Abstract
The objective of this study was to evaluate the age distribution, mode of injury, type of hematomas, and their surgical outcome in patients with bilateral traumatic head injuries. The present study included 669 cases of traumatic head injury who presented at the neurosurgery emergency out of which 94 cases had bilateral head injuries from the period of August 2009 to April 2014. The data from the hospital computerized database were retrospectively analysed. Cases of bilateral traumatic head injury included 94 patients out of which 88.29 % (n = 83) were males and 11.70 % (n = 11) were females. Commonest mode of injury was road traffic accident in 56.38 % (n = 53) followed by fall from height in 29.78 % (n = 28). In our study, 25.53 % patients had epidural hematoma (EDH) with intracerebral hematoma (ICH) or contusion (n = 24), followed by EDH with subarachnoid hemorrhage (SAH) in 18.08 % (n = 17). At the time of discharge, all those patients managed conservatively had good Glasgow outcome scale (GOS) while with surgical intervention 58 % patients had good GOS, 19 % had moderate disability, and 9 % remained with severe disability. In cases of bilateral hematomas, EDH is most common and should be managed in neurosurgical emergency. Other combinations of bilateral intracranial hematomas should be managed according to the surgical indication and serial CT imaging.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Hematomas within the cranium are life-threatening emergencies. Following traumatic head injury, the accumulated blood leads the raised of intracranial pressure, which damages the brain and can lead to permanent vegetative state or death. Traumatic intracranial hematomas are classified into four categories: epidural hematoma, subdural hematoma, subarachnoid hemorrhage, and intracerebral hematoma [1, 2]. Not much literature is available on traumatic bilateral intracranial hematomas as resources are limited in our developing country.
Traumatic head injuries affect 2 % of population and are the major cause of death among young people. Most severe complication of traumatic head injury is intracranial hematoma which comprises of 25–45 % of traumatic head injuries [3]. With Pubmed advanced search, we found only a handful of published articles on bilateral surgery following traumatic head injury [4–11].
We retrospectively analysed the 669 cases of traumatic head injures admitted at our hospital over a period of 4 years and 9 months. Out of the 669 reported cases of traumatic head injuries, 94 patients had bilateral traumatic head injuries. We also evaluated the age distribution, mode of injury, type of hematomas, and their surgical outcome in these bilateral traumatic head injury cases.
Materials and Methods
The present study was conducted at the Department of Neurosurgery, Institute of Medical Sciences, Sir Sunder Lal Hospital, Banaras Hindu University from August 2009 to April 2014. During this period, 669 cases of traumatic head injuries presented at the emergency setting out of which 94 cases reported with bilateral head injuries. These 94 cases were then further analysed in terms of age, mode of injury, type of hematomas/CT findings, operative management, and outcome at our medical facility. The study excluded bilateral traumatic head injuries following trauma to sagittal sinus, non-traumatic chronic subdural hematoma, intracranial hematoma secondary to spontaneous hemorrhage, and patients below 5 years of age.
Observations and Results
The present retrospective study included 669 cases out of which 14.05 % (n = 94) patients had bilateral traumatic head injury. Cases of bilateral traumatic head injury included patients aged between 6 and 78 years comprising of 88.29 % (n = 83) males and 11.70 % (n = 11) females. Male to female ratio was 7.54:1. Commonest age group was 16–25 years in 29.78 % (n = 28), followed by 26–35 years in 22.34 % (n = 21) (Table 1). Commonest mode of injury was road traffic accident in 56.38 % (n = 53) followed by fall from height in 29.78 % (n = 28) (Table 2). In this retrospective analysis of bilateral head injuries, maximum patients had epidural hematoma (EDH) with intracerebral hematoma (ICH) or contusion in 25.53 % (n = 24), followed by EDH with SAH which comprised of 18.08 % (n = 17) of the patients. Other combinations of bilateral hematomas reported were EDH with EDH in 11.70 % (n = 11), EDH with SDH in 3.19 % (n = 3), SDH with SDH in 2.12 % (n = 2), SDH with subarachnoid hemorrhage (SAH) in 10.63 % (n = 10), ICH with SDH in 8.51 % (n = 8), ICH with ICH in 13.82 % (n = 13), and SAH with SAH in 6.38 % (n = 6) (Table 3).
All patients with bilateral head injuries had associated injuries, viz. skull bone fracture while few patients also had abdominal injury, chest injury, spinal injury, etc. All patients with bilateral intracranial hematomas were operated in the emergency department except patients with bilateral subarachnoid hemorrhage and small hematoma with no midline shift with GCS score 13 and above who were managed conservatively. In some patients who were managed conservatively, obliteration of cisterns and effacement of cortical sulci, were present. Evacuation of hematoma in cases with EDHs was managed by trephine craniotomy or craniectomy, acute on chronic SDH by burr hole craniotomy, ICH/contusion by burr hole craniotomy or craniectomy, and acute SDH by decompressive craniectomy. At the time of discharge, all those patients managed conservatively had good Glasgow outcome scale (GOS) while those with surgical intervention had 58 % patients with good GOS, 19 % with moderate disability, and 9 % remained with severe disability. Also, 11 % patients were referred to various other departments for further management and 3 % died (Fig. 1).
