Abstract
Our primary objective in this study was to determine the preferred strength setting for the sinogram-affirmed iterative reconstruction algorithm (SAFIRE) in abdominal computed tomography (CT) imaging. Sixteen consecutive clinical CT scans of the abdomen were reconstructed by use of traditional filtered back projection (FBP) and 5 SAFIRE strengths: S1–S5. Six readers of differing experience were asked to rank the images on preference for overall diagnostic quality. The contrast-to-noise ratio was not significantly different between SAFIRE S1 and FBP, but increased with increasing SAFIRE strength. For pooled data, S2 and S3 were preferred equally but both were preferred over all other reconstructions. S5 was the least preferred, with FBP the next least preferred. This represents a marked disparity between the image quality based on quantitative parameters and qualitative preference. Care should be taken to factor in qualitative in addition to quantitative aspects of image quality when one is optimizing iterative reconstruction images.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
1 Introduction
Computed tomography (CT) of the abdomen is one of the most widely utilized radiologic modalities and, as such, is a considerable source of medical exposure to ionizing radiation [1]. Reducing tube current settings as a means of reducing radiation exposure typically results in increased image noise with the traditional filtered back projection (FBP) image reconstruction technique [2, 3]. Iterative reconstruction is an alternative reconstruction technique which produces a reduced level of image noise at lower radiation doses compared to those of FBP [4, 5]. Although iterative reconstruction (IR) software generates images with less noise than that of FBP, it often leads to undesirable images [4, 5]. For improvement of this shortcoming, software has been designed that blends IR and FBP images [6]. The sinogram-affirmed iterative reconstruction algorithm (SAFIRE) describes this technique as different “strength” settings of the IR [7]. The goal is to achieve a better balance between noise reduction and image appearance, in particular, the excessively blocky and pixilated appearance [7]. However, studies have not yet clearly identified the optimum strength settings for SAFIRE in abdominal CT. One primary purpose in this study was to assess for the optimal strength setting of SAFIRE for readers of abdominal CT images, in regard to both qualitative and quantitative image quality measures.
2 Materials and methods
2.1 Subjects
The local institutional review board approved this retrospective, single-center study with a waiver of written informed consent. This was a Health Insurance Portability and Accountability Act compliant study. Sixteen consecutive CT scans which had been performed on the same CT scanner with identical radiation emission settings were chosen for inclusion in the study. Images were viewed without identifiable patient data.
2.2 CT technique
All examinations were performed on a single 64 slice Siemens SOMATOM Definition Flash scanner. Routine radiation emission settings on this scanner for abdominal CT were 100 kV and 150 mAs with automatic exposure control settings employed. Radiation settings as well as radiation dose reports are routinely archived with each patient image set. For this study, we recorded the Volume Computed Tomography Dose Index (CTDIvol), which is a standardized parameter for measurement of the scanner radiation output in mGy.
For the analysis, six image reconstructions were performed from the raw CT data for each acquisition: SAFIRE reconstruction strengths 1–5 as well as conventional FBP. All data sets were reconstructed with a slice thickness of 5 mm.
2.3 Quantitative image evaluations
The contrast-to-noise ratio (CNR) was measured by a single observer for all image sets. The level of image contrast was obtained from the difference in mean Hounsfield units (HU) measurement of two regions of interest (ROI), one placed over the liver parenchyma and the other over the portal vein. This was divided by the noise level from an ROI recording the standard deviation of the mean HU drawn no <10 mm2 in area and no >20 mm2 within the subcutaneous fat posterior to the latissimus doris at the level of the umbilicus. Patient size was recorded as the sum of the maximum anterior–posterior (AP) and lateral measurements (in cm) at the same level as that of the image noise evaluation (umbilicus level).
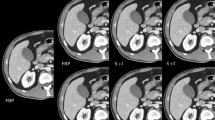
2.4 Qualitative image evaluations
All abdominal CT images were viewed on a Siemens Syngo workstation. For each image set, the 6 image reconstructions were available for review (Fig. 1). Six separate readers of differing experience in the interpretation of abdominal CT were asked to review each dataset and rank their preference for the individual image reconstructions based on the overall appearance desired for clinical interpretation. The readers were not given a specific diagnostic task, but rather were asked to assess all aspects of the image quality expected for a routine clinical case. The first reader was a first year radiology resident, who had no prior experience interpreting abdominal CT. The second reader was a second year radiology resident with 1 year of experience in CT of the abdomen. The third reader was a third year radiology resident, having had an estimated 2 years of experience in abdominal CT. The fourth reader was an attending radiologist with 6 years total of abdominal CT experience. The fifth was an attending radiologist with 10 years of experience, and the sixth was an attending radiologist with 34 years of experience in abdominal CT. The readers were instructed not to change the window level/width settings which had been sent from the CT scanner. They were identical settings typical for abdominal CT viewing. Readers were asked to rank the individual reconstructed image datasets for each patient examination with a value of ‘1’ for their most preferred and ‘6’ for their least preferred.
