Abstract
The aim of this study is to evaluate the effectiveness and feasibility of Limberg and Karydakis flap in complicated and recurrent cases of pilonidal sinus. This study was performed on 54 patients with complicated or recurrent (PSD) who referred to Minya University Hospital from January 2018 to January 2019. Patients were randomly divided into two groups, group A who were subjected to the Limberg flap and group B who were subjected to the Karydakis flap technique. Regarding postoperative complications, the occurrence of wound breakdown in the Karydakis group was 40.7% versus 11.1% in the Limberg group. No recurrence occurred in the Limberg group but recurrence observed in six cases in the Karydakis group. In the Karydakis group, eight patients had infection in comparison to one case in the Limberg group. All these differences were statistically significant. The overall patient satisfaction in the Limberg group was significantly higher than that in the Karydakis group. It is concluded that Limberg flap rotation is clearly preferred in management of recurrent and complicated PNS for safety reasons given its low recurrence and postoperative complication rates.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Pilonidal sinus disease (PSD) is a chronic inflammation and infection of the sacrococcygeal or intergluteal region. It is commonly affects young adult males after puberty. Patients usually presents with swelling, abscess, and discharge in sacrococcygeal region or painful sinus tract in the natal cleft [1, 2].
The etiology and pathogenesis of PSD are not clear [3, 4]. The pathogenesis of the disease is hypothesized to be related to deep natal cleft associated with other favorable factors such as sweating, maceration, poor personal hygiene, bacterial contamination, and penetration of shed hair shafts through the skin in the intergluteal region, which resulting in foreign body reaction, leading to abscess and sinus formation [5, 6]. Male sex, family history, sedentary lifestyle, obesity, and jobs that require sitting for long hours are among the listed risk factors [7].
Although many treatment methods have been described for the treatment of PSD, an ideal treatment has not been determined until now due to high rate of recurrence, infections, and delayed wound healing [8]. A number of surgical options are available. The simplest are incision and drainage, laying open, open excision, excision, and primary closure [9]. Simple excision techniques are associated with high morbidity and recurrence (0–5%) due to presence of natal cleft which provides a portal for hair entry starting the vicious circle of abscess formation, and discharging sinuses begins [10]. Accumulation of dead tissue or debris in the intergluteal cleft, sweating, friction, and poor hygiene are predisposing factors for recurrence [11].
The more complex surgical options include Kardaykis and rhomboid excision with Limberg flap. The purpose with these methods is to prevent recurrence through removing the cavity in the natal cleft and lateralization of the midline. It is achieved with the Karydakis flap (KF) by moving the suture laterally, while in the Limberg flap (LF) operation by flattening the natal cleft with a full-thickness flap [12].
The objective of this study is to evaluate the effectiveness and feasibility of KF and LF in complicated and recurrent cases of pilonidal sinus.
Patient and Methods
This study was performed on 54 patients with complicated or recurrent (PSD) who referred to Minya University Hospital from January 2018 to January 2019. This study is a prospective, comparative study using randomized controlled trial (RCT).
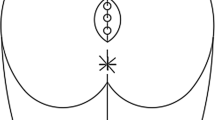
Patients with complicated or recurrent pilonidal sinus were included in the study. Patients were considered they have complicated pilonidal sinus when the patient have multiple sinuous orifices in the sacrococcygeal region; large wound dehiscence after previous surgical interference (Fig. 1); large external opening of the pilonidal sinus; sinuses localized laterally of the midline (Fig. 2), while the diagnosis of recurrent PSD was made based on clinical features no matter what the first operation was. Thirty six patients were referred to us with recurrence following primary surgery while there was 18 patients had complicated disease.
The exclusion criteria were cases with incomplete patients’ data, patients who were lost to follow-up, patient presenting with different conditions mimicking PNS, and patients with chronic conditions such as immunosuppression and diabetes mellitus.
Sample size was calculated according to the following formula [13]:
where α = 0.5, β = 0.1, μ1 = 2, μ2 = 4, σ = 2, K = 4, ρ = 0.9.
