Abstract
In cohort C of the phase 2 MM-014 trial, the efficacy and safety of pomalidomide, dexamethasone, and daratumumab therapy were investigated in 18 Japanese patients with relapsed/refractory multiple myeloma (RRMM) after their most recent regimen of lenalidomide-based therapy (NCT01946477). Patients received oral pomalidomide (4 mg daily), oral dexamethasone (20–40 mg weekly), and intravenously infused daratumumab (16 mg/kg). Median age was 67.5 years. All patients received prior lenalidomide per protocol; 89% received prior bortezomib. Twelve patients (67%) had lenalidomide-refractory disease, and 6 (33%) had lenalidomide-relapsed disease. Ten patients (56%) had only 1 prior treatment line. As of August 3, 2020, 15 patients (83%) were still on treatment; median follow-up was 8.1 months. Three patients (17%) discontinued treatment (2 for adverse events; 1 for major protocol deviation). Overall response rate (primary endpoint) was 83% (very good partial response or better, 61%). All patients had ≥ 1 grade 3/4 treatment-emergent adverse events, most commonly neutropenia (78%; febrile, 6%), leukopenia (28%), and lymphopenia (22%). Grade 3/4 infections occurred in 17%; 11% had pneumonia. In Japanese patients with RRMM, a triplet regimen of pomalidomide, dexamethasone, and daratumumab after early-line lenalidomide treatment failure showed high efficacy and safety consistent with the known safety profile.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Recent advances in multiple myeloma (MM) therapy have resulted in improved outcomes, yet the disease remains incurable, and nearly all patients will relapse after initial treatment [1, 2]. Lenalidomide-based therapy until disease progression is a standard of care for patients with newly diagnosed MM [3, 4]. As a result, most patients will have exhausted the benefits of lenalidomide at the time of first relapse. Although a number of treatment options are available for subsequent therapy, most studies do not include large lenalidomide-exposed or -refractory patient populations [5]. An important goal for any antimyeloma regimen in this setting is to delay relapse; patient outcomes worsen with every relapse, and the time between relapses becomes shorter with each successive line of treatment [1, 2, 5,6,7,8,9].
Pomalidomide is an oral immunomodulatory agent with immune-stimulating and direct tumoricidal activities [10]. In preclinical studies, pomalidomide was shown to decrease myeloma cell proliferation and reduce tumor volume in xenograft mouse models, specifically in the context of lenalidomide resistance [11, 12]. Importantly, in clinical trials, maintaining continuous immunomodulation with pomalidomide has also demonstrated clinical benefit in patients with lenalidomide-refractory disease [13,14,15,16]. In Japan, pomalidomide is approved for patients with relapsed or refractory MM (RRMM) whose disease did not respond to ≥ 1 standard treatment or relapsed after treatment; also, pomalidomide is recommended by the Japanese Society of Hematology guidelines as a salvage therapy for Japanese patients with RRMM [17, 18]. Currently, the Japanese Society of Hematology guidelines recommend doublet combination with dexamethasone or triplet combination with carfilzomib or bortezomib and dexamethasone as a salvage therapy with pomalidomide, although the combination with pomalidomide, carfilzomib, and dexamethasone is not approved in Japan [17, 19]. Daratumumab, an anti-CD38 monoclonal antibody, is also recommended in Japan as salvage therapy for patients with RRMM, but at this time, there is no recommendation to combine daratumumab with pomalidomide. Approved daratumumab combinations for Japanese patients with RRMM include daratumumab with dexamethasone and lenalidomide, bortezomib, or carfilzomib [20].
MM-014 is a phase 2, international, multicenter, nonrandomized trial investigating the outcomes of sequencing pomalidomide-based therapy immediately after lenalidomide-based treatment failure in patients with RRMM (NCT01946477). In an interim analysis (median follow-up, 17.2 months), the triplet combination of pomalidomide, dexamethasone, and daratumumab demonstrated an overall response rate (ORR) of 77.7% (76.2% in lenalidomide-refractory patients) in patients from the US and Canada (MM-014 DPd cohort; cohort B) who had received 1 or 2 prior lines of treatment [15]. At 1 year, 75.1% of patients were alive and had not experienced disease progression. The reported safety profile for this triplet regimen was consistent with the known toxicities of the individual agents. As an amendment to the MM-014 study, the efficacy and safety of this regimen was investigated in Japanese patients (cohort C) who were previously treated with a lenalidomide-containing regimen. This report describes the interim results of 18 patients treated in cohort C.