2.5 Statistical analysis
The Mann–Whitney U test was used for assessment of the nonparametric continuous variables, particularly relating to quantitative image quality measures (significance was set at p < 0.05). The Kruskal–Wallis test was used for comparison of ordinal ranked data including for assessment of the preference of the different reconstruction techniques (significance was set at p < 0.05).
3 Results
The median patient size (AP + lateral dimension) was 56 cm (range 45–80 cm). For these patients, the median radiation dose (CTDIvol) was 7 mGy (range 4–18 mGy). The relationship between patient size and radiation exposure was one of direct proportionality, as expected with the use of automatic exposure control (Fig. 2).
The average noise for the FBP reconstruction was 18.5 ± 4.1, which was not significantly different from the noise of S1, 18.8 ± 3.9 (p = 0.79). However, the noise decreased with increasing SAFIRE strength: S2 = 16.5 ± 3.5, S3 = 14.7 ± 3.5, S4 = 12.8 ± 3.6, S5 = 10.9 ± 3.3. Also, the rate of decrease in noise was roughly constant between all strength settings. Based on the CNR, the contrast level for each SAFIRE setting (and FBP) in each subject was identical. Therefore, the highest CNR was observed in the S5 reconstruction (6.4 ± 1.6) and the lowest in both FBP (3.8 ± 1.8) and S1 (3.7 ± 1.9), which were not significantly different from each other (p = 0.71). The CNR values were: S2 = 4.2 ± 1.7, S3 = 4.8 ± 1.7, and S4 = 5.5 ± 1.6.
Despite the trend toward increasing CNR with increasing SAFIRE strength, the pooled preference scores (ranked as lowest to highest) for the readers identified low to intermediate strength settings as the most preferred and the highest strength SAFIRE as least preferred. For pooled data, the preference values for each reconstruction were: FBP = 4.6 ± 1.5, S1 = 3.5 ± 1.3, S2 = 2.0 ± 1.0, S3 = 2.0 ± 1.1, S4 = 3.5 ± 1.2, S5 = 5.7 ± 0.6. The individual raw score data are reported in Table 1. Specifically, the highest strength setting (S5) was the least preferred by all readers (although for one reader, S5 and FBP were statistically equally least preferred). FBP was generally less preferred by most readers in comparison to the low to intermediate strength SAFIRE settings, although one reader had a noticeably higher preference for FBP than did the other readers. Interestingly, there was a statistically significant observation that even though the lowest SAFIRE setting (S1) had a CNR (and noise level) identical to that of as FBP, S1 was rated consistently as preferred (p < 0.01).
4 Discussion
The results of this study suggest that a low to intermediate strength of the SAFIRE iterative reconstruction setting is preferred by radiologists of all experience levels over higher strength SAFIRE settings. This finding is in contradistinction to the finding that the CNR improved with increasing SAFIRE strength. Therefore, this study serves to highlight the importance of qualitative image evaluations in the assessment of optimal image settings, and not simply using quantitative measures. In addition, low to intermediate strength SAFIRE was significantly preferred to FBP based on pooled data, although the degree of preference was variable among readers. Importantly, the results of this study corroborate the results of recently performed studies on variable strength SAFIRE settings for other organ systems [8–10]. Therefore, the low to intermediate SAFIRE settings are likely to be an optimal choice regardless of the body part being imaged.
The level of reader experience had very little impact on the SAFIRE setting preference, suggesting that the preference for the appearance of clinical images is likely to be a durable finding and unlikely to be based simply on the appearance of images, one has become used to viewing. However, a follow-up longitudinal study may be of benefit in assessing whether the less-experienced readers maintain their preference for SAFIRE strength or whether they change their preference.
Most previously available iterative reconstruction techniques for CT did not have the ability to provide a hybrid image of IR and FBP. Images reconstructed entirely with an iterative technique led to an image with an extremely sharp transition between regions with differing contrast, causing a pixilated and overly blotchy appearance which was unfamiliar and therefore often undesirable to the reader [4, 7, 11, 12]. With SAFIRE, this ability to blend the images results in different strength settings, which have a greater iterative reconstruction component with increasing strength. This offers readers the ability to balance noise reduction and undesirable image smoothing. Despite the fact that a higher SAFIRE strength results in lower noise, the images produced may be considered suboptimal for diagnostic purposes, as suggested by the results of this study.