Then, we added additional number, about 20% of the calculated sample to guard against drop out. All patients who met the inclusion criteria were selected. All details of both the procedures were explained to all the patients and then they agreed for being randomized. Written consent from the patients was obtained after that.
An independent clinician was responsible for generating a random allocation sequence that kept hidden from all the trial participants. Based on type of operation, the participants were assigned equally into two groups using a computer-generated block randomization technique. The printed letters were folded several times and placed within an aluminum foil. The letter placed inside an opaque sealed and stapled envelope, including patient’s identification code, name, time, and date. The type of treatment was masked for the patient (single-blinded technique).
Patients were randomly divided into two groups:
-
Group A: this group included 27 patients who were subjected to the Limberg flap technique.
-
Group B: this group included 27 patients who were subjected to the Karydakis flap technique.
Surgical Procedure
Patients were placed in the prone position under general or spinal anesthesia. Intravenous 1 g of ceftriaxone was administered as antibiotic prophylaxis. In group A, the area of the sinus was marked in the shape of a rhomboid and the rotation (Limberg) flap was drawn to the site of sinuses. The rhomboid excision was carried down to the pre-sacral fascia. The subcutaneous tissue was approximated with absorbable sutures. Suction drains were placed in all patients (Fig. 1). While in group B, the Karydakis flap was performed as an asymmetrical elliptic excision was done, lower and upper ends being located at approximately 2 cm lateral to the natal cleft, and all defective tissues were removed until reaching to the healthy borders. After that, the medical wound edge was mobilized, and the flap was slid by suturing to the fascia and skin suitable wound layers on the lateral wound edge corresponding to one another. The subcutaneous tissue was closed with 2-fold 2/0 polyglactin suture, and the skin was closed with 3/0 polypropylene mattress suture. In all patients, a suction drain was applied to the region (Fig. 2).
The demographic data of the patients included in the study were recorded. Preoperative presence of an infection or abscess; number and outcome of previous surgery in recurrent cases; operative time; hospital stay; time of drain removal and early postoperative complications: wound site infection, seroma, discharge, and wound dehiscence; recovery time, time to return to work; and patient satisfaction were recorded. Follow-up was scheduled for all patients as visits at 3 and 10 days following discharge and once at the end of 1, 3, 6, and 12 months after the operation. Preoperative evaluation of this area with a sinogram was performed routinely to look for any branching of the tract.
Ethical Approval
The protocol of the study was discussed and approved regarding ethics of research in the general surgical department. The study had been approved by the ethical committee for human studies in our institution. Full written, informed consent was signed from all participants.
Statistical Analysis
The statistical program SPSS version 13 was used for data entry and analysis. Quantitative data were presented by mean and SD, whereas qualitative data were presented by frequency distribution. The Chi-square test was used to compare between two or more proportions. The Student’s t test was used to compare two means. The lowest accepted level of significance was 0.05 or less.
Results
This study included 54 patients with either recurrent or complicated PSD, of whom 27 patients were treated with Karydakis flap and 27 with Limberg flap. Patients’ age ranged from 19 to 48 and the mean was 32 ± 7.9. Males were 40.7% and 44.4% in group A and group B respectively, while females were 59.3% and 55.6% respectively. No statistically significant differences were observed between the groups regarding age and sex (Table 1).
This study showed that the operative time in the Limberg group was 50.1 ± 14.4, whereas in the Karydakis group, it was 37.2 ± 8.9, and this difference was significantly different as shown in Table 2. Whereas, the differences between the two groups in term of length of hospital stay, postoperative analgesic needed, and duration of drainage were not statistically significant.
Regarding time of first mobilization and painless toilet setting, they are significantly shorter in the Limberg group (1 ± 0 and 1.4 ± 0.5 respectively). On the other hand, access to normal daily activity was shorter in the Karydakis group (17.2 ± 2.6) and these differences were statistically significant (Table 2).
The time of wound healing in the Karydakis group was 24.3 ± 3.4, whereas in the Limberg group, it was 25.8 ± 4.8; this was not a significant difference. The time taken to remove stitches in the Karydakis group was 15.3 ± 1.5, which is shorter the time taken in the Limberg group (17 ± 2.3), and this difference was significant as shown in Table 3.
