Abstract
Transplantation of mesenchymal stem cells (MSC) improves repair and function recovery following myocardial infarction (MI), but underlying mechanisms remain to be elucidated. We hypothesize that MSC could achieve protection by paracrine effects through released mediators rather than direct cardiac regeneration. We sought to characterize the effects of MSC-secreted growth factors on extent of early recovery from MI. Swine subjected to acute MI by temporary balloon occlusion of the left anterior descending coronary artery using percutaneous techniques received intracoronary injection of either concentrated MSC-derived growth factors or control medium. Animals were killed at 7 days to evaluate early effects. Treatment with MSC-derived factors significantly reduced cardiac troponin-T elevation and improved echocardiographic parameters, including fractional area shortening, stroke volume, cardiac output, and wall motion score index. Quantitative evaluation of fibrosis by Verhoff staining revealed a reduction of the fibrotic area in the infarcted zone. Similarly, Masson’s trichrome staining revealed reduced myocardial damage as demonstrated by areas of relatively preserved myocardium in the infarcted area. TUNEL assay demonstrated less cardiomyocyte apoptosis. Protein array detected the presence of angiogenic (vascular endothelial growth factor, endothelin, and epiregulin), anti-apoptotic (Galectin-3, Smad-5, sRFP-1, and sRFP-4) and anti-remodeling factors. Reverse transcription polymerase chain reaction confirmed the expression of these factors. In summary, a single intracoronary injection of concentrated biologically active factors secreted by MSC could achieve early protection of ischemic myocardium and improve cardiac repair and contractility. MSC-derived growth factors injection (rather than MSC themselves) should be evaluated as a novel therapy to treat ischemic heart disease, avoiding many practical and technical issues of cell therapy.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Despite improvements in survival rates following myocardial infarction (MI), reduction in cardiac function attributable to irreversible loss of viable myocytes remains a major clinical problem [1]. Stem cell transplantation is a potential approach to repopulate injured myocardium [2], to treat heart failure [2, 3], and restore cardiac function [4]. Many cell types have been successfully engrafted into the injured myocardium and have been shown to have a favorable impact on structural and functional repair. However, the exact mechanisms underlying these beneficial effects remain to be elucidated.
Experimental data suggest that bone-marrow-derived mesenchymal stem cells (MSC) can repair infarcted myocardium [2, 5–7]. These cells are capable of both inducing myogenesis and promote angiogenesis, ultimately leading to improvement of cardiac contractility and function [2, 4–6]. We previously demonstrated that intramyocardial injection of MSC into rat and mice ischemic hearts improved cardiac healing and function as early as 3 days after MI [8, 9]. Such an early recovery could not be explained by direct de novo myogenesis, cellular fusion, or differentiation, suggesting alternate mechanisms [9]. MSC are known to secrete a wide spectrum of biologically active factors that can be found in the MSC-conditioned culture medium (MSC-CM) [10–12]. Under hypoxic culture conditions, such as those found in ischemic myocardium, the expression of several cytokines is significantly upregulated [10, 12–14]. We and others have shown that injection of MSC-derived factors (MSC-CM) from hypoxic or serum starvation cultured MSC either directly into infarcted hearts [8, 15], by intramuscular injections [16], or by intraperitoneal injections [12] improves ventricular function in small animals MI models.
Therefore, we hypothesize that paracrine mechanisms mediated by biologically active factors secreted by MSC could be responsible for their beneficial effects. The objective of the current study is to characterize the early effects of a single intracoronary injection of MSC-derived growth factors on functional recovery and myocardial repair in a swine model of MI using percutaneous techniques under fluoroscopic guidance. This convenient large animal model reproduces the clinical settings of an acute MI with percutaneous coronary intervention (PCI) used for revascularization, and this study presents a novel application of stem cell therapy.
Methods
MSC Isolation and Characterization
Swine MSC were isolated from bone marrow iliac crest aspirates and expanded as previously described [6, 9]. Immunophenotyping was performed by multiparameter flow cytometry (FACScan®; Becton Dickinson, Mountain View, CA, USA) with monoclonal antibodies directed against human antigens (Coulter Immunology, Hialeah, FL, USA) [17, 18].
Preparation of MSC-Derived Growth Factors from Hypoxic MSC-Conditioned Medium
To stimulate growth factor secretion [8, 13, 15], swine allogenic MSC were cultured under artificial hypoxic atmosphere (<1% oxygen) consisting of 5% CO2 balanced with nitrogen in serum-free medium. For each animal, MSC-derived growth factors contained in the supernatant of cultured MSC were obtained from 12 confluent (fourth to sixth passage, >90% MSC confluence) 10 cm2 plates of MSC exposed to hypoxia for 16 h. MSC-CM was collected, centrifuged to eliminate cells debris, and filtered, and proteins were concentrated using the Amicon centrifugal filters (Millipore, Bedford, MA, USA). Control animals were injected with serum-free medium prepared in similar hypoxic conditions and concentrated (control-CM).
Animal Preparation and Coronary Occlusion
Landrace pigs (30–35 kg) were obtained from Primiporcs (St-Gabriel-de-Brandon, Quebec, Canada). The Animal Experimentation Committee of the Montreal Heart Institute (Montreal, Canada) approved this protocol. Animals were anesthetized with sodium pentobarbital (30 mg/kg) and mechanically ventilated (Harvard Apparatus, South Natick, MA, USA) according to our standard protocol [19].