Materials and methods
Study design and patients
MM-014 is an open-label clinical trial with 3 cohorts conducted at 49 study sites in the United States, Canada, and Japan. Patients in cohort A received pomalidomide plus low-dose dexamethasone. Patients in cohort B (Canada and US) and cohort C (Japan) received pomalidomide, low-dose dexamethasone, and daratumumab. This analysis focuses only on cohort C. Patients were not simultaneously allocated across cohorts; rather, cohort B was added to the trial via protocol amendment after the full accrual of cohort A, and cohort C was added after the full accrual of cohort B. Data from cohorts A and B have been published [14,15,16].
Patients eligible for inclusion in cohort C were ≥ 18 years of age with a documented MM diagnosis, measurable disease (serum M-protein ≥ 0.5 g/dL or urine M-protein ≥ 200 mg/day) or involved free light-chain levels ≥ 100 mg/L, and Eastern Cooperative Oncology Group performance status ≤2. In addition, patients must have received 1 or 2 prior lines of treatment with a lenalidomide-containing regimen. Patients with disease that relapsed after or was refractory to lenalidomide were eligible for inclusion. Refractory disease was defined as being nonresponsive to therapy or experiencing disease progression within 60 days of the last dose of lenalidomide.
Key exclusion criteria for cohort C included prior treatment with pomalidomide or daratumumab, or hypersensitivity to thalidomide, lenalidomide, dexamethasone, or monoclonal antibodies. The following laboratory abnormalities were exclusionary criteria: absolute neutrophil count < 1 × 109/L, platelet count < 75 × 109/L (< 30 × 109/L for patients in whom ≥ 50% of bone-marrow nucleated cells were plasma cells), corrected serum calcium > 2.875 mmol/L (11.5 mg/dL), hemoglobin < 80 g/L (4.9 mmol/L), aspartate aminotransferase or alanine transaminase > 3.0 × upper limit of normal, serum total bilirubin > 34.2 μmol/L (2.0 mg/dL) or 3.0 × upper limit of normal, and severe renal impairment (creatinine clearance < 30 mL/min or requiring dialysis). Patients were also excluded if they had received an allogeneic bone-marrow or peripheral blood stem cell transplant < 12 months prior to study entry and had not discontinued immunosuppressive treatment ≥ 4 weeks prior to study initiation.
This study was carried out in accordance with the principles of the Declaration of Helsinki and the International Conference on Harmonisation Guideline E6 for Good Clinical Practice. The study received approval from each institution’s review board or independent ethics committee prior to study initiation and was carried out in accordance with applicable national, state, and local laws. Patients signed an informed consent document prior to undergoing any study related procedures.
All patients were treated with open-label pomalidomide, dexamethasone, and daratumumab using the following schedule for a 28-day treatment cycle: pomalidomide 4 mg/day was administered orally on days 1–21; oral dexamethasone 40 mg/day in patients aged ≤ 75 years or 20 mg/day in patients aged > 75 years was administered on days 1, 8, 15, and 22; and daratumumab was administered as an intravenous infusion at a starting dose of 16 mg/kg on days 1, 8, 15, and 22 during cycles 1 and 2. During cycles 3 through 6, daratumumab was given on days 1 and 15; for cycle 7 and subsequent cycles, daratumumab was given on day 1 until disease progression. All patients received thromboprophylaxis that included low-dose aspirin, low-molecular-weight heparin, or other equivalent antithrombotic agents. To reduce the risk of infusion reactions, it was recommended that all patients receive their protocol-specified dose of oral dexamethasone, oral acetaminophen, oral or intravenous antihistamine, and an oral leukotriene receptor antagonist approximately 1 h prior to daratumumab infusion.
