of people with mutation-proven MFS reported the diagnosis of MV prolapse in 77% with mitral regurgitation in 61% [14]. Wide divergence in the reported prevalence of MV disease in these cohorts may be explained by small cohorts (in some cases) and by differences in the criteria used to assign the presence of MV disease. Taking this into consideration, the prevalence of at least mild MV pathology appears to be approximately 75% and the prevalence of more severe myxomatous MV thickening with prolapse appears closer to 25% among individuals with MFS.
Neonatal MFS is often complicated by severe MV prolapse and regurgitation. In one series of 22 infants diagnosed with MFS in the first 3 months of life, MV prolapse was present in 82%, and MV insufficiency was a major contributor to the poor prognosis in this subset [15]. Sisk and colleagues described 15 consecutive infants and children who were diagnosed with MFS prior to age 4 years. In this cohort, all had aortic root enlargement, but mitral regurgitation was the leading cause of morbidity [16]. Investigators with the Universal Marfan Database reported an inverse correlation between age of onset in children with MFS and prevalence of MV prolapse [17]. Among 320 children diagnosed with MFS at age <18 years, the prevalence of MV prolapse was 73% among those classified as having neonatal MFS (diagnosed prior to age 4 weeks), 62% among those diagnosed between age 4 weeks and 10 years, and 59% among those diagnosed between 10 and 18 years of age [17].
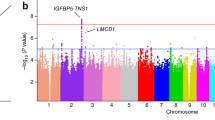
The prevalence of MV disease in MFS should be considered in the context of its prevalence among healthy control populations. The fifth examination of the offspring cohort of the Framingham Heart Study included 3,491 participants, all of whom were assessed for MV prolapse [18]. Classic MV prolapse was defined as superior displacement of the mitral leaflets of greater than 2 mm during systole with maximal leaflet thickness of at least 5 mm, and nonclassic prolapse was defined as displacement of more than 2 mm during systole, with a maximal thickness of less than 5 mm. In this cohort, 1.3% had classic prolapse and 1.1% had nonclassic prolapse [18]. While earlier publications suggested that MV prolapse occurs more frequently in healthy controls, they did not appropriately account for the three-dimensional structure of the valve and its annulus [19]. MV prolapse occurs in a familial pattern, but definitive recognition of its genetic basis has been elusive. To date, standard linkage analyses have reported three chromosomal loci linked to nonsyndromic familial MV prolapse, chromosome 16p12.1-p11.2, chromosome 11p15.4, and chromosome 13q31.3-q32.1 [20–22]. Recognition of the genes in which mutations occur in these loci should lead to improved understanding of the complex pathogenesis of MV disease.
Increased TGFβ Signaling in Marfan Syndrome
Although some disease manifestations in MFS, such as ocular lens dislocation, may be readily explained by a reduction or dysfunction of a structural protein, myxomatous thickening and prolongation of the MV are less readily attributable to a structural deficiency due to FBN1 mutation. The striking similarity of fibrillin-1 with the latent TGFβ-binding proteins (LTBPs) initially suggested the possibility that fibrillin-1 binds to the large latent complex of TGFβ. The TGFβ isoforms are expressed and synthesized intracellularly as large precursors that are cleaved into mature TGFβ and propeptide complexes, called “small latent complexes” [23]. Prior to secretion, TGFβ is covalently bound to the LTBPs, forming a “large latent complex” (LLC). Upon secretion, the LLC covalently links to the extracellular matrix, sequestering TGFβ [23]. Both fibrillin-1 and fibronectin have been shown to bind LTBP-1 and the LLC [24, 25].
We hypothesized that elongation and thickening of the MV leaflets could be caused by increased activation and signaling of TGFβ. Both heterozygous and homozygous mice with a fully expressed missense mutation in Fbn1 were compared to wild-type mice. Those with a missense mutation in Fbn1 had previously been shown to have many phenotypic features of MFS [26]. MV length and thickness were increased by postnatal day 6.5 in the heterozygous mice compared to wild-type mice, and they were also increased in the homozygous mice compared to the heterozygous Fbn1 mutant mice [27]. Adult heterozygous mutant mice were shown to have MV prolapse by high-resolution echocardiography [27]. These findings correlate with increased cellular proliferation and decreased apoptosis consistent with changes associated with myxomatous degeneration, as well as increased expression of TGFβ-responsive genes including regulators of matrix content and remodeling (collagens, Timp1) [27]. Treatment with a TGFβ-neutralizing antibody successfully normalized both the length and the thickness of the MV leaflets in the mutant mice, further supporting that the valve abnormalities were caused by increased TGFβ [27]. Similar increases in the activation and signaling of TGFβ have also been demonstrated in mice with Fbn1 mutations in the pulmonary alveoli, aortic root, skeletal muscle, and spinal dura [28–31].