A 7-Fr central jugular venous access (Arrow International, Erding, Germany) was installed for repeated blood sampling. Arterial blood pressure was continuously monitored and recorded. A balloon catheter (Gemini, ACF Guidant California, 3–3.5 mm) was inserted into the left femoral artery and positioned in the left anterior descending (LAD) coronary artery distal to the first diagonal branch. Following heparinization (10 U/kg), the balloon catheter was inflated under angiographic guidance to a pressure sufficient to achieve complete coronary occlusion for 60 min [6]. Complete coronary occlusion by the balloon catheter was regularly verified by angiographic visualization using contrast injection and fluoroscopy [20]. MI was confirmed with continuous electrocardiogram (EKG) recording showing typical persistent ST segment elevation. Following balloon-catheter deflation and a 30-min reperfusion period, 10 ml of control-CM or MSC-derived factors were injected using an intracoronary infusion catheter (Remedy, Boston Scientific, 3–3.5 mm). Blood samples for cardiac troponin-T (cTnT) serum measurement (Montreal Heart Institute, Clinical Biochemistry Laboratory) were drawn at baseline and after different time points following CM injection. Animals were randomly assigned to the treatment group, and technicians were blinded to the treatment during MI procedure.
Myocardial Function Assessment by Echocardiography
A trained operator blinded to the assigned treatment performed transthoracic echocardiographic studies at baseline (before MI) and 1 week following MI using a M3S probe (2.0–4.3 MHz) and a Vivid 7 Dimension system (GE Healthcare Ultrasound, Horten, Norway). A left ventricular (LV) short-axis view at the papillary muscle level was recorded. LV areas at both end diastole (EDA) and end systole (ESA) were measured. LV fractional area shortening (FAS) representing global LV function was calculated as (EDA − ESA)/EDA × 100%. LV outflow tract (LVOT) dimension (D) was measured in zoomed parasternal long axis view, LVOT cross-sectional area (CSA) was calculated by CSA = π(D/2)2. In the apical five-chamber view, velocity time integral of trans-LVOT flow (VTI) and heart rate (HR) were obtained with pulsed wave Doppler sampled proximal to the aortic valve. Cardiac output (CO) was calculated as CO = CSA × VTI × HR. The average of three consecutive cardiac cycles was used for each measurement.
Histological Evaluation of Infarction and Apoptosis
Animals were killed at 7 days to assess early effects on myocardial repair. Heart sections at the levels of the LV papillary muscles were separated into four zones by visual inspection of the infarct and localization of the LAD: A and C as the transition-infarcted border zones, B as the infarcted antero/septal zone (between A and C), and D as the remote non-infarcted zone or LV free wall. Heart tissue was fixed, mounted in paraffin, and cut in 5-µm sections. Quantitative evaluation of fibrosis was performed by planimetry using Verhoff staining on digitalized images (average of ten random fields) using automated computer Macintosh ImageJ software v1.38X (NIH, USA), with pre-established and fixed calibration setup. Fibrotic area is presented as the percent of fibrosis (pink staining) over the total area.
Whole heart tissue sections stained with Masson’s trichrome were scanned using the slide scanner Super Coolscan 5000 ED (Nikon, USA), and the digitalized pictures were analyzed by planimetry with pre-established and fixed calibration setup. All non-red areas, representing nonviable tissue with collagen deposition, fibrosis, necrotic, and granulation tissues were subtracted from total surface area occupied by heart section to represent the viable area for each section expressed as ratio (percent) as described [21].
Cardiomyocyte apoptosis was characterized by TUNEL staining according to the manufacturer’s recommendations (http://www.millipore.com). To describe the extent of apoptosis, we used a semiquantitative scoring system with modifications [22]. Apoptosis was scored on a scale of 1–4 by two observers blinded to the treatment regimen, as follows: grade 1, no TUNEL(+) cells or minimal (<10%); grade 2, slight or few TUNEL(+) cells (<30%); grade 3, moderate TUNEL(+) cells (30–75%); and grade 4 severe or marked number of TUNEL(+) cells (>75%). Scores were averaged from each tissue section divided into nine quadrants, from every heart zones in each animal.
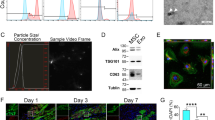
Characterization and Validation of MSC-Derived Growth Factors
Protein concentration in the conditioned medium (concentrated and non-concentrated) was evaluated by the Bio-Rad protein assay (Bio-Rad, USA). Characterization of MSC-derived factors in MSC-CM was assessed using the RayBio biotin label-based human antibody array I (RayBiotech, USA). Relative concentration of each factor was evaluated using the dedicated software from RayBiotech on the membrane containing internal controls for reference. Vascular endothelial growth factor (VEGF) was quantified with the VEGF quantikine enzyme-linked immunosorbent assay (ELISA) kit (R&D Systems, USA). Expression of selected genes by MSC was validated by semiquantitative reverse transcription polymerase chain reaction (RT-PCR). RNA was extracted using TRIzol and reverse-transcribed to complementary DNA using Moloney murine leukemia virus polymerase, then amplified with Taq polymerase (http://www.invitrogen.com). The 18S gene was used as the endogenous control. Sequences of the primers used are provided in Supplementary data. The PCR conditions were 95°C for 2 min, followed by 40 cycles of 95°C for 15 s, 60°C for 20 s, 72°C for 30 s, and final extension at 72°C for 5 min.