Pomalidomide and dexamethasone dose modifications were permitted during the study; if pomalidomide was withheld, dexamethasone was also withheld. Daratumumab dose reductions were not allowed. In the event of grade 4 neutropenia or febrile neutropenia, the daratumumab dose was withheld, and complete blood counts were evaluated weekly. The treating physician could begin granulocyte colony-stimulating factor if the patient was not already receiving it. Absolute neutrophil counts of ≥ 1000 cells/µL were required before restarting pomalidomide. In the event of thrombocytopenia, the dose was withheld, and complete blood counts were evaluated weekly. Dosing resumed for pomalidomide at 1 dose level lower once platelet count had recovered to ≥ 50,000/µL.
Endpoints and assessments
The primary endpoint was the ORR by modified International Myeloma Working Group (mIMWG) criteria [21]. Secondary endpoints were time to response, duration of response (DOR), time to progression, progression-free survival (PFS), and overall survival.
At screening, all patients provided baseline bone-marrow aspirate and blood samples for analysis. Tumor responses were based on the investigator’s assessment using local imaging review (if applicable) and central laboratory results according to mIMWG criteria. For patients with daratumumab interference on serum immunofixation (IFE), the Sebia Hydrashift 2/4 Daratumumab IFE Interference test (Norcross, GA, USA) was used to distinguish a positive serum protein electrophoresis/IFE due to the presence of daratumumab vs the presence of underlying (endogenous) monoclonal protein. Patients were considered complete responders if their positive IFE was confirmed to be daratumumab and if they met all other iMWG criteria for complete response (CR). Time to response, DOR, time to progression, and PFS were calculated based on the investigator’s response assessment, and all time-to-event endpoints were estimated from the time of study enrollment, except DOR, which was calculated from the time of initial response.
Safety assessments included adverse events (AEs), physical examinations, clinical laboratory evaluations performed at a central laboratory, venous thromboembolism monitoring, pregnancy testing, and counseling. AEs were coded according to the Medical Dictionary for Regulatory Activities (MeDRA version 23). The severity of AEs was graded according to the National Cancer Institute Common Terminology Criteria for Adverse Events (version 4.03). Once discontinued from the study treatment, patients would be followed up for ≤5 years after the last patient was enrolled (unless the follow-up was shorter due to withdrawal of consent, loss to follow-up, or death).
Statistical considerations
The safety population, defined as all enrolled patients who received ≥ 1 dose of study medication, was used for all safety analyses. The intention-to-treat population consisted of all enrolled patients, regardless of whether they received any study treatment, and was used for all efficacy analyses. The efficacy-evaluable population consisted of all enrolled patients who met eligibility criteria, received ≥ 1 dose of study medication, and had ≥ 1 postbaseline response assessment. The efficacy-evaluable population was used to provide supporting sensitivity analyses for the primary endpoint and key secondary endpoints.
Sample size determination
In this study, the primary objective was to test the hypothesis that the ORR for the triplet therapy in Japanese patients exceeded 25% using an exact 1-sided binomial test conducted at an α level of 0.025. A sample size of 17 patients was calculated to provide 80% power for an expected ORR of 60% [22]. Accounting for dropouts and non-eligibility, approximately 20 patients were expected to be enrolled in the study. The null ORR of 25% was based on Ichinohe et al.[22], and the expected 60% ORR under this triplet therapy was based on Chari et al.[23].
Analysis of the primary endpoint
The ORR was based on the best confirmed response prior to the data cutoffand was defined as the percentage of patients showing a confirmed partial response (PR) or better (CR, very good partial response [VGPR], or PR). ORR was estimated and the hypothesis of ORR exceeding 25% was evaluated using a binomial test. In addition, the 95% confidence intervals were calculated using the Clopper-Pearson exact method. The analysis of the ORR primary endpoint was used for both the intention-to-treat and efficacy-evaluable populations.
