Abstract
Langerhans cell histiocytosis (LCH) is a clonally expanding neoplasm characterized by the accumulation of CD1a + CD207 + myeloid dendritic cells. As LCH is a rare disease and is presumed to mainly affect children, the clinical features and treatment outcomes of adult LCH have been poorly documented. We retrospectively reviewed 53 adult patients with LCH who were referred to the Institute of Medical Science, the University of Tokyo from 2005 to 2018. The median age at diagnosis was 42 years with a slight female predominance (57%). The time between onset and diagnosis varied among patients (median, 8 months; range, 0–144 months). In total, 40% of the patients had single organ involvement and 60% had multiple organ involvement. Overall, the most frequently affected organ was bone (62%), followed by the central nervous system (34%), and the lung (28%). Twenty-six patients required systemic treatment, and 25 patients underwent the Special C regimen. Twenty patients (80%) who underwent Special C regimen showed a partial response or better with favorable toxicity. All but one patient is still alive. Median progression-free survival has not been reached despite a median follow-up of 35.5 months. Immunohistochemistry revealed that 39% of patients were positive for BRAF-V600E, which was a lower proportion than in previous reports from North America and Europe.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Langerhans cell histiocytosis (LCH) is a rare inflammatory myeloid neoplasm characterized by infiltration of CD1a + CD207 + histiocyte with immune cells. As indicated by its name, LCH was believed to arise from epidermal Langerhans cells due to similarities in expression markers and histopathological findings. However, recent studies suggest that LCH cells are more similar to dendritic cell precursors derived from bone marrow [1]. There has been significant progress in clinical and basic research on LCH during the last decade. The recurrent oncogenic BRAF-V600E mutation has been found in more than half of LCH patients, which represents a major breakthrough [2]. Consequently, LCH is now defined as a clonally expanding inflammatory myeloid neoplasm according to the revised 2016 classification of the World Health Organization [3, 4]. Despite advances in genetic understanding and treatment options, the clinical profile and treatment outcomes of adult LCH remain poorly documented. Here, we report the clinical features and BRAF status of 53 Japanese patients with adult LCH from a single institution.
Materials and methods
Patients
We retrospectively analyzed the data of 61 patients who were referred to the hospital of the Institute of Medical Science, University of Tokyo (IMSUT) between October 2005 and November 2018 with adult LCH. Eight patients were excluded due to being undiagnosed, in turn due to a lack of biopsy specimens or atypical histopathological findings. This study was approved by the Institutional Review Board of IMSUT (#28–5-0502) and was conducted according to the principles of the Declaration of Helsinki. All patients provided written informed consent.
Diagnosis and clinical evaluation
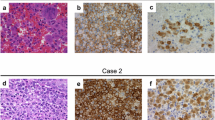
Fifty-three patients were diagnosed with LCH based on histopathological findings and immunohistochemical expression of CD1a and CD207. All patients were re-evaluated via a complete physical examination, laboratory tests, and a radiographic evaluation, including computed tomography and magnetic resonance imaging. A positron emission tomography scan and gallium-67 scintigraphy were also performed if necessary. The clinical classification was made according to the LCH Evaluation and Treatment Guidelines of the Histiocyte Society [5].
BRAF-V600E analysis
A BRAF-V600E immunohistochemical analysis was also performed in cases where formalin-fixed paraffin-embedded blocks or frozen specimens were available. The immunohistochemical analysis was performed using anti-BRAF V600E mouse monoclonal antibody (clone VE1; Spring Bioscience Corp., Pleasanton, CA, USA). In addition, cell-free DNA (cfDNA) was prepared from peripheral blood plasma and was subjected to BRAF-V600E genotyping by allele-specific quantitative polymerase chain reaction (AS-qPCR), which was specifically designed to detect BRAF-V600E, as described previously [6]. Furthermore, cfDNA was also evaluated by digital droplet PCR (ddPCR) using a BRAF V600 Screening Kit (Bio-Rad Laboratories, Hercules, CA, USA) to improve detection accuracy.
Treatments and outcomes
In consideration of the safety and efficacy at the outpatient clinic without hospitalization, we used nine cycles of the Japan LCH Study Group (JLSG) Special C regimen as first-line therapy for patients who required systemic treatment. The protocol consisted of 6 mg vinblastine on day 1, 60 mg oral prednisolone on days 1–5, and 20 mg/m2 methotrexate on day 15 with 1.5 mg/kg daily 6-mercaptopurine (6-MP) [7]. (Fig. 1).