Discussion
All intracranial hematomas have some common clinical features, viz. headache, nausea, vomiting, confusion, or seizures. At the time of presentation, patient may be alert, drowsy, or moribund on general physical examination. Importantly, older age and drugs like anticoagulants predispose to large intracranial hematoma even with minor head trauma. Epidural and subdural hematomas are the most common intracranial hematomas as a consequence of traumatic head injury [1].
In traumatic head injury, multiple intracranial hematomas are a common phenomenon [12, 13].
Besides locating the hematoma, CT imaging also helps in detecting other features such as midline shift, skull bone fracture, basal cistern obliteration, and volume and type of hematomas which influence the management strategy.
In this study, analysis showed that the maximum number of the patients were in the most productive stages of life, i.e., second and third decade, approximately 54 % (n = 56). Only 9.6 % (n = 10) patients were above the age of 55 years. Similar were the finding in other studies which reported second decade to be the most commonly affected [14–16]. In this study, wide gap in the male to female ratio can be attributed to lesser outdoor activities of females, lesser involvement in driving vehicles, and male-dominated society with all outdoor responsibilities leading to more movement for socioeconomic purposes and drunken driving.
Similar to other published studies, road traffic accidents (RTA) was found to be the most common cause of head injury in this study [16, 17]. In children, fall from height was found to be the commonest cause of head injury. In most of the studies on bilateral head injuries, surgeries reported were bifrontal craniotomies [18] or contralateral removal of a hematoma after evacuation of an intracranial hematoma [4, 9, 19, 20].
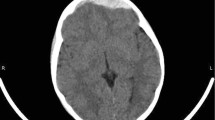
In our study, most common bilateral hematoma was EDH with ICH or contusion for which bilateral craniectomy with evacuation of hematoma was done (Fig. 2a,b,c) followed by EDH with SAH. Other combinations of bilateral hematomas reported were EDH with EDH, EDH with SDH, SDH with SDH, SDH with SAH, ICH with SDH, ICH with ICH, and SAH with SAH (Fig. 2).
a, b, c Preoperative and postoperative CT image of a large epidural hematoma in the left temporoparietal area and intracerebral hematoma in the right temporal lobe. d, e, f, g, h, i, j, k Various combinations of bilateral traumatic intracerebral hematomas EDH with EDH, ICH/contusion with ICH/contusion,SAH with EDH, SAH with SAH, SAH with SDH, SDH with ICH/contusion, acute on chronic SDH with SDH, and EDH with ICH
Depending on the clinical status and type of injury, management of bilateral hematoma needs to be planned. EDH evacuation helps in improving the prognosis in bilateral intracranial hematomas. Any delay in evacuation of a contralateral EDH can result into postoperative neurological deficit and even death [4]. Most cases of bilateral hematomas with dural artery damage have no midline shift, and EDH can develop on removing the contralateral hematoma because of the release of a pressure effect which further aggravates brain injury. Thus, EDH evacuation should be done on priority in cases of bilateral intracranial hematomas. Trephine craniotomy or craniectomy should be done for the evacuation of EDH and then either simultaneously or later small craniotomy or burr hole for contralateral intracranial hematoma evacuation as per the serial CT evaluation should be done. In cases of traumatic acute on chronic SDH, burr hole craniotomy is sufficient for bilateral intracranial hematomas. But in cases of acute SDH with ICH or EDH, decompressive craniectomy should be attempted for acute SDH. During SDH removal, if brain matter swells, postoperative CT scan should be done to rule out any contralateral EDH, which if present demands craniotomy [6, 10, 21]. EDH evacuation helps in improving prognosis in bilateral intracranial hematomas. After evacuation of hematoma on one side, delayed evacuation of a contralateral EDH can result into postoperative neurological deficit and even death [4]. In case of bilateral ICH, after operating on one side, the contralateral intracranial hematoma should be reevaluated by CT scan. Intraoperative CT scan if available is valuable in detecting any change in lesion characteristics [22]. However, in developing countries like India, facility for intraoperative imaging is not available at most of the treatment facilities.
Conclusion
In cases of bilateral hematomas, EDH is most common and should be managed in neurosurgical emergency as early as possible to reduce the potential morbidity and mortality. Other combinations of bilateral intracranial hematomas should be managed according to the surgical indication and serial CT imaging. In developing country like ours, with limited resources, poor patient economic status, and time delay in reaching the nearest medical facility, managing bilateral hematomas is a big challenge as urgent neurosurgical intervention is required. Taking care of these hindrances in developing countries, besides reducing the mortality, we can manage to limit the postoperative neurological deficit which is again another challenge for patient’s whole life.
References
Oliver Z. Intracranial hemorrhage. In: Senecal E. CDEM self study modules Neurologic emergencies. Boston, Massachusetts:Harvard Medical School. Available from: http://www.cdemcurriculum.org/ssm/neurologic/ich/ich.php.