Results
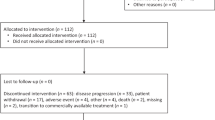
A total of 25 patients were screened for cohort C, and 18 patients were enrolled at 7 sites in Japan. Median age was 67.5 years, and most patients (77.8%) were male (Table 1). The median time since MM diagnosis was 3.9 years. Patients had either 1 (56%) or 2 (44%) prior lines of therapy. All patients were treated with lenalidomide in the immediate prior line of therapy, and 12 (67%) had lenalidomide-refractory disease. The most recent prior lenalidomide dose was ≤10 mg in 11 patients (61%). Overall, 16 patients (89%) had received a proteasome inhibitor, and 10 patients (56%) had undergone prior stem cell transplant.
At data cutoff (August 3, 2020), 15 patients (83%) were still on treatment; 3 patients (17%) had discontinued treatment—2 due to AEs and 1 due to a protocol violation. Treatment exposure is shown in Table 2. Median duration of treatment for the triplet therapy was 6.9 months, and the median number of treatment cycles was 7. The median relative dose intensity was 0.7 for pomalidomide and dexamethasone and 0.9 for daratumumab.
At a median follow-up of 8.1 months (range 2.3–14.7 months), the ORR was 83% (95% CI, 58.6–96.4%; P < 0.001) in the intention-to-treat population, including 4 patients with CR (22%) and 7 with VGPR (39%) (Table 3). The clinical benefit response rate was 83% (95% CI 58.6–96.4%). Median time to response was 1.1 months (range 1.0–9.0 months). At 52 weeks, all patients were event free for PFS, and the 15 patients with response were event free for DOR. In patients who relapsed while receiving previous lenalidomide treatment, the ORR was 100% (96% CI 54.1–100.0%). In patients whose disease was refractory to previous lenalidomide treatment, the ORR was 75% (95% CI 42.8–94.5%) (Table 3). Patients with high-risk cytogenetic abnormalities achieved PR or better (i.e., presence of 17p deletion [n = 2; 1 CR, 1 VGPR] and 4;14 translocation [n = 1 PR]). No patients in the study had 14;16 translocation.
All patients in the safety population experienced ≥ 1 treatment-emergent AE (TEAE). The most frequently reported TEAEs of any grade were neutropenia (77.8%), rash (33.3%), and leukopenia, pyrexia, and infusion-related reaction (27.8% each). All patients also had ≥ 1 grade 3/4 TEAE (Table 4), the most common of which were neutropenia (78%), leukopenia (28%), and lymphopenia (22%). The most common nonhematologic grade 3/4 TEAEs were pneumonia (11%) and hypophosphatemia (11%). Eight patients (44%) had ≥ 1 TEAE leading to pomalidomide dose reduction (Table 5), of which the most common was neutropenia (28%). The most common TEAEs leading to pomalidomide dose interruption included neutropenia (67%), leukopenia (17%), and rash (17%). The most common TEAE leading to dexamethasone dose interruption was neutropenia (61%). Neutropenia (78%) and infusion-related reaction (28%) were the most common TEAEs leading to daratumumab dose interruption. Two patients (11%) experienced TEAEs leading to discontinuation; 1 patient experienced pneumonia and rash, and the other patient experienced neutropenia.
Overall, 3 patients (17%) had a serious TEAE: 2 patients with pneumonia and 1 patient with tumor lysis syndrome. No patients died during the treatment period. One patient died due to progressive disease 276 days after their first dose of study treatment, but this death occurred outside of the study treatment period after the patient had initiated a subsequent antimyeloma therapy.
Discussion
The combination of pomalidomide, dexamethasone, and daratumumab demonstrated promising efficacy in this population of previously lenalidomide-treated Japanese patients with RRMM. The study met its primary endpoint with an ORR of 83% (P < 0.001), thus rejecting the null hypothesis (i.e., ORR ≤ 25%). These outcomes from the Japan-only cohort C of MM-014 were consistent with the results observed with pomalidomide, dexamethasone, and daratumumab in cohort B (US and Canada: ORR, 77.7%; median PFS, not reached; 1-year PFS rate, 75.1%; median follow-up, 17.2 months) [15] as well as a large European population (APOLLO: ORR, 69%; 18-month PFS rate, 42%; median follow-up, 16.9 months [24]). Furthermore, an ORR of 75% was achieved in patients whose disease was refractory to previous lenalidomide treatment. Notably, all 3 patients in this cohort with high-risk cytogenetic phenotypes achieved clinically meaningful responses (CR, VGPR, or PR), which suggests that this triplet combination could be an option for these difficult-to-treat Japanese patients; results were consistent with those in the larger MM-014 cohort B and APOLLO studies [15, 24].