The responsiveness of the MV length and thickness to excess TGFβ has implications for the identification of novel genes in which mutations may lead to MV disease. Furthermore, these results have raised the possibility that MV disease could be treated with therapies that reduce TGFβ. Although treatment with TGFβ-neutralizing antibodies successfully improves many phenotypic manifestations of MFS in mice, this therapy cannot be readily translated to treatment of human disease in the absence of FDA-approved humanized antibodies that block TGFβ. Because of extensive interaction between angiotensin II and TGFβ signaling, mice with Fbn1 mutation were treated with losartan, a selective angiotensin II type 1 receptor (AT1) antagonist, in an attempt to diminish TGFβ signaling [29, 32]. Remarkably, those mutant mice treated with losartan had dramatic improvement in their rate of aortic root growth compared to mutant mice treated with beta-adrenergic receptor blockers in doses with similar hemodynamic effects, and treatment effects correlated nicely with direct evidence for attenuated TGFβ signaling in the aortic media [29]. Marked phenotypic improvements are also evident with losartan treatment in nonhemodynamic tissues, such as pulmonary alveoli and skeletal muscle [29, 30]. Studies are ongoing now in both murine models of disease and in people with MFS to assess such treatments for their ability to improve aortic disease as well as MV prolapse and regurgitation [33].
Importance of the Angiotensin II Type 2 Receptor
The remarkable ability of selective AT1 receptor blockade in mice with an Fbn1 mutation to normalize aortic root growth and aortic wall architecture, to improve alveolar septation, and to restore skeletal muscle regeneration has led to further studies to identify the critical pathophysiologic processes that contribute to these manifestations of MFS, many of which are highlighted in Fig. 2. Today, at least three categories of medications are available to diminish angiotensin II signaling through the AT1 receptor. Angiotensin-converting enzyme (ACE) inhibitors block the conversion of the inactive angiotensin I to its active form (angiotensin II), thereby decreasing any interaction of this ligand with both the AT1 and the angiotensin II type 2 receptor (AT2) receptors [34]. Direct renin inhibitors have recently been developed, and they also decrease angiotensin II production [35]. Only the selective AT1 blockers permit ongoing stimulation of the AT2 receptor. AT1 receptor blockers were initially developed with the expectation that they would be better than ACE inhibitors, but studies of kidney dysfunction and heart failure have failed to show a benefit of AT1 blockers over ACE inhibitors [36, 37]. Stimulation of the AT2 receptor has many potential therapeutic advantages in aortic tissue, such as decreasing proliferation of smooth muscle cells, decreasing fibrosis, and decreasing the production of metalloproteinases [32, 38, 39]. However, AT2 stimulation has also been shown to increase vascular smooth muscle cell (VSMC) apoptosis, and apoptotic VSMCs have been reported in late-stage aortic aneurysms [40, 41]. Because of persistent questions about the advantages and disadvantages of selective blockade of AT1 vs. ACE inhibitors in Marfan-associated aortic disease, murine studies were performed to address this question [42].
Mice without the AT2 receptor are viable without cardiovascular malformations or a known vascular phenotype [43]. Mice without AT2 and with a heterozygous Fbn1 missense mutation not only have worsened aortic disease but also have decreased survival compared to mice with the Fbn1 mutation alone [42]. Treatment of Fbn1 mutant mice with a dose of enalapril (an ACE inhibitor) with nearly an identical hemodynamic effect as losartan resulted in only a modest reduction in the rate of aortic root growth, far less than that achieved by treatment with losartan. Furthermore, aortic root architecture was preserved far better by losartan than by enalapril in these Fbn1 mutant mice [42].
