Abstract
Pancreatic pseudocysts are one of the most frequent complications after acute pancreatitis occurring in up to 20% of cases. Majority of the pseudocysts less than 4 cm resolve in 6–8 weeks. Large pseudocysts in the pancreatic head can cause biliary or duodenal obstruction. However, acute jejunal obstruction due to pancreatic pseudocyst has been rarely reported. We present a case of gallstone-related acute pancreatitis resulting in pseudocyst formation causing acute jejunal obstruction. The patient was successfully treated by surgery.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Pancreatic pseudocysts are the most commonly encountered cystic lesions of the pancreas [1]. They develop due to the collection of amylase-rich fluid within or around the pancreas following acute or chronic pancreatitis. The prevalence of pseudocysts in acute pancreatitis varies from 6 to 18.5% and in chronic pancreatitis ranges from 20 to 40% [2, 3]. Most of the pseudocysts less than 4 cm resolve spontaneously within 6 to 8 weeks [2]. However, persistent large pseudocysts can lead to complications such as biliary obstruction, spontaneous rupture, bleeding, or duodenal obstruction. But acute jejunal obstruction due to pseudocyst in the pancreatic body and tail is rare. To the best of our knowledge, there is only one reported case of partial small bowel obstruction due to pancreatic pseudocyst in English literature [4].
Case Description
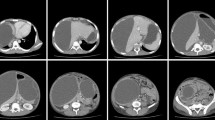
A 55-year-old male presented with a history of abdominal distension, constipation, and obstipation for 3 days. In the past, the patient had developed gallstone-related acute pancreatitis 2 years back which was managed conservatively. On examination, the abdomen was distended with the presence of hyper-peristaltic bowel sounds. The abdominal radiograph revealed multiple air-fluid levels suggestive of intestinal obstruction. The patient was resuscitated with intravenous fluids, nasogastric decompression, and antibiotics. Contrast-enhanced computed tomography (CECT) of the abdomen and pelvis revealed a pseudocyst of 9.3 × 7.8 × 9.8 cm involving the body and tail of the pancreas. The main pancreatic duct was not dilated. The proximal jejunal loops were dilated with an abrupt cutoff at the level of distal jejunum. The distal bowel loops were collapsed. The narrowed part of the jejunal loop was seen abutting the inferior aspect of the pseudocyst (Fig. 1). With the provisional diagnosis of adhesive intestinal obstruction, we prepared the patient for surgery and obtained written informed consent.
Intraoperatively, the pancreatic pseudocyst was bulging from the mesocolon into the infra-colic compartment. The distal jejunal loop was densely adhered to the pseudocyst causing intestinal obstruction (Fig. 2). On opening the pseudocyst, about 400 ml of sero-purulent fluid was drained. No solid debris was found. The adhered segment of the jejunal loop was separated from the cyst wall to relieve the obstruction. Due to the thin cyst wall, external drainage was performed. The operative time was 135 min with the blood loss of 100 ml. The postoperative course was uneventful with the hospital stay of 5 days. The drain was removed during the follow-up at 20 days. Until the last follow-up at 6 months after surgery, the patient was symptom-free.
Discussion
We report a rare complication of acute jejunal obstruction caused by pancreatic pseudocyst. In most cases, pancreatic pseudocysts are located in the supra-colic compartment due to which the jejunal loops do not come in direct contact with the cyst. Some pseudocysts extend into the infra-colic compartment and have adhesions with the jejunal loops. However, development of complete jejunal obstruction due to adhesions has not been reported.
In the present case, the adhesion between the inferior surface of the pseudocyst and the jejunal loop was very dense and wide leading to luminal compromise (Fig. 2). There are few reports of jejunal and colonic obstruction in the setting of acute pancreatitis [5, 6]. It is believed to occur due to retroperitoneal inflammation, thrombosis of mesenteric arteries, or ischemic necrosis of watershed areas [5, 6].
CECT is the imaging modality of choice for the diagnosis of pancreatic pseudocyst and its complications. In the present case, the pseudocyst and small bowel obstruction were accurately diagnosed on CECT.
With the advancements in endoscopic techniques and instrumentation, the pseudocysts are being increasingly managed by endoscopic drainage [7]. However, in the present case, we did not suspect pseudocyst as the cause of bowel obstruction preoperatively due to its rarity. Hence, we did not consider endoscopic decompression of the pseudocyst. Laparoscopic surgery has been found to be as effective as open surgery with faster recovery in experienced hands for the management of pancreatic pseudocyst [8]. However, in the present case, due to lack of surgical expertise in advanced laparoscopy and the presence of small bowel obstruction, we preferred open surgery. The drainage of the pseudocyst failed to relieve the intestinal obstruction. The adhered jejunal loop had to be separated from the cyst wall to relieve the obstruction.
In conclusion, an infra-colic extension of pancreatic pseudocyst can predispose to development of adhesions with the bowel loops leading to acute intestinal obstruction.
References
Khan A, Khosa F, Eisenberg RL (2011) Cystic lesions of the pancreas. AJR 196:W668–W677
Maringhini A, Uomo G, Patti R, Rabitti P, Termini A, Cavallera A, Dardanoni G, Manes G, Ciambra M, Laccetti M, Biffarella P, Pagliaro L (1999) Pseudocysts in acute nonalcoholic pancreatitis: incidence and natural history. Dig Dis Sci 44:1669–1673
Barthet M, Bugallo M, Moreira LS, Bastid C, Sastre B, Sahel J (1993) Management of cysts and pseudocysts complicating chronic pancreatitis. A retrospective study of 143 patients. Gastroenterol Clin Biol 17:270–276
Wilson C, Peterson S (2016) Pancreatic pseudocyst causing partial small bowel obstruction and cholangitis. J Emerg Med 50:493–494
Sunkara T, Etienne D, Caughey ME, Gaduputi V (2017) Small bowel obstruction secondary to acute pancreatitis. Gastroenterology Res 10:42–44
Pyun DK, Kim KJ, Ye BD, Byeon JS, Myung SJ, Yang SK, Kim JH, Yoon SN (2009) Two cases of colonic obstruction after acute pancreatitis. Korean J Gastroenterol 54:180–185
Sharma SS, Bhargawa N, Govil A (2002) Endoscopic management of pancreatic pseudocyst: a long-term follow-up. Endoscopy 34:203–207
Palanivelu C, Senthilkumar K, Madhankumar MV, Rajan PS, Shetty AR, Jani K, Rangarajan M, Maheshkumaar GS (2007) Management of pancreatic pseudocyst in the era of laparoscopic surgery-experience from a tertiary centre. Surg Endosc 21:2262–2267
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of Interest
The authors declare that they have no conflict of interest.
Patient Consent
Informed consent was taken from the patient for case publication.
Article Guarantor
Rahul Gupta
Additional information
Poster Presentation
This article was presented as poster in the 48th Annual Congress of the Korean Association of HBP surgery (HBP Surgery Week 2018)
Rights and permissions
About this article
Cite this article
Gupta, R., Singh, A.K. & Verma, P. Acute Small Bowel Obstruction Secondary to a Pancreatic Pseudocyst. Indian J Surg 81, 391–393 (2019). https://doi.org/10.1007/s12262-018-1845-x
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12262-018-1845-x