Although published data from clinical trials are limited in patients with RRMM who previously received lenalidomide, in larger studies such as MM-014 cohort B [15], OPTIMISMM [13], ELOQUENT-3 [25], and APOLLO [24], triplet combinations with pomalidomide in these patients resulted in a higher ORR rate and improved PFS vs doublet combinations. Similar results were observed in a Japanese subset (n = 17) of OPTIMISMM [26], where ORR was 100% (VGPR or better, 58%; median PFS, 17.6 months) in 12 patients treated with pomalidomide, bortezomib, and dexamethasone compared with an ORR of 60% (VGPR or better, 20%; median PFS, 4.4 months) in 5 patients treated with bortezomib and dexamethasone. A subset analysis of the ELOQUENT-3 study also showed similar results in a Japanese subpopulation (n = 20), 80% of whom had disease refractory to both lenalidomide and a proteasome inhibitor [27]. In this subpopulation, an ORR of 69% and VGPR-or-better rate of 23% were achieved in patients receiving the triplet therapy (n = 13). The similarity of clinical outcomes among global and Japanese populations in MM-014, OPTIMISMM, and ELOQUENT-3 supports the overall findings of efficacy with these pomalidomide-based triplet combinations.
The safety profile of pomalidomide, dexamethasone, and daratumumab was consistent with the known toxicities of the individual agents and with the well-established safety profile seen in the larger MM-014 cohort B. The most common grade 3/4 hematologic TEAEs were neutropenia, anemia, and thrombocytopenia, and the most common grade 3/4 nonhematologic TEAE was pneumonia [15]. While no new safety concerns were identified, these interim results should be interpreted with caution due to the small number of patients and the shorter median follow-up (8.1 months) compared with MM-014 cohort B (17.2 months) and APOLLO (16.9 months) [15, 24]. Most TEAEs were managed with dose reductions or interruptions, but 2 patients discontinued due to neutropenia (n = 1) and rash (n = 1), indicating that patients treated with this regimen may require careful management of these AEs.
In summary, the pomalidomide, dexamethasone, and daratumumab triplet regimen demonstrated promising efficacy and a tolerable safety profile in Japanese patients with RRMM previously treated with lenalidomide. The results suggest that continuous immunomodulation with pomalidomide-based triplets is an effective approach in patients exposed to or whose disease progressed after 1 or 2 prior lines that included lenalidomide treatment; the results support the use of pomalidomide as a foundation for combination therapy in RRMM.
Data availability statement
The Bristol Myers Squibb policy on data sharing may be found at https://www.bms.com/researchers-and-partners/independent-research/data-sharing-request-process.html.
References
Moreau P, de Wit E. Recent progress in relapsed multiple myeloma therapy: implications for treatment decisions. Br J Haematol. 2017;179:198–218.
Sonneveld P, Broijl A. Treatment of relapsed and refractory multiple myeloma. Haematologica. 2016;101:396–406.
Rajkumar SV. Multiple myeloma: 2020 update on diagnosis, risk-stratification and management. Am J Hematol. 2020;95:548–67.
Moreau P, San Miguel J, Sonneveld P, Mateos MV, Zamagni E, Avet-Loiseau H, et al. Multiple myeloma: ESMO Clinical Practice Guidelines for diagnosis, treatment and follow-up. Ann Oncol. 2017;28:iv52–61.
Moreau P, Zamagni E, Mateos M-V. Treatment of patients with multiple myeloma progressing on frontline-therapy with lenalidomide. Blood Cancer J. 2019;9:38.
Harousseau JL, Attal M. How I treat first relapse of myeloma. Blood. 2017;130:963–73.