Analysis of the mechanism of worsened aortic disease and survival in mice with both an Fbn1 mutation and absence of the AT2 receptor compared to those with the Fbn1 mutation and with a normal AT2 receptor led to the discovery of augmented phosphorylation of the extracellular signal-regulated kinases 1 and 2 (ERK1/2) in mice without the AT2 receptor [42]. Since diseased tissue in mice with an Fbn1 mutation has both increased TGFβ and increased phosphorylation of ERK1/2 (pERK1/2), studies were performed to selectively decrease pERK1/2. We demonstrated that pERK1/2 is a principal effector of disease in fibrillin-1-deficient mice and that the stimulation of the AT2 receptor improves aortic disease by decreasing ERK1/2 activation [42]. Ongoing investigation of this murine model of MFS will include assessment of MV disease in relation to both phosphorylation of ERK1/2 and the role of AT2 in the pathogenesis of MV disease. The MAPK/ERK pathway has previously been implicated in valvular interstitial cell (VIC) calcification, conversion of VICs from a synthetic to a contractile phenotype, and to serotonin-induced valve fibrosis [44, 45].
MV Disease in Related Disorders
Loeys–Dietz syndrome (LDS) closely parallels many features of MFS though several important additional characteristics also occur [46]. LDS typically involves marked arterial tortuosity and distinct craniofacial abnormalities such as hypertelorism (widely spaced eyes), and cleft palate or a uvula that is bifid or broad based. One study reported that 4/14 (29%) individuals with LDS had prolapse of the MV [46]. As in MFS, malar hypoplasia, long bone overgrowth, pectus deformity of the chest, scoliosis, and joint laxity are commonly seen in LDS. In contrast, LDS often shows bluish discoloration of the ocular sclerae, craniosynostosis, and atrial septal defects, which are not associated with MFS [46]. In addition to those with typical LDS (type I), a second category of LDS that closely mimics vascular Ehlers–Danlos syndrome (vEDS) has been classified as LDS type II [47]. These individuals have aortic enlargement, visceral rupture, easy bruising, wide and atrophic scars, joint laxity, and/or velvety skin in the absence of craniofacial features of LDS type I, though isolated bifid uvula does not exclude the diagnosis of LDS type II [47].
Both presentations of LDS are caused by heterozygous mutations in either TGFBR1 or TGFBR2, genes encoding subunits of the TGFβ receptor [46]. These mutations are typically missense alterations of highly conserved amino acids in the kinase domains of the encoded receptor. Despite initial suspicions that these mutations would decrease activity of the TGFβ receptor by disruption of the kinase domain, immunostaining of diseased tissues from affected individuals shows evidence of increased TGFβ activity, such as increased nuclear accumulation of phosphorylated Smad2 and increased connective tissue growth factor, which is induced by TGFβ [46].
Because an individual with LDS may meet phenotypic criteria for MFS and because LDS is associated with aortic dissection at smaller aortic root diameter and shortened survival, one must look for phenotypic features of LDS among individuals who are considered to have MFS. For individuals whose diagnosis could be either MFS or LDS, molecular genetic testing for mutation in FBN1, TGFBR1, and TGFBR2 should be considered, along with clinical genetic counseling. Similarly, among individuals who could have either vEDS or LDS type II, a molecular diagnosis should be strongly considered, either through collagen studies on cultured dermal fibroblasts or molecular genetic testing, since LDS type II patients seem to have better surgical outcomes and improved rates of survival compared to vEDS patients [47].
The prevalence of MV disease appears to be greater in MFS than in LDS, although variability in the criteria used for MV prolapse and regurgitation may contribute to these differences. One group reported direct comparison of 71 individuals with TGFBR2 mutations, 243 with FBN1 mutations, and 50 unaffected family members [48]. They found a substantially higher prevalence of both MV prolapse and regurgitation in the cohort with FBN1 mutations than with TGFBR2 mutations (45% and 56% vs. 21% and 35%, respectively) [48].
Recently, three unrelated Dutch families with a comparable disorder were reported to have inactivating heterozygous mutations in MADH3 encoding Smad3 [49]. This condition is characterized by aortic aneurysms with arterial tortuosity, craniofacial features similar to LDS, and early-onset osteoarthritis. It was given the eponym of “aneurysms–osteoarthritis syndrome” or AOS in this report [49]. Among the affected individuals, MV abnormalities were common and ranged from mild to severe; 10/22 (45%) had MV prolapse and 6/22 (27%) had MV regurgitation. The prevalence of MV abnormalities in this cohort was compared to published frequencies in LDS type I, LDS type II, and MFS [49]. Once again, analysis of the diseased tissue from affected individuals with MADH3 mutations showed evidence of increased TGFβ activity, including increased TGF-β1, increased nuclear accumulation of phosphorylated-Smad2 and Smad3, as well as increased connective tissue growth factor, which is induced by TGFβ signaling [49].