Statistical Analysis
Data are expressed as mean ± standard deviation for continuous variables and analyzed using Student’s t test. Categorical variables are expressed as a number (percentage) and compared using χ 2 test or Fishers’ exact test, as appropriate.
A hierarchical model was used to evaluate group difference in percent of fibrosis. This model accounts for the correlation between the multiples measurements in the same animal. The effect was analyzed at the level of the animal. A fully parameterized hierarchical model was built, including a coefficient for each section for each group (the MIXED procedure in SAS software, version 9.1; SAS Institute, Cary, NC, USA). The overall effect of “group” and “zones A to D” was assessed, and comparisons were made between the two groups for specific zone. From the model, group comparisons were also made for the average fibrosis percentage for zones A, B, and C.
In order to compare group apoptosis score, grading results (grades 1–4) were summarized in a 4 × 2 table (i.e., number or percentage of quadrants with grade 1, 2, 3, or 4). Group differences were compared using a χ 2 test. Weights were used in the model to obtain the average apoptosis score for the two observers.
We investigated earlier (3 days) and prolonged effects (28 days) of MSC-derived growth factors on cardiac function. In a parallel pilot study, five animals were treated in each group as above; animals were killed at 3 days after echocardiography (n = 2/group) and the remaining at 28 days (n = 3/group). Fully parameterized longitudinal mixed effect models were built for echocardiographic measurements, including a coefficient for each point in time for each group (the MIXED procedure). These models account for the correlation between repeated measurements in the same animal.
For all analyses, p < 0.05 were considered statistically significant.
Results
Characterization of MSC
Swine MSC did not express hematopoietic markers, including CD11b, CD14, and CD45 but were positive for MSC markers CD44 and CD90 (Table 1). Results were comparable to those obtained with human MSC. MSC are very resistant to hypoxic culture condition and serum starvation [7]. Using trypan blue staining, we observed that about 90% of the cells survived more than 48-h cultivation in these conditions, and there was no difference between cells subjected to hypoxia or normoxia, with or without serum [12].
Model of Acute MI and Evaluation of Myocardial Damage
In this study, 18 pigs underwent experimental MI. As proven angiographically, complete occlusion of the LAD was achieved in all pigs with the balloon catheter, along with successful reperfusion after balloon deflation. All pigs had significant ST segment elevation on continuous EKG, confirming MI. The mortality rate was 28%: severe arrhythmias were responsible for the early loss of three animals during myocardial ischemia. Two other animals died in the MSC-CM group: one on day 1 due to cardiac failure and the other on day 3 when put under general anesthesia for echocardiography. There were seven surviving animals in the MSC-CM group and six in the control group.
Despite the presence of many potent vasoactive factors found in the MSC-CM, no significant changes in hemodynamics were observed in the immediate period after MSC-derived factors injection. Blood pressure (systolic, diastolic, and mean) and heart rate were not different in the control group and the MSC-CM treated animals at all time points, including after CM injection and kill (data not shown). Serum cardiac Troponin T were <0.01 µg/L for all animals before MI (baseline level). Treatment with MSC-derived growth factors significantly reduced early troponin T elevation at 60 min after CM injection, but levels were not significantly different at 24 and 48 h post-MI, (Fig. 1).
Evaluation of Myocardial Function by Echocardiography
Echocardiographic values at 7 days were compared to baseline (before MI, each animal being its own control) and presented as percentage of change (Fig. 2). Myocardial infarct was associated with a reduction in contractility, which was significantly worst in the control group (P = 0.013) when looking at FAS, suggesting a favorable effects on the ischemic myocardium by the MSC-derived factors. Similarly, the left ventricular ejection fraction (LVEF) decreased in both groups after MI, but the group difference was not significant (P = 0.138). Stroke volume (SV) and CO improved with MSC-derived factors treatment, as opposed to a significant reduction in control animals (P values of 0.013 and 0.024, respectively). The deterioration in wall motion score index (WMSI) was significantly worst in the control group (P = 0.043). Left ventricular end-systolic volume (LVESv) was 58.5 ± 2.2 ml in the control group compared to 54.3 ± 1.1 ml in MSC-CM (P = 0.095). Likewise, left ventricular end-diastolic volume (LVEDv) was 108.6 ± 8.3 ml in the control group compared to 101.4 ± 9.6 ml in MSC-CM group (P = 0.443), see Table 2. Heart rate and blood pressure did not change over time, and differences were not significant between groups (data not shown).
Echocardiographic analysis at day 7 to evaluate early cardiac function recovery, results are presented as percent change versus baseline. LV function measured by FAS was significantly worst in the control group (n = 6) compared to MSC-CM treated group (n = 7), *P < 0.05. Similarly, MSC-CM treatment significantly improved stroke volume (SV), cardiac output (CO) and wall motion score index (WMSI)
Similarly to early beneficial effects observed at 7 days, animals treated with MSC-derived factors demonstrated a better cardiac function represented by WMSI (P < 0.001) and LVEF (P = 0.073) at 28 days compared to controls (Table 2 and Supplementary figure). Moreover, treatment with MSC-derived factors demonstrated favorable effects at 28 days on remodeling and prevention of cardiac dilatation post-MI. Indeed, animals in control group showed larger LV cardiac cavities compared to MSC-CM treated animals at 28 days with LVES of 89.9 ± 9.7 ml vs 42.3 ± 6.2 ml (P < 0.001) and LVED of 150.7 ± 5.1 ml and 101.4 ± 9.6 ml (P < 0.001), respectively (Table 2).