Regarding postoperative complications, the occurrence of wound breakdown in the Karydakis group was 40.7% versus 11.1% in the Limberg group. No recurrence occurred in the Limberg group but recurrence observed in six cases in the Karydakis group. In the Karydakis group, eight patients had infection in comparison to one case in the Limberg group. All these differences were statistically significant (Table 3).
All patients have to lie prone postoperatively in limberg group to avoid flap necrosis for at least 2 weeks, whereas in the Karydakis group no need for that position. The overall patient satisfaction in the Limberg group was significantly higher than that in the Karydakis group (Table 3).
Discussion
Although several surgical methods have been defined for PSD treatment, no golden standard method is available yet. The present study compares the effectiveness of two procedures: Limberg flap and Karydakis flap in the surgical management of recurrent or complicated sacrococcygeal PSD. It was found that there is a significant differences between the groups in operative time, which is shorter in Karydakis operation. This is in agreement with Kohla et al. who found that duration of surgery in the Karydakis group was 37.73 ± 12.98, whereas in the Limberg group, it was 61.60 ± 11.11 [14]. However, there is no significant difference between the two groups regarding length of hospital stay which is not in accordance with Bostanoglu et al. who observed that hospital stay was shorter (3.0 ± 1.5 days) in Karydakis technique as compared to Limberg flap procedure (4.3 ± 1.5 days) [15].
In terms of remaining short term results, the current study shows that Karydakis operation is superior to Limberg operation regarding access to normal daily activity. This is in line with Karaca et al. [16]. After 12 months from follow-up, we had no recurrence in the Limberg group. However, six of 27 patients had recurrence in the Karydakis group and these cases suffered from postoperative seroma and wound infection as Arslan et al. reported that the appearance of seroma, hematoma, or wound infection in the early period increases the risk of recurrence of the disease [17], and this difference was statistically significant.
A Cochrane overview has been performed to provide evidence-based guidance for surgical treatment [18]. The review concluded that off-midline closure (including rhomboid, Karydakis, and Bascom flaps) is the best choice if the sinus is to be excised and sutured, and this closure is associated with shorter hospital stay and the lowest recurrence rates [19]. In the current study, cosmetic results did not differ between the studied groups. These findings were in coherence with Ashok and Nikhilesh who found no significant differences between the groups in cosmetic results [20]. However, patient satisfaction in the Limberg group was significantly higher than that in the Karydakis group, and this result is consistent with Alvandipour et al. [13].
Conclusion
It is concluded that Limberg flap rotation is clearly preferred in management of recurrent and complicated PNS for safety reasons given its low recurrence and postoperative complication rates. Karydakis technique is superior to Limberg flap regarding shorter operative time and shorter time needed for access to normal daily activity so it is preferred in uncomplicated PNS.
References
Petersen S, Koch R, Stelzner S, Wendlandt TP, Ludwig K (2002) Primary closure techniques in chronic pilonidal sinus: a survey of the result of different surgical approaches. Dis Colon Rectum 45(11):1458–1462
Bertelsen CA (2011) Cleft-lift operation for pilonidal sinuses under tumescent local anesthesia: a prospective cohort study of peri- and postoperative pain. Dis Colon Rectum 54(7):895e900
Muzi MG, Milito G, Cadeddu F, Nigro C, Andreoli F, Amabile D, Farinon AM (2010) Randomized comparison of Limberg flap versus modified primary closure for the treatment of pilonidal disease. Am J Surg 200(1):9–14
Krand O, Yalt T, Berber I, Kara VM, Tellioglu G (2009) Management of pilonidal sinus disease with oblique excision and bilateral gluteus maximus fascia advancing flap: result of 278 patients. Dis Colon Rectum 52:1172–1177