Summary
MV disease commonly occurs in MFS and similar monogenic disorders. Both human and murine studies of MV disease in the setting of fibrillin-1 mutations indicate that a genetically induced reduction in extracellular matrix binding of latent TGFβ leads to localized increase in TGFβ activity, with consequent elongation and excessive thickening of the MV leaflets. MV prolapse and regurgitation also commonly occur in related conditions with increased TGFβ activity due to mutations in the TGFβ receptors or its downstream canonical signaling pathway. The variability of MV disease in these conditions, even within families who share the same mutation, indicates that additional genetic and environmental modifiers influence MV pathology. The response to TGFβ-neutralizing antibodies in Fbn1 mutant mice suggests that targeted treatments may be able to modulate pathologic growth of the MV. Ongoing studies of selective AT1 blockade will include analysis of MV regurgitation and its progression in response to losartan or atenolol, a beta blocker. Improved understanding of the pathogenesis of MV disease in MFS and similar conditions is likely to inform the search for genes with mutations resulting in nonsyndromic MV disease.
References
Marfan, A.-B. (1896). Un cas de deformation congenitale des quarte membres plus prononcee aux extremites caracterisee par l'allongement des os avec un certain degre d'amincissement. Bulletins et Mémoires de la Société Médicale des Hôpitaux de Paris, 13, 220–226.
Marfan, A.-B. (1938). La dolichosténomélie [dolichomélie arachnodactylie]. Annals of Medicine, 44, 5–29.
Baer, R. W., Taussig, H. B., & Oppenheimer, E. H. (1943). Congenital aneurysmal dilatation of the aorta associated with arachnodactyly. Bulletin of the Johns Hopkins Hospital, 72, 309–317.
McKusick, V. A. (1955). The cardiovascular aspects of Marfan's syndrome. Circulation, 11, 321.
Bowers, D. (1969). Pathogenesis of primary abnormalities of the mitral valve in Marfan's syndrome. British Heart Journal, 31, 679–683.
Loeys, B. L., Dietz, H. C., Braverman, A. C., et al. (2010). The revised Ghent nosology for the Marfan syndrome. Journal of Medical Genetics, 47, 476–485.
De Paepe, A., Devereux, R. B., Dietz, H. C., Hennekam, R. C., & Pyeritz, R. E. (1996). Revised diagnostic criteria for the Marfan syndrome. American Journal of Medical Genetics, 62, 417–426.
Barlow, J. B., & Bosman, C. K. (1966). Aneurysmal protrusion of the posterior leaflet of the mitral valve. An auscultatory-electrocardiographic syndrome. American Heart Journal, 71, 166–178.
Bhudia, S. K., Troughton, R., Lam, B. K., et al. (2006). Mitral valve surgery in the adult Marfan syndrome patient. The Annals of Thoracic Surgery, 81, 843–848.
Montgomery, R. A., Geraghty, M. T., Bull, E., et al. (1998). Multiple molecular mechanisms underlying subdiagnostic variants of Marfan syndrome. American Journal of Human Genetics, 63, 1703–1711.
Aalberts, J. J., Schuurman, A. G., Pals, G., et al. (2010). Recurrent and founder mutations in the Netherlands: extensive clinical variability in Marfan syndrome patients with a single novel recurrent fibrillin-1 missense mutation. Netherlands Heart Journal, 18, 85–89.
Pyeritz, R. E., & Wappel, M. A. (1983). Mitral valve dysfunction in the Marfan syndrome. Clinical and echocardiographic study of prevalence and natural history. The American Journal of Medicine, 74, 797–807.
Taub, C. C., Stoler, J. M., Perez-Sanz, T., et al. (2008). Mitral valve prolapse in Marfan syndrome: an old topic revisited. Echocardiography, 26(4), 357–364.
Detaint, D., Faivre, L., Collod-Beroud, G., et al. (2010). Cardiovascular manifestations in men and women carrying a FBN1 mutation. European Heart Journal, 31, 2223–2229.
Morse, R. P., Rockenmacher, S., Pyeritz, R. E., et al. (1990). Diagnosis and management of infantile Marfan syndrome. Pediatrics, 86, 888–895.