Histological Analysis for Fibrosis, Myocardial Damage, and Cell Death
Treatment with MSC-derived factors significantly reduced collagen deposition and fibrosis in the infarcted border zones A and C, but not in the infarcted area B (Fig. 3). When combining all infarcted zones A + B + C, the area occupied by fibrotic tissue was smaller in the MSC-CM group compared to controls.
Quantitative evaluation of fibrosis by Verhoff staining of left ventricular (LV) sections at 7 days post-treatment. a Representative tissue sections with fibrosis stained pink-red, original magnification ×10. b Fibrotic area (%) represents the ratio of area occupied by fibrotic tissue over the entire area. LV heart zones examined are as follows: A and C are infarct transition-border zones and B is the infarcted antero-septal zone. MSC-CM treatment significantly reduced the fibrotic area in the infarct border zones (A and C combined) and in the infarcted zone (A+B+C combined)
Qualitative histological analysis suggested a different pattern of myocardial injury with reduced myocardial damage in the MSC-CM group as demonstrated by areas of relatively preserved myocardium in the border and infarcted areas (Fig. 4a). Quantitatively, planimetric analysis demonstrated a significantly smaller area of viable tissues in the infarcted area of control animals (Fig. 4b).
a Masson’s trichrome staining at 7 days. Representative whole heart sections in the infarcted zone is presented on the left, as well as the higher magnifications (original ×10) in the black box. b Quantitative planimetric evaluation revealed that MSC-CM significantly reduced non-viable tissue area (necrosis, fibrosis, and collagen deposition) with less myocardial damage and a more favorable healing process in the infarcted zone B and all infarcted LV zones combined (A+B+C). LV heart zones examined are as follows: A and C are infarct transition-border zones, B is the infarcted zone, and D is the remote normal LV free wall
Treatment with MSC-derived factors significantly decreased the number of TUNEL-positive cardiomyocytes in the infarcted zone B, and a trend toward reduction of apoptosis was observed in zone A (Table 3). When combining all infarcted zones A + B + C, the TUNEL scores in these regions were significantly smaller in the MSC-CM group.
Characterization of MSC-Derived Factors in Conditioned Medium
Protein concentration in MSC-CM (n = 8, unconcentrated medium collected from cultured MSC) was 230.6 ± 96.7 μg/ml, compared to 0.22 ± 0.7 μg/ml (P < 0.001) in α-MEM culture medium alone [n = 8, control medium, no fetal bovine serum (FBS) serum, no cells]. In the samples injected in our study and concentrated using the Amicon filters, total protein concentration in the MSC-CM was increased to 519.9 ± 617.7 μg/ml (n = 4) compared to 1.3 ± 1.2 μg/ml in control CM (n = 6, control medium, no FBS serum, and no MSC; P < 0.05).
We used the RayBio® human protein array to characterize the growth factors secreted by MSC. Many factors, including epiregulin, endotheline, fibroblast growth factor-16, IL-1α, secreted frizzled related protein 1 and 4 (sFRP-1 and sFRP-4), tissue inhibitor of matrix metalloprotease-2 (TIMP-2), and VEGF, were detected in the supernatants of swine MSC (Table 4). Results obtained using human MSC were similar for these factors. Quantitative measurement by VEGF ELISA validated the secretion of VEGF by the swine MSC and showed a significant increase when swine MSC were cultured under hypoxic conditions (Fig. 5a). Moreover, VEGF concentration in MSC-CM from injected animals (n = 4) was very high 1,326.4–9,854.2 pg/ml (mean, 3,798 ± 4,052).
Detection of growth factors in the supernatants of cultured MSC. a Quantitative measurement of VEGF by ELISA in swine MSC-CM. VEGF secretion is significantly increased when MSC are cultured in hypoxic conditions compared to normoxic conditions. VEGF concentration in the MSC supernatant was normalized by the number of MSC cells in the culture dish (1 × 105 cells). b Production of growth factors by human and swine MSC detected distinctly by RT-PCR, cultured under normoxia (N) or hypoxia (H)
Semiquantitative analysis of messenger RNA expression by RT-PCR confirmed the production of various factors by swine MSC. The expression of interesting genes including angiogenic factors (epiregulin and endothelin), anti-apoptotic factors (sFRP-1), and anti-remodeling factors (TIMP-1 and TIMP-2) were detected. These genes were also expressed by human MSC (Fig. 5b).
Discussion
The mechanism underpinning effects of MSC therapy appears to be far more complex than previously anticipated but is certainly multifactorial [23]. It remains unclear whether the beneficial effect of this cell-based therapy is a direct consequence of the transplanted cells participating and integrating in a functional syncytium with the host myocardium or, alternatively, if the transplanted cells improve cardiac function without directly contributing to systolic contraction [2].
MSC transplantation may improve myocardial function recovery predominantly by facilitating endogenous repair mechanisms, rather than through direct regeneration. Therefore, it is speculated that implanted MSC could secrete bioactive factors, which may stimulate angiogenesis [10], suppress apoptosis of cardiomyocytes [12, 15], increase efficiency of cardiomyocyte metabolism [24], improve inotropy of survival myocytes by affecting the activities of ion channels [25], or modulate interstitial matrix composition and remodeling [26–28]. Moreover, transplantation of MSC into ischemic heart may have beneficial effect on endogenous cardiac resident stem cells in a paracrine manner [26, 29].