Statistical analysis
All statistical analyses were performed with EZR (Saitama Medical Center, Jichi Medical University, Saitama, Japan), which is a graphical user interface for R (R Foundation for Statistical Computing, Vienna, Austria) [8]. Progression-free survival (PFS) and overall survival (OS) were calculated from the start of therapy until disease progression or death, or until the last follow-up. PFS and OS were estimated using the Kaplan–Meier method and compared via log-rank analysis. Cox models were used to assess the impact of covariates on outcomes. A p value < 0.05 was considered significant.
Results
The patient and disease characteristics are shown in Table 1. The median patient age at diagnosis was 42 years (range 1–79 years), and 57% were females (Fig. 2). Nearly all patients were adult-onset, except for two patients with relapsed infancy-onset LCH after a long period of remission. The duration of remission was 30 and 37 years, respectively. These two patients had single organ involvement at the time of first onset (skin and bone); however, both of them developed to multiple organ involvement after a long period of time. There was wide variation in the time between disease onset and diagnosis (from 0 to 144 months; median, 8 months; mean, 23.3 months), and patients’ first admissions after symptom onset were to various departments (Table 2). Six patients were diagnosed by chance during a regular medical checkup and showed no subjective symptoms. Patients with skin lesions tended to receive an earlier diagnosis. However, two patients were misdiagnosed and received incorrect management for several years. One patient with multifocal skin lesion was diagnosed with Behçet's disease and was treated with systemic and topic corticosteroids which made symptoms worse. Another patient with skin lesion was diagnosed as cutaneous pseudolymphoma and was also treated by systemic corticosteroids.
Twenty-one patients (40%) had single organ disease (single-system; SS) and 32 (60%) had multiple organ disease (multisystem; MS). One patient with MS-LCH showed comorbid Erdheim–Chester disease. Overall, more than half of the patients had bone lesions (62%), followed by central nervous system (CNS) involvement (34%). Of 19 patients with CNS involvement, 15 had isolated hypothalamic–pituitary lesion and two had hypothalamic–pituitary lesion with involvement in the lobe. One of the other two patients had lesion in convexity and another had dura-derived lesion. Of all, nine patients showed signs of diabetes insipidus as an initial symptom. Eventually, diabetes insipidus affected 12 patients, and 11 of them remain on 1-deamino-8-d-arginine vasopressin (DDAVP) replacement therapy to date. Of the 15 patients with pulmonary lesions, 2 were lung-only and the others were MS-LCH. Thirteen patients were smokers and 2 were never smokers. Of 19 patients with CNS involvement, 15 had isolated hypothalamic–pituitary lesion and 2 had hypothalamic–pituitary lesion with involvement in the lobe. One of the other two patients had lesion in convexity and another had dura-derived lesion. Among the MS-LCH patients, seven had a risk of organ involvement, such as liver, spleen, or bone marrow.
Immunohistochemical analysis of the biopsy specimens of 23 patients revealed that 9 (39%) were positive for BRAF-V600E. The AS-qPCR and/or ddPCR analyses of peripheral blood samples of 33 patients showed that only 6 MS-LCH patients were positive for BRAF-V600E. The list of patients who were able to perform immunohistochemical analysis and AS-qPCR and/or ddPCR is listed in Table 3. As shown in Table 3, nearly all the results matched in both immunohistochemical analyses and AS-qPCR. However, UPN 7 was positive for AS-qPCR, but was negative for immunohistochemical analyses. This may be explained by the limitation of the tumor specimen, namely, possibility that some but not all lesions are positive for BRAF-V600E in patients with multisystem LCH. Indication for systemic therapy was patients with multiple organ involvements, symptomatic CNS lesion, and multifocal bone lesions. In addition, one SS-LCH patient with progressive skin lesion affecting the whole body required systemic therapy. Of the 26 patients who required systemic treatment, 25 (first onset: 22, relapsed: three) received the JLSG Special C regimen. One patient, who had aggressive multiple organ involvement including a hypothalamic pituitary lesion, received 2-chlorodeoxyadenosine (2-CdA) initially. Of the 25 patients who were prescribed the Special C regimen, 19 completed the protocol and 2 patients are still in treatment. Four patients dropped out during the treatment due to a poor response with/without adverse events (AEs). The response rate to the Special C regimen, defined as a partial response or better, was 84% (21 patients), and a complete response (CR) was achieved in 64% (16 patients). (Table 4) The most common treatment-related AE was liver toxicity. An increase in aspartate aminotransferase was seen in 32% of patients, and an increase in alanine aminotransferase was seen in 24%. Grade 3 AEs were seen in eight (32%) patients, and the most common grade 3 AE was a decrease in the white blood cell count, seen in four patients. Dose reduction of 6-MP was required in five patients with grade 3 AEs, and, moreover, two among these had also skipped methotrexate once. All five patients completed the protocol. The Kaplan–Meier curves for OS and PFS of 25 patients for induction therapy are shown in Fig. 3a and b. The median OS and PFS have not been reached at the time of analysis. The median OS observation period was 37 months (range 2–97 months) and that of PFS was 36 months (range 2–80 months). One patient, who died during the clinical course, had multiple organ involvement including a hypothalamic–pituitary lesion and received 2-CdA as salvage therapy following an inadequate response to the Special C regimen.