Sisk, H. E., Zahka, K. G., & Pyeritz, R. E. (1983). The Marfan syndrome in early childhood: analysis of 15 patients diagnosed at less than 4 years of age. The American Journal of Cardiology, 52, 353–358.
Faivre, L., Masurel-Paulet, A., Collod-Beroud, G., et al. (2009). Clinical and molecular study of 320 children with Marfan syndrome and related type I fibrillinopathies in a series of 1009 probands with pathogenic FBN1 mutations. Pediatrics, 123, 391–398.
Freed, L. A., Levy, D., Levine, R. A., et al. (1999). Prevalence and clinical outcome of mitral-valve prolapse. The New England Journal of Medicine, 341, 1–7.
Levine, R., Triulzi, M., Harrigan, P., & Weyman, A. (1987). The relationship of mitral annular shape to the diagnosis of mitral valve prolapse. Circulation, 75, 756–767.
Disse, S., Abergel, E., Berrebi, A., et al. (1999). Mapping of a first locus for autosomal dominant myxomatous mitral-valve prolapse to chromosome 16p11.2-p12.1. American Journal of Human Genetics, 65, 1242–1251.
Freed, L. A., Acierno, J. S., Jr., Dai, D., et al. (2003). A locus for autosomal dominant mitral valve prolapse on chromosome 11p15.4. American Journal of Human Genetics, 72, 1551–1559.
Nesta, F., Leyne, M., Yosefy, C., et al. (2005). New locus for autosomal dominant mitral valve prolapse on chromosome 13: clinical insights from genetic studies. Circulation, 112, 2022–2030.
Shi, Y., & Massague, J. (2003). Mechanisms of TGF-beta signaling from cell membrane to the nucleus. Cell, 113, 685–700.
Massam-Wu, T., Chiu, M., Choudhury, R., et al. (2010). Assembly of fibrillin microfibrils governs extracellular deposition of latent TGF beta. Journal of Cell Science, 123, 3006–3018.
Isogai, Z., Ono, R. N., Ushiro, S., et al. (2003). Latent transforming growth factor beta-binding protein 1 interacts with fibrillin and is a microfibril-associated protein. Journal of Biological Chemistry, 278, 2750–2757.
Judge, D. P., Biery, N. J., Keene, D. R., et al. (2004). Evidence for a critical contribution of haploinsufficiency in the complex pathogenesis of Marfan syndrome. The Journal of Clinical Investigation, 114, 172–181.
Ng, C. M., Cheng, A., Myers, L. A., et al. (2004). TGF-beta-dependent pathogenesis of mitral valve prolapse in a mouse model of Marfan syndrome. The Journal of Clinical Investigation, 114, 1586–1592.
Neptune, E. R., Frischmeyer, P. A., Arking, D. E., et al. (2003). Dysregulation of TGF-beta activation contributes to pathogenesis in Marfan syndrome. Nature Genetics, 33, 407–411.
Habashi, J. P., Judge, D. P., Holm, T. M., et al. (2006). Losartan, an AT1 antagonist, prevents aortic aneurysm in a mouse model of Marfan syndrome. Science, 312, 117–121.
Cohn, R. D., van Erp, C., Habashi, J. P., et al. (2007). Angiotensin II type 1 receptor blockade attenuates TGF-beta-induced failure of muscle regeneration in multiple myopathic states. Nature Medicine, 13, 204–210.
Jones, K. B., Myers, L., Judge, D. P., Kirby, P. A., Dietz, H. C., & Sponseller, P. D. (2005). Toward an understanding of dural ectasia: a light microscopy study in a murine model of Marfan syndrome. Spine, 30, 291–293.
Rodriguez-Vita, J., Sanchez-Lopez, E., Esteban, V., Ruperez, M., Egido, J., & Ruiz-Ortega, M. (2005). Angiotensin II activates the Smad pathway in vascular smooth muscle cells by a transforming growth factor-beta-independent mechanism. Circulation, 111, 2509–2517.
Lacro, R. V., Dietz, H. C., Wruck, L. M., et al. (2007). Rationale and design of a randomized clinical trial of beta-blocker therapy (atenolol) versus angiotensin II receptor blocker therapy (losartan) in individuals with Marfan syndrome. American Heart Journal, 154, 624–631.
Helin, K., Stoll, M., Meffert, S., Stroth, U., & Unger, T. (1997). The role of angiotensin receptors in cardiovascular diseases. Annals of Medicine, 29, 23–29.