We previously reported that intramyocardial injection of MSC into rat and mice ischemic hearts improved cardiac healing as early as 72 h after MI, which is too early to be explained solely by direct myocardial regeneration from MSC [8, 9]. Bioactive factors secreted by MSC and found in MSC-CM reduced apoptosis and triggered vigorous spontaneous contraction of isolated hypoxic adult rat cardiomyocytes in vitro, suggesting the presence of cytoprotective and inotropic factors [8, 15]. We observed that pre-stimulation of MSC by hypoxia improved the cytoprotective effects. Indeed, it has been reported that the expression of several growth factors is upregulated in hypoxic cultured MSC [10, 12–14]. Therefore, using hypoxia-stimulated MSC, we previously demonstrated in a rat model of acute MI that direct intramyocardial injection of MSC-derived growth factors could improve cardiac function and protection [8, 15], providing strong evidences for paracrine hypothesis and indirect effects of MSC therapy.
Herein, in larger animals, we demonstrated that a single intracoronary injection of MSC-derived factors into ischemic myocardium resulted in significantly lower early troponin elevation, suggesting a reduction in tissue damage [30]. Serum cardiac troponin T (cTnT) has been validated in laboratory animals as a biomarker of cardiac injury and level increases in proportion to severity of cardiac injury [31]. In the swine model of acute MI, the release of troponin is known to occur early following ischemic injury, and the critical time for measurements is within the first few hours [20, 32]. We also measured troponin subsequently at 24 and 48 h but failed to unveil any differences between animal groups. It is conceivable that we missed important variation within the first 24 h of ischemic injury. Alternatively, it is possible that MSC-derived factors act as preconditioning factors on ischemic tissues or by modulation of the reperfusion injury.
Microscopic analysis of myocardial infarct demonstrated a favorable healing process and remodeling with a reduction of the fibrosis and necrosis in animals treated with MSC-derived factors. It has been reported that apoptotic cell death contributes to expansion of MI extent and progression of LV remodeling after MI. Accordingly, apoptosis is a key pathologic feature in acute MI and heart failure [33]. Understanding the mechanisms involved in the apoptotic cascade may be useful in better understanding of heart failure and its management. Anti-apoptotic treatments may be effective in the prevention and treatment of post-infarction remodeling and heart failure [33].
Importantly, echocardiographic data demonstrated that early reduction in myocardial injury by MSC-derived factors had beneficial effects on myocardial contractile function as shown by significant preservation at 7 days of FAS, a significant improvement in SV and CO. Moreover, WMSI, used as a surrogate measure of LV function [34], was significantly improved in the MSC-CM group. These important findings cannot be attributed to a difference in heart rate between controls and MSC-CM-treated animals. Remarkably, the intracoronary injection of MSC-derived factors with potential vasoactive effects had no impact on blood pressure or hemodynamics. Inspired by our previous work on rodent, where we achieved significant myocardial repair and functional recovery after only 3 days following MSC or MSC-CM intracardiac injection [8, 13, 15, 24, 35], we investigated early myocardial repair in the swine at 7 days after MI. We are aware that this early time point may fail to uncover more significant improvements on global cardiac function due to the persisting stunning effects of the ischemic myocardium, the lack of recovery and remodeling, and other important cellular interactions such as neovascularization. Nevertheless, these early favorable effects on improved cardiac function were sustained up to 28 days, as shown in a parallel pilot study. MSC-derived factor treated animals demonstrated a significantly better WMSI and a trend toward improved LVEF (see Supplementary data). More interestingly, we also observed a significant improvement in LV remodeling with reduction of LVES and LVED in the MSC-derived factor treated animals. Our findings correlate with several clinical trials where the favorable impact of bone marrow stem cell injection into ischemic heart was seen on the regional infarcted area, not of global LVEF by echocardiography [36–38].
Because acute myocardial ischemia and subacute microinfarction have been reported after intracoronary arterial cellular injection [39], MSC were not injected in this study as controls [6, 40]. Instead, MSC-derived growth factors and control-CM were injected once in our protocol, and immediately after MI, the results of several injections were not investigated. Optimal timing for injection has yet to be determined, but infusion of MSC-derived factors at time of PCI for reperfusion of acute MI is the most clinically efficient way for early myocardial protection and repair.
Consistent with previous work, results of the current study demonstrated the importance of mediators produced by hypoxia-stimulated MSC and the prospect to use MSC-derived factors to achieve protection and functional improvement of the ischemic myocardium [8, 13, 15]. In accordance with previous reports, we identified a broad spectrum of factors secreted by MSC [10–13]. Some of these factors have been shown individually to have positive effects on experimental blood flow recovery, cardioprotection, cell proliferation, survival, and anti-apoptosis [10–12, 41–44]. However, we do not know yet the functional role of each cytokine and growth factors and which play the most important in myocardial repair and function recovery [12]. TIMP-1 has been found by Singela et al [45]. to be an important anti-apoptotic factor found in embryonic stem cell-conditioned medium. Recently, VEGF has been identified as a key therapeutic trophic factor in MSC-mediated cardiac repair by Zisa et al [46]. These authors and others [12] found a VEGF concentration of 40–225 pg to be sufficient for in vivo cardioprotective effects. We injected animals with concentration of VEGF up to 9,854 pg/ml. Of note, our experimental protocol relies on a single injection of concentrated MSC-derived factors, and we achieved injection of high amount of MSC-derived factors (final total protein concentration in the injectate of 143–1,440 ug/ml). Other groups used repeated injection for myocardial repair (intraperitoneal or intramuscular) because they injected unconcentrated MSC-CM [12, 16]. We believe that the delivery of highly concentrated mixture of MSC-derived factors is superior to unconcentrated MSC-conditioned medium. We combined the medium from 12 Petri dishes (10-cm diameter, about 5–6 ml of medium each) to prepare the CM to be injected for each swine, which represent growth factors produced by approximately 40–50 million MSC cells, as reported by other investigators in similar model injecting MSC into swine ischemic heart [40].