Yong K, Delforge M, Driessen C, Fink L, Flinois A, Gonzalez-McQuire S, et al. Multiple myeloma: patient outcomes in real-world practice. Br J Haematol. 2016;175:252–64.
Dimopoulos MA, Oriol A, Nahi H, San-Miguel J, Bahlis NJ, Usmani S, et al. Daratumumab, lenalidomide, and dexamethasone for multiple myeloma. N Engl J Med. 2016;375:1319–31.
Raab MS, Cavo M, Delforge M, Driessen C, Fink L, Flinois A, et al. Multiple myeloma: practice patterns across Europe. Br J Haematol. 2016;175:66–76.
Pomalyst (pomalidomide) [package insert]. Summit, NJ: Celgene Corporation; 2019.
Lopez-Girona A, Mendy D, Ito T, Miller K, Gandhi AK, Kang J, et al. Cereblon is a direct protein target for immunomodulatory and antiproliferative activities of lenalidomide and pomalidomide. Leukemia. 2012;26:2326–35.
Ocio EM, Fernández-Lázaro D, San-Segundo L, López-Corral L, Corchete LA, Gutiérrez NC, et al. In vivo murine model of acquired resistance in myeloma reveals differential mechanisms for lenalidomide and pomalidomide in combination with dexamethasone. Leukemia. 2014;29:705–14.
Richardson PG, Oriol A, Beksac M, Liberati AM, Galli M, Schjesvold F, et al. Pomalidomide, bortezomib, and dexamethasone for patients with relapsed or refractory multiple myeloma previously treated with lenalidomide (OPTIMISMM): a randomised, open-label, phase 3 trial. Lancet Oncol. 2019;20:781–94.
Siegel DS, Schiller GJ, Song KW, Agajanian R, Stockerl-Goldstein K, Kaya H, et al. Pomalidomide plus low-dose dexamethasone in relapsed refractory multiple myeloma after lenalidomide treatment failure. Br J Haematol. 2020;188:501–10.
Siegel DS, Schiller GJ, Samaras C, Sebag M, Berdeja J, Ganguly S, et al. Pomalidomide, dexamethasone, and daratumumab in relapsed refractory multiple myeloma after lenalidomide treatment. Leukemia. 2020;34:3286–97.
Pierceall WE, Amatangelo MD, Bahlis NJ, Siegel DS, Rahman A, Van Oekelen O, et al. Immunomodulation in pomalidomide, dexamethasone, and daratumumab-treated patients with relapsed/refractory multiple myeloma. Clin Cancer Res. 2020;26:5895–902.
Pomalyst (pomalidomide) [package insert] [in Japanese]. Tokyo, Japan: Celgene KK; 2019.
The Japanese Society of Hematology: Hematopoietic tumor clinical practice guidelines. III. Multiple myeloma: MM. http://www.jshem.or.jp/gui-hemali/3_1.html#soron Accessed June 23, 2021.
Iida S, Ishida T, Murakami H, Ozaki S, Abe M, Hata H, et al. JSH practical guidelines for hematological malignancies, 2018: III. Myeloma-1. Multiple myeloma (MM). Int J Hematol. 2019;109:509–38.
Darzalex (daratumumab) [package insert] [in Japanese]. Tokyo, Japan: Janssen Pharmaceutical K.K; 2019.
Kyle RA, Rajkumar SV. Criteria for diagnosis, staging, risk stratification and response assessment of multiple myeloma. Leukemia. 2009;23:3–9.
Ichinohe T, Kuroda Y, Okamoto S, Matsue K, Iida S, Ueda R, et al. A multicenter phase 2 study of pomalidomide plus dexamethasone in patients with relapsed and refractory multiple myeloma: the Japanese MM-011 trial. Exp Hematol Oncol. 2016;5:11.
Chari A, Suvannasankha A, Fay JW, Arnulf B, Kaufman JL, Ifthikharuddin JJ, et al. Daratumumab plus pomalidomide and dexamethasone in relapsed and/or refractory multiple myeloma. Blood. 2017;130:974–81.