Despite the large differences in reader experience, there was a clear trend in this study for the intermediate strength reconstruction settings (S2 and S3) being preferred over both the lower and higher strengths (S1, S4, and S5) and traditional FBP in low-dose abdominal CT. Whereas it could be suggested that experienced readers may desire lower strength settings, which are more similar to the FBP images to which they are accustomed, the preference for intermediate strength was also seen in the entirely inexperienced reader, who would be unbiased by prior experience with FBP. This suggests that intermediate strength settings provide the appropriate balance between noise reduction and image smoothing regardless of personal preferences. Interestingly, the readers also preferred S1 to FBP, despite the fact that these had no significant difference in image noise or CNR. This clearly indicates that there is no direct correlation between noise and subjective image quality. Also, high strength SAFIRE (S5) was the least preferred, indicating the value of variable strength settings in iterative reconstruction techniques.
In conclusion, low to intermediate strength settings of SAFIRE (S2, S3) are recommended for low-mGy abdominal CT over both FBP and high strength SAFIRE (S5). Further, the image reconstruction preference was not correlated with the CNR. Thus, the CNR should not be used alone as the basis for assessment of image quality.
References
International Commission on Radiological Protection (ICRP). Managing patient dose in multi-detector computed tomography (MDCT). ICRP Publication 102. Ann ICRP. 2007;37(1):1–79.
Kalender WA. X-ray computed tomography. Phys Med Biol. 2006;51(13):R29–43.
Defrise M, Gullberg GT. Image reconstruction. Phys Med Biol. 2006;51(13):R139–54.
Kalra MK, Woisetschlager M, Dahlstrom N, et al. Radiation dose reduction with sinogram affirmed iterative reconstruction technique for abdominal computed tomography. J Comput Assist Tomogr. 2012;36:339–46.
Sarabjeet S, Mannudeep K, Jiang H, et al. Abdominal CT: comparison of adaptive statistical iterative and filtered back projection reconstruction techniques. Radiology. 2010;257:373–83.
Deak Z, Grimm JM, Treitl M. Filtered back projection, adaptive statistical iterative reconstruction, and a model-based iterative reconstruction in abdominal CT: an Experimental clinical study. Radiology. 2013;266:197–206.
Wen JE, Fu HY, Bo L, et al. Can sinogram-affirmed iterative (SAFIRE) reconstruction improve imaging quality on low-dose lung ct screening compared with traditional filtered back projection (FBP) reconstruction? J Comput Assist Tomogr. 2013;37:301–5.
Wang R, Schoepf UJ, Wu R, Nance JW Jr, Lv B, Yang H, Li F, Lu D, Zhang Z. Diagnostic accuracy of coronary CT angiography: comparison of filtered back projection and iterative reconstruction with different strengths. J Comput Assist Tomogr. 2014;38((2):179–84.
Wuest W, May MS, Scharf M, Layritz C, Eisentopf J, Ropers D, Pflederer T, Uder M, Achenbach S, Lell MM. Stent evaluation in low-dose coronary CT angiography: effect of different iterative reconstruction settings. J Cardiovasc Comput Tomogr. 2013;7(5):319–25.
Hwang HJ, Seo JB, Lee HJ, Lee SM, Kim EY, Oh SY, Kim JE. Low-dose chest computed tomography with sinogram-affirmed iterative reconstruction, iterative reconstruction in image space, and filtered back projection: studies on image quality. J Comput Assist Tomogr. 2013;37(4):610–7.
Pontana F, Pagniez J, Duhamel A, et al. Reduced dose low voltage chest CT angiography with sinogram affirmed iterative reconstruction versus standard dose filtered back projection. Radiology. 2013;267:609–18.
Hara AK, Paden RG, Silva AC, Kujak JL, Lawder HJ, Pavlicek W. Iterative reconstruction technique for reducing body radiation dose at CT: feasibility study. AJR Am J Roentgenol. 2009;193(3):764–71.
Conflict of interest
The authors declare that they have no conflict of interest.
Author information
Authors and Affiliations
Corresponding author
About this article
Cite this article
Hardie, A.D., Nelson, R.M., Egbert, R. et al. What is the preferred strength setting of the sinogram-affirmed iterative reconstruction algorithm in abdominal CT imaging?. Radiol Phys Technol 8, 60–63 (2015). https://doi.org/10.1007/s12194-014-0288-8
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12194-014-0288-8