Herein, we postulated that, first, MSC transplantation could be used for the treatment of ischemic heart disease and that, second, important mechanisms mediating the beneficial effects of this cell-based therapy on cardiac function and repair may be an early effect through the release of biologically active and cytoprotective factors secreted by hypoxia-stimulated MSC. Because early reperfusion by PCI is the treatment of choice in the clinical setting of an ongoing acute MI [47], we developed and used a reproducible large animal model that mimics acute MI and reperfusion in the human by means of PCI techniques. Using similar experimental protocol in the swine with 60-min LAD occlusion and reperfusion, Freyman and coworkers [40] demonstrated a reproducible infarction affecting 20–30% of the LV. The intracoronary route of administration of stem cells or growth factors has been demonstrated to be safe in clinical trial [48–50]. To our knowledge, this is the first study to investigate the paracrine and indirect effects of stem cell therapy by percutaneous intracoronary injection of MSC-derived growth factors for the treatment of acute myocardial ischemia in a pre-clinical large animal model.
In conclusion, the present study was designed to characterize the early protective effects and functional improvement of the ischemic myocardium following a single intracoronary injection of MSC-derived factors in a preclinical experimental large animal model. It is interesting to speculate that MSC-derived growth factor injection could be used as a novel pharmacological therapy to treat ischemic heart diseases, rather than MSC themselves, thus avoiding many practical and technical issues regarding cell therapy. MSC-CM could be produced by an established cell line and be readily available for any patient presenting with an acute myocardial infarct in the emergency room and undergoing acute PCI treatment for myocardial reperfusion. Moreover, combining stem cells and gene therapy, MSC could be cultured and genetically modified ex vivo to alter the expression of targeted cytokines, making these cells ideal to be used as “minipumps” to produce and release factors required for improving tissue repair, viability, contractility, and blood flow.
References
Timmermans, F., De Sutter, J., & Gillebert, T. C. (2003). Stem cells for the heart, are we there yet? Cardiology, 100, 176–185.
Dowell, J. D., Rubart, M., Pasumarthi, K. B., Soonpaa, M. H., & Field, L. J. (2003). Myocyte and myogenic stem cell transplantation in the heart. Cardiovascular Research, 58, 336–350.
Raeburn, C. D., Zimmerman, M. A., Arya, J., Banerjee, A., & Harken, A. H. (2002). Stem cells and myocardial repair. Journal of the American College of Surgeons, 195, 686–693.
Tomita, S., Mickle, D. A., Weisel, R. D., et al. (2002). Improved heart function with myogenesis and angiogenesis after autologous porcine bone marrow stromal cell transplantation. Journal of Thoracic and Cardiovascular Surgery, 123, 1132–1140.
Tomita, S., Li, R. K., Weisel, R. D., et al. (1999). Autologous transplantation of bone marrow cells improves damaged heart function. Circulation, 100, II247–II256.
Shake, J. G., Gruber, P. J., Baumgartner, W. A., et al. (2002). Mesenchymal stem cell implantation in a swine myocardial infarct model: Engraftment and functional effects. Annals of Thoracic Surgery, 73, 1919–1925. discussion 26.
Mangi, A. A., Noiseux, N., Kong, D., et al. (2003). Mesenchymal stem cells modified with Akt prevent remodeling and restore performance of infarcted hearts. Nature Medicine, 9, 1195–1201. Epub 2003 Aug 10.
Gnecchi, M., He, H., Liang, O. D., et al. (2005). Paracrine action accounts for marked protection of ischemic heart by Akt-modified mesenchymal stem cells. Nature Medicine, 11, 367–368.
Noiseux, N., Gnecchi, M., Lopez-Ilasaca, M., et al. (2006). Mesenchymal stem cells overexpressing Akt dramatically repair infarcted myocardium and improve cardiac function despite infrequent cellular fusion or differentiation. Molecular Therapy, 14, 840–850.
Kinnaird, T., Stabile, E., Burnett, M. S., et al. (2004). Marrow-derived stromal cells express genes encoding a broad spectrum of arteriogenic cytokines and promote in vitro and in vivo arteriogenesis through paracrine mechanisms. Circulation Research, 94, 678–685.
Kinnaird, T., Stabile, E., Burnett, M. S., et al. (2004). Local delivery of marrow-derived stromal cells augments collateral perfusion through paracrine mechanisms. Circulation, 109, 1543–1549.
Takahashi, M., Li, T. S., Suzuki, R., et al. (2006). Cytokines produced by bone marrow cells can contribute to functional improvement of the infarcted heart by protecting cardiomyocytes from ischemic injury. American Journal of Physiology. Heart and Circulatory Physiology, 291, H886–H893.
Mirotsou, M., Zhang, Z., Deb, A., et al. (2007). Secreted frizzled related protein 2 (Sfrp2) is the key Akt-mesenchymal stem cell-released paracrine factor mediating myocardial survival and repair. Proceedings of the National Academy of Sciences of the United States of America, 104, 1643–1648.