Dimopoulos MA, Terpos E, Boccadoro M, Delimpasi S, Beksac M, Katodritou E, et al. Daratumumab plus pomalidomide and dexamethasone versus pomalidomide and dexamethasone alone in previously treated multiple myeloma (APOLLO): an open-label, randomised, phase 3 trial. Lancet Oncol. 2021;22:801–12.
Dimopoulos MA, Terpos E, Boccadoro M, Delimpasi S, Beksac M, Katodritou E, et al. Elotuzumab plus pomalidomide and dexamethasone for multiple myeloma. N Engl J Med. 2018;379:1811–22.
Sunami K, Matsue K, Suzuki K, Takezako N, Shinagawa A, Sakurai S, et al. Pomalidomide-bortezomib-dexamethasone in relapsed or refractory multiple myeloma: Japanese subset analysis of OPTIMISMM. Cancer Sci. 2020;111:2116–22.
Hori M, Takezako N, Sunami K, Ito S, Kuroda J, Popa-McKiver M, et al. Elotuzumab plus pomalidomide/dexamethasone for the treatment of relapsed/refractory multiple myeloma: Japanese subanalysis of the randomized phase 2 ELOQUENT-3 study. Blood. 2018;132:3260.
Acknowledgements
The authors thank the patients and families who made this study possible. We also thank the study investigators and the clinical teams who made this study possible. The study was funded and supported by Celgene, a Bristol-Myers Squibb Company. The authors acknowledge Alex Loeb, PhD, of Chrysalis Medical Communications for medical writing and editorial assistance in the preparation of this manuscript, which was funded by Bristol Myers Squibb.
Author information
Authors and Affiliations
Contributions
K. Matsue, K. Sunami, M. Matsumoto, J. Kuroda, S. Kuwayama, M. Nishio, K. Lee, and S. Iida contributed to the conceptualization and design of the study. Patient treatment and data collection were performed by K. Matsue, K. Sunami, M. Matsumoto, J. Kuroda, I. Sugiura, H. Iwasaki, and S. Iida. Data analysis was performed by W. Chung. All authors contributed to the interpretation of results and preparation of the manuscript. All authors have read and approved the final manuscript.
Corresponding author
Ethics declarations
Conflict of interests
K. Matsue reported receiving travel funding from Celgene, a Bristol-Myers Squibb Company, and Janssen. K. Sunami reported honoraria and research funding from AbbVie, Alexion Pharma, Amgen Astellas, Bristol Myers Squibb, Celgene, a Bristol-Myers Squibb Company, Daiichi Sankyo, GlaxoSmithKline, Janssen, MSD, Novartis, Ono, Sanofi, and Takeda. M. Matsumoto reported honoraria from Janssen and Sanofi KK. J. Kuroda reported honoraria and research funding from AbbVie, Bristol Myers Squibb, Celgene, a Bristol-Myers Squibb Company, Chugai, Dainippon Sumitomo, Eizai, Janssen, Kyowa, Nippon Shinyaku, Ono, Otsuka, Sanofi, Sysmex, and Takeda. I. Sugiura reported no competing interests. H. Iwasaki reported research funding from Kyowa Kirin. W. Chung is an employee of Bristol Myers Squibb and has equity ownership in Bristol Myers Squibb. S. Kuwayama is an employee of Bristol Myers Squibb and has equity ownership in Bristol Myers Squibb. M. Nishio is an employee of Bristol Myers Squibb and has equity ownership in Bristol Myers Squibb. K. Lee is an employee of Bristol Myers Squibb and has equity ownership in Bristol Myers Squibb. S. Iida received honoraria and research funding from Celgene, a Bristol-Myers Squibb Company, Janssen, Takeda, Ono, Sanofi, and Daiichi Sankyo and research funding from Chugai, Bristol Myers Squibb, AbbVie, Kyowa Kirin, and GlaxoSmithKline.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
About this article
Cite this article
Matsue, K., Sunami, K., Matsumoto, M. et al. Pomalidomide, dexamethasone, and daratumumab in Japanese patients with relapsed or refractory multiple myeloma after lenalidomide-based treatment. Int J Hematol 116, 122–130 (2022). https://doi.org/10.1007/s12185-022-03338-4
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12185-022-03338-4