Ono J, Yamaura A, Kubota M, Okimura Y, Isobe K (2001) Outcome prediction in severe head injury: analyses of clinical prognostic factors. J Clin Neurosci 8:120–3
Thurman D, Guerrero J (1999) Trends in hospitalization associated with traumatic brain injury. JAMA 282(10):954–7
Shen J, Pan JW, Fan ZX, Zhou YQ, Chen Z, Zhan RY (2013) Surgery for contralateral acute epidural hematoma following acute subdural hematoma evacuation: five new cases and a short literature review. Acta Neurochir (Wien) 155:335–41
Fridley J, Thomas J, Kitagawa R, Chern J, Omeis I (2011) Immediate development of a contralateral acute subdural hematoma following acute subdural hematoma evacuation. J Clin Neurosci 18:422–3
Matsuno A, Katayama H, Wada H, Morikawa K, Tanaka K, Tanaka H et al (2003) Significance of consecutive bilateral surgeries for patients with acute subdural hematoma who develop contralateral acute epi-or subdural hematoma. Surg Neurol 60:23–30
Rochat P, Johannesen HH, Poulsgård L, Bøgeskov L (2002) Sequentially evolved bilateral epidural haematomas. Clin Neurol Neurosurg 105:39–41
Shen J, Pan JW, Fan ZX, Zhou YQ, Chen Z, Zhan RY (2013) Surgery for contralateral acute epidural hematoma following acute subdural hematoma evacuation: five new cases and a short literature review. Acta Neurochir (Wien) 155:335–41
Su TM, Lee TH, Chen WF, Lee TC, Cheng CH (2008) Contralateral acute epidural hematoma after decompressive surgery of acute subdural hematoma: clinical features and outcome. J Trauma 65:1298–302
Yagüe LG, Rodríguez-Sánchez J, Polaina M, Porras LF, Lorenzana L, Cabezudo JM (1991) Contralateral extradural hematoma following craniotomy for traumatic intracranial lesion. Case report. J Neurosurg Sci 35:107–9
Kompheak H, Hwang SC, Kim DS, Shin DS, Kim BT (2014) Surgery for bilateral large intracranial traumatic hematomas: evacuation in a single session. J Korean Neurosurg Soc 55(6):348–52. doi:10.3340/jkns.2014.55.6.348
Eisenberg HM, Gary HE Jr, Aldrich EF, Saydjari C, Turner B, Foulkes MA et al (1990) Initial CT findings in 753 patients with severe head injury. A report from the NIH Traumatic Coma Data Bank. J Neurosurg 73:688–98
Zimmerman RA, Bilaniuk LT, Gennarelli T, Bruce D, Dolinskas C, Uzzell B (1978) Cranial computed tomography in diagnosis and management of acute head trauma. AJR Am J Roentgenol 131:27–34
Bullock MR, Chesnut R, Ghajar J, Gordon D, Hartl R, Newell DW (2006) Surgical management of acute epidural haematomas. Neurosurgery 58(3 Suppl):S7–15, discussion Si-iv
Haselsberger K, Pucher R, Auer L (1988) Prognosis after acute subdural or epidural haemorrhage. Acta Neurochir (Wien) 90:111–6
Meier U, Heinitz A, Kintzel D (1994) Surgical outcome after severe craniocerebral trauma in childhood and adulthood. A comparative study. Unfallchirurg 97:406–9 (in German)
Wester K (1999) Decompressive surgery for pure epidural hematomas: does neurosurgical expertise improve the outcome? Neurosurgery 44:495–500
Polin RS, Shaffrey ME, Bogaev CA, Tisdale N, Germanson T, Bocchicchio B et al (1997) Decompressive bifrontal craniectomy in the treatment of severe refractory posttraumatic cerebral edema. Neurosurgery 41:84–94
Milo R, Razon N, Schiffer J (1987) Delayed epidural hematoma. A review. Acta Neurochir (Wien) 84:13–23
Rochat P, Johannesen HH, Poulsgård L, Bøgeskov L (2002) Sequentially evolved bilateral epidural haematomas. Clin Neurol Neurosurg 105:39–41
Feuerman T, Wackym PA, Gade GF, Lanman T, Becker D (1988) Intraoperative development of contralateral epidural hematoma during evacuation of traumatic extraaxial hematoma. Neurosurgery 23:480–4
Huang AP, Chen YC, Hu CK, Lin TK, Huang SJ, Tu YK et al (2011) Intraoperative sonography for detection of contralateral acute epidural or subdural hematoma after decompressive surgery. J Trauma 70:1578–9
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Ethical committee clearance was obtained before the start of the study.
Conflict of Interest
The authors declare that they have no competing interests.
Rights and permissions
About this article
Cite this article
Pandey, S., Sharma, V., Singh, K. et al. Bilateral Traumatic Intracranial Hematomas and its Outcome: a Retrospective Study. Indian J Surg 79, 19–23 (2017). https://doi.org/10.1007/s12262-015-1416-3
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12262-015-1416-3