Rehman, J., Traktuev, D., Li, J., et al. (2004). Secretion of angiogenic and antiapoptotic factors by human adipose stromal cells. Circulation, 109, 1292–1298.
Gnecchi, M., He, H., Noiseux, N., et al. (2006). Evidence supporting paracrine hypothesis for Akt-modified mesenchymal stem cell-mediated cardiac protection and functional improvement. Faseb Journal, 20, 661–669.
Shabbir, A., Zisa, D., Suzuki, G., & Lee, T. (2009). Heart failure therapy mediated by the trophic activities of bone marrow mesenchymal stem cells: a noninvasive therapeutic regimen. American Journal of Physiology. Heart and Circulatory Physiology, 296, H1888–H1897.
Allan, D. S., Dubé, P., Roy, J., Busque, L., & Roy, D. C. (2007). Endothelial-like vascular progenitor cells from autologous and allogeneic donors: mobilization features distinct from hematopoetic progenitors. Biology of Blood & Marrow Transplantation, 13, 433–439.
Guimond, M., Balassy, A., Barrette, M., Brochu, S., Perreault, C., & Roy, D. C. (2002). P-glycoprotein targeting: a unique strategy to selectively eliminate immunoreactive T cells. Blood, 100, 375–382.
Perrault, L. P., Malo, O., Desjardins, N., et al. (2002). Surgical experience with retroperitoneal heterotopic heart transplantation in the large white domestic swine. Journal of Investigative Surgery, 15, 45–55.
Pye, J., Ardeshirpour, F., McCain, A., et al. (2003). Proteasome inhibition ablates activation of NF-kappa B in myocardial reperfusion and reduces reperfusion injury. American Journal of Physiology. Heart and Circulatory Physiology, 284, H919–H926.
Berry, M. F., Engler, A. J., Woo, Y. J., et al. (2006). Mesenchymal stem cell injection after myocardial infarction improves myocardial compliance. American Journal of Physiology. Heart and Circulatory Physiology, 290, H2196–H2203.
Ananiadou, O. G., Bibou, K., Drossos, G. E., et al. (2007). Effect of profound hypothermia during circulatory arrest on neurologic injury and apoptotic repressor protein Bcl-2 expression in an acute porcine model. Journal of Thoracic and Cardiovascular Surgery, 133, 919–926.
Wollert, K. C., & Drexler, H. (2005). Clinical applications of stem cells for the heart. Circulation Research, 96, 151–163.
Gnecchi, M., He, H., Melo, L. G., et al. (2009). Early beneficial effects of bone marrow-derived mesenchymal stem cells overexpressing Akt on cardiac metabolism after myocardial infarction. Stem Cells, 27, 971–979.
Benzhi, C., Limei, Z., Ning, W., et al. (2009). Bone marrow mesenchymal stem cells upregulate transient outward potassium currents in postnatal rat ventricular myocytes. Journal of Molecular and Cellular Cardiology, 47, 41–48.
Braga, L. M., Rosa, K., Rodrigues, B., et al. (2008). Systemic delivery of adult stem cells improves cardiac function in spontaneously hypertensive rats. Clinical and Experimental Pharmacology and Physiology, 35, 113–119.
Xu, R. X., Chen, X., Chen, J. H., Han, Y., & Han, B. M. (2009). Mesenchymal stem cells promote cardiomyocyte hypertrophy in vitro through hypoxia-induced paracrine mechanisms. Clinical and Experimental Pharmacology and Physiology, 36, 176–180.
Guo, J., Lin, G. S., Bao, C. Y., Hu, Z. M., & Hu, M. Y. (2007). Anti-inflammation role for mesenchymal stem cells transplantation in myocardial infarction. Inflammation, 30, 97–104.
Nakanishi, C., Yamagishi, M., Yamahara, K., et al. (2008). Activation of cardiac progenitor cells through paracrine effects of mesenchymal stem cells. Biochemical and Biophysical Research Communications, 374, 11–16.
De Sousa, E., Veksler, V., Minajeva, A., et al. (1999). Subcellular creatine kinase alterations. Implications in heart failure. Circulation Research, 85, 68–76.
O'Brien, P. J., Dameron, G. W., Beck, M. L., et al. (1997). Cardiac troponin T is a sensitive, specific biomarker of cardiac injury in laboratory animals. Laboratory Animal Science, 47, 486–495.
Vikenes, K., Westby, J., Matre, K., Kuiper, K. K., Farstad, M., & Nordrehaug, J. E. (2002). Release of cardiac troponin I after temporally graded acute coronary ischaemia with electrocardiographic ST depression. International Journal of Cardiology, 85, 243–251. discussion 52-3.
Abbate, A., Bussani, R., Amin, M. S., Vetrovec, G. W., & Baldi, A. (2006). Acute myocardial infarction and heart failure: role of apoptosis. International Journal of Biochemistry and Cell Biology, 38, 1834–1840.
Galasko, G. I., Basu, S., Lahiri, A., & Senior, R. (2001). A prospective comparison of echocardiographic wall motion score index and radionuclide ejection fraction in predicting outcome following acute myocardial infarction. Heart, 86, 271–276.
Noiseux, N., Lopez Ilasaca, M., Gnecchi, M., et al. (2006). Mesenchymal stem cells over-expressing akt dramatically repairs infarcted myocardium and improves cardiac function despite infrequent cellular fusion or differentiation. Molecular Therapy Journal, 14, 840–850.