Can MF, Sevinc MM, Hancerliogullari O, Yilmaz M, Yagci G (2010) Multicenter prospective randomized trial comparing modified Limberg flap transposition and Karydakis flap reconstruction in patients with sacrococcygeal pilonidal disease. Am J Surg 200(3):318–327
Bessa SS (2013) Comparison of short-term results between the modified Karydakis flap and the modified Limberg flap in the management of pilonidal sinus disease: a randomized controlled study. Dis Colon Rectum 56(4):491–498
Humphries AE, Duncan JE (2010) Evaluation and management of pilonidal disease. Surg Clin North Am 90(1):113–124
Søndenaa K, Nesvik I, Andersen E, Natås O, Søreide JA (1995) Bacteriology and complications of chronic pilonidal sinus treated with excision and primary suture. Int J Color Dis 10:161–166
Lieto E, Castellano P, Pinto M, Zamboli A, Pignatelli C, Galizia G (2010) Dufourmentel rhomboid flap in the radical treatment of primary and recurrent sacrococcygeal pilonidal disease. Dis Colon Rectum 53(7):1061–1068
Mentes O, Bagci M, Bilgin T, Ozgul O, Ozdemir M (2008) Limberg flap procedure for pilonidal sinus disease: results of 353 patients. Langenbeck's Arch Surg 393:185–189
Lee PJ, Raniga S, Biyani DK, Watson AJ, Faragher IG, Frizelle FA (2008) Sacrococcygeal pilonidal disease. Color Dis 10(7):639–650
Ersoy E, Devay AO, Aktimur R, Doganay B, Ozdoğan M, Gundoğdu RH (2009) Comparison of the short-term results after Limberg and Karydakis procedures for pilonidal disease: randomized prospective analysis of 100 patients. Color Dis 11(7):705–710
Alvandipour M, Zamani MS, Ghorbani M, Charati JY, Karami MY (2019) Comparison of Limberg flap and Karydakis flap surgery for the treatment of patients with pilonidal sinus disease: a single-blinded parallel randomized study. Ann Coloproctol; 1–6
Kohla SM, Alsesy AA, Abd El-Aziz TF, Mohammed MA, Abo Zaid MA (2016) Comparative study between the Karydakis technique and the Limberg flap in pilonidal sinus. Menoufia Med J 29:539–544
Bostanoglu S, Sakcak I, Avsar FM, Cosgun E, Hamamci EO (2010) Comparison of Karydakis technique with Limberg flap procedure in pilonidal sinus disease: advantages of Karydakis technique. Pak J Med Sci 26(4):773–777
Karaca T, Yoldaş O, Bilgin BÇ, Ozer S, Yoldaş S et al (2012) Comparison of short-term results of modified Karydakis flap and modified Limberg flap for pilonidal sinus surgery. Int J Surg 10(10):601–606
Arslan K, Said Kokcam S, Koksal H, Turan E, Atay A, Dogru O. Which flap method should be preferred for the treatment of pilonidal sinus? A prospective randomized study. Tech
McCallum IJ, King PM, Bruce J (2008) Healing by primary closure versus open healing after surgery for pilonidal sinus: systematic review and meta-analysis. BMJ 336(7649):868–871. https://doi.org/10.1136/bmj.39517.808160.BE
Petersen S, Koch R, Stelzner S, Wendlandt TP, Ludwig K (2002) Primary closure techniques in chronic pilonidal sinus: a survey of the - results of different surgical approaches. Dis Colon Rectum 45(11):1458–1467. https://doi.org/10.1007/s10350-004-6451-2
Ashok, Nikhilesh (2018) Comparison of Karydakis flap and Limberg flap in pilonidal sinus. Int J Surg Surg Tech 2(2):1–4
Acknowledgments
The authors would like to offer their sincere thanks to all patients and their relevant.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
The protocol of the study was discussed and approved regarding ethics of research in the general surgical department. The study had been approved by the ethical committee for human studies in our institution. Full written, informed consent was signed from all participants.
Conflict of Interest
The authors declare that they have no conflicts of interest.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Manuscript has been read and approved by all the authors
Rights and permissions
About this article
Cite this article
Elhiny, A.A.H., Saad, D.A. & Farahat, M.S. Effectiveness and Feasibility of Limberg and Karydakis Flap in Recurrent and Complicated Pilonidal Sinus Disease. Indian J Surg 83, 55–60 (2021). https://doi.org/10.1007/s12262-020-02236-5
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12262-020-02236-5