Shafiq, M. M., Menon, D. V., & Victor, R. G. (2008). Oral direct renin inhibition: premise, promise, and potential limitations of a new antihypertensive drug. The American Journal of Medicine, 121, 265–271.
Pitt, B., Poole-Wilson, P. A., Segal, R., et al. (2000). Effect of losartan compared with captopril on mortality in patients with symptomatic heart failure: randomised trial—the Losartan Heart Failure Survival Study ELITE II. Lancet, 355, 1582–1587.
Barnett, A. H., Bain, S. C., Bouter, P., et al. (2004). Angiotensin-receptor blockade versus converting-enzyme inhibition in type 2 diabetes and nephropathy. The New England Journal of Medicine, 351, 1952–1961.
Jones, E. S., Black, M. J., & Widdop, R. E. (2004). Angiotensin AT2 receptor contributes to cardiovascular remodelling of aged rats during chronic AT1 receptor blockade. Journal of Molecular and Cellular Cardiology, 37, 1023–1030.
Daugherty, A., Manning, M. W., & Cassis, L. A. (2001). Antagonism of AT2 receptors augments angiotensin II-induced abdominal aortic aneurysms and atherosclerosis. British Journal of Pharmacology, 134, 865–870.
Nagashima, H., Sakomura, Y., Aoka, Y., et al. (2001). Angiotensin II type 2 receptor mediates vascular smooth muscle cell apoptosis in cystic medial degeneration associated with Marfan's syndrome. Circulation, 104, I282–I287.
Nagashima, H., Uto, K., Sakomura, Y., et al. (2002). An angiotensin-converting enzyme inhibitor, not an angiotensin II type-1 receptor blocker, prevents beta-aminopropionitrile monofumarate-induced aortic dissection in rats. Journal of Vascular Surgery, 36, 818–823.
Habashi, J. P., Doyle, J. J., Holm, T. M., et al. (2011). Angiotensin II type 2 receptor signaling attenuates aortic aneurysm in mice through ERK antagonism. Science, 332, 361–365.
Siragy, H. M., Inagami, T., Ichiki, T., & Carey, R. M. (1999). Sustained hypersensitivity to angiotensin II and its mechanism in mice lacking the subtype-2 (AT2) angiotensin receptor. Proceedings of the National Academy of Sciences of the United States of America, 96, 6506–6510.
Gu, X., & Masters, K. S. (2009). Role of the MAPK/ERK pathway in valvular interstitial cell calcification. American Journal of Physiology—Heart and Circulatory Physiology, 296, H1748–H1757.
Xu, J., Jian, B., Chu, R., et al. (2002). Serotonin mechanisms in heart valve disease II: the 5-HT2 receptor and its signaling pathway in aortic valve interstitial cells. American Journal of Pathology, 161, 2209–2218.
Loeys, B. L., Chen, J., Neptune, E. R., et al. (2005). A syndrome of altered cardiovascular, craniofacial, neurocognitive and skeletal development caused by mutations in TGFBR1 or TGFBR2. Nature Genetics, 37, 275–281.
Loeys, B. L., Schwarze, U., Holm, T., et al. (2006). Aneurysm syndromes caused by mutations in the TGF-beta receptor. The New England Journal of Medicine, 355, 788–798.
Attias, D., Stheneur, C., Roy, C., et al. (2009). Comparison of clinical presentations and outcomes between patients with TGFBR2 and FBN1 mutations in Marfan syndrome and related disorders. Circulation, 120, 2541–2549.
van de Laar, I. M., Oldenburg, R. A., Pals, G., et al. (2011). Mutations in SMAD3 cause a syndromic form of aortic aneurysms and dissections with early-onset osteoarthritis. Nature Genetics, 43, 121–126.
Acknowledgments
The authors gratefully acknowledge support from the Fondation Leducq, the W.W. Smith Charitable Trust, the Smilow Center for Marfan Syndrome Research, the National Marfan Foundation, the Howard Hughes Medical Institute, and the National Institutes of Health.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Judge, D.P., Rouf, R., Habashi, J. et al. Mitral Valve Disease in Marfan Syndrome and Related Disorders. J. of Cardiovasc. Trans. Res. 4, 741–747 (2011). https://doi.org/10.1007/s12265-011-9314-y
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12265-011-9314-y