Janssens, S., Dubois, C., Bogaert, J., et al. (2006). Autologous bone marrow-derived stem-cell transfer in patients with ST-segment elevation myocardial infarction: double-blind, randomised controlled trial. Lancet, 367, 113–121.
Lunde, K., Solheim, S., Aakhus, S., et al. (2006). Intracoronary injection of mononuclear bone marrow cells in acute myocardial infarction. New England Journal of Medicine, 355, 1199–1209.
Strauer, B. E., Brehm, M., Zeus, T., et al. (2002). Repair of infarcted myocardium by autologous intracoronary mononuclear bone marrow cell transplantation in humans. Circulation, 106, 1913–1918.
Vulliet, P. R., Greeley, M., Halloran, S. M., MacDonald, K. A., & Kittleson, M. D. (2004). Intra-coronary arterial injection of mesenchymal stromal cells and microinfarction in dogs. Lancet, 363, 783–784.
Freyman, T., Polin, G., Osman, H., et al. (2006). A quantitative, randomized study evaluating three methods of mesenchymal stem cell delivery following myocardial infarction. European Heart Journal, 27, 1114–1122.
Buschmann, I., Heil, M., Jost, M., & Schaper, W. (2003). Influence of inflammatory cytokines on arteriogenesis. Microcirculation, 10, 371–379.
Heil, M., Ziegelhoeffer, T., Mees, B., & Schaper, W. (2004). A different outlook on the role of bone marrow stem cells in vascular growth: bone marrow delivers software not hardware. Circulation Research, 94, 573–574.
Kinnaird, T., Stabile, E., Burnett, M. S., & Epstein, S. E. (2004). Bone marrow-derived cells for enhancing collateral development: mechanisms, animal data, and initial clinical experiences. Circulation Research, 95, 354–363.
Toma, C., Pittenger, M. F., Cahill, K. S., Byrne, B. J., & Kessler, P. D. (2002). Human mesenchymal stem cells differentiate to a cardiomyocyte phenotype in the adult murine heart. Circulation, 105, 93–98.
Singla, D. K., & McDonald, D. E. (2007). Factors released from embryonic stem cells inhibit apoptosis of H9c2 cells. American Journal of Physiology. Heart and Circulatory Physiology, 293, H1590–H1595.
Zisa, D., Shabbir, A., Suzuki, G., & Lee, T. (2009). Vascular endothelial growth factor (VEGF) as a key therapeutic trophic factor in bone marrow mesenchymal stem cell-mediated cardiac repair. Biochemical and Biophysical Research Communications, 390, 834–838.
Topol, E. J. (2003). Current status and future prospects for acute myocardial infarction therapy. Circulation, 108, III6–III13.
Abdel-Latif, A., Bolli, R., Tleyjeh, I. M., et al. (2007). Adult bone marrow-derived cells for cardiac repair: a systematic review and meta-analysis. Archives of Internal Medicine, 167, 989–997.
Ince, H., Valgimigli, M., Petzsch, M., et al. (2008). Cardiovascular events and re-stenosis following administration of G-CSF in acute myocardial infarction: systematic review and meta-analysis. Heart, 94, 610–616.
Mansour, S., Roy, D. C., Bouchard, V., et al. (2009). COMPARE-AMI Trial: Comparison of Intracoronary Injection of CD133+ Bone Marrow Stem Cells to Placebo in Patients After Acute Myocardial Infarction and Left Ventricular Dysfunction: Study Rationale and Design. Journal of Cardiovascular Translational Research, in press.
Acknowledgements
We acknowledge Dr. D.C. Roy (Hôpital Maisonneuve-Rosemont) for his contribution in flow cytometric analyses. We thank M.P. Mathieu, E. Reny-Nolin, S. Gilligan, P. Geoffroy, and D. Lauzier for their precious help in this study and Dr Yan Fen Shi for the echocardiographic analysis. Drs. Noiseux and Perrault are scholars of Fonds de la Recherche en Santé du Québec (FRSQ). Dr. Noiseux and Perrault are supported by the Heart and Stroke Foundation of Québec, and Department of Surgery, Université de Montréal. Dr Stevens is supported by the Canadian Institutes of Health Research (CIHR).
Disclosures
No conflict of interest to disclose.
Author information
Authors and Affiliations
Corresponding author
Electronic supplementary material
Below is the link to the electronic supplementary material.
Supplementary data
(DOC 42 kb)
Supplementary figure
Echocardiographic analysis up to 28 days. A Intracoronary injection of MSC-derived growth factors after acute MI had persistent favorable effects on cardiac function as revealed by a significantly improved WMSI, used as an indicator of LV function and contractility (P < 0.001). B Similarly, LVEF tended to be worst in the control group (P = 0.072). Number of animals: n = 11 and 12 at baseline, n = 5 at 3 days, n = 6 and 7 at 7 days, and n = 3 at 30 days for controls and MSC-CM, respectively. Statistical analyses were made using longitudinal mixed effect models (JPEG 408 kb) (JPEG 408 kb)
Rights and permissions
About this article
Cite this article
Nguyen, BK., Maltais, S., Perrault, L.P. et al. Improved Function and Myocardial Repair of Infarcted Heart by Intracoronary Injection of Mesenchymal Stem Cell-Derived Growth Factors. J. of Cardiovasc. Trans. Res. 3, 547–558 (2010). https://doi.org/10.1007/s12265-010-9171-0
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12265-010-9171-0