Discussion
As LCH is quite rare and the majority of patients are children; adult patients with LCH are typically ignored by physicians, so the diagnosis is generally delayed. In our study, the median time from the first symptom to diagnosis was 8 months, and the mean time was 23.3 months. The clinical presentation of LCH varies and it can mimic other diseases; therefore, patients are often referred to various professionals. In our study, patients were referred to 12 different departments and only two patients were referred to a hematology–oncology specialist before admission to IMSUT. Although LCH is not always fatal, a delay in the diagnosis and treatment can lead to serious and irreversible organ impairment. In our study, one patient was misdiagnosed with malignant lymphoma for nearly 6 years and was subjected to a systemic chemotherapy regimen consisting of cyclophosphamide, doxorubicin, vincristine, and prednisone, which exacerbated his condition. Physicians should be aware that LCH is a myeloid neoplasm and requires prompt diagnosis and appropriate treatment. The clinical presentation of LCH is extremely heterogeneous, ranging from self-healing indolent disease to disseminated aggressive disease that can lead to death. Localized pulmonary lesions, which are common in adults, are strongly associated with smoking and diminish on smoking cessation. In our study, among 15 patients with pulmonary lesions, 13 (86.7%) were smokers. Considering that the smoking rate in Japan is 17.9% according to a survey conducted by Japan Tobacco Inc. in 2018, the smoking rate in these patients is extremely high [9]. Two patients were never-smokers, and both had multiple organ involvement. Of the 15 patients with a lung lesion, 13 had MS-LCH, and two had lung-only disease; both were current smokers.
Systemic chemotherapy is strongly recommended for MS-LCH or SS-LCH with multifocal bone lesions [10]. There are no evidence-based standard treatments for adult LCH, but a combination of vinblastine and prednisolone, as derived from the pediatric LCH protocol, is commonly used as an induction therapy. However, some reports have shown that adult patients who undergo vinblastine and prednisolone treatment tend to show higher incidents of grade 3–4 neuropathy, resulting in a poor overall response [7, 11, 12]. The JLSG Special C regimen that we adopted was also derived from the pediatric protocol, where the purpose was to establish a chemotherapy regimen that can be completed in the outpatient clinic without hospitalization. The outcome was equivalent to that of other reported regimens, with favorable toxicity [13, 14]. Tazi et al. (2017) indicated that the most common grade 3–4 AE among adult patients with LCH treated with the vinblastine-based regimen was neutropenia [11]. Our study showed similar outcomes; however, liver toxicity was the most common AE. The liver function of all of our patients had recovered to the normal range after reducing the 6-MP dose, suggesting a possible racial difference. Patients with skin lesions treated with the Special C regimen showed the highest response rate (88%). However, they also had a higher frequency of relapse (38%) compared to patients with other lesions. In contrast, patients with a CNS lesion had a lower rate of relapse (11%), with a fairly high response rate (81%).
While LCH has a definite age at onset peak of < 10 years of age [15], the prevalence and incidence rates in adult patients remain unclear. In our study, there seemed to be an age onset peak between the 20s and early 40s (Fig. 2). A previous report based on the International Registry of the Histiocyte Society showed similar age peaks [16]. Common malignancies in adolescents and young adults include breast cancer, brain tumors, melanoma, thyroid cancer, and leukemia. However, the peak incidence age of these malignancies is older, and none of them have an age peak similar to adult LCH. Male predominance has been described in childhood LCH, with a ratio of about 2:1 [17]. However, our study showed no gender difference in adult patients, as per previous reports [16, 18].
In our study, the BRAF mutation was identified in 39% of patient biopsy specimens, and in 20% of peripheral blood plasma samples. As nearly half of the peripheral blood samples were obtained from patients with low disease activity, the plasma BRAF mutation results were reasonable. However, immunohistochemistry analysis of the biopsy specimens showed a lower positive ratio compared to previous reports. Interestingly, reports from Asian countries seem to show a lower frequency of the BRAF mutation in LCH patients, indicating possible racial differences in mutation frequencies (Table 5). Moreover, the BRAF mutation seems to be less frequent in Asian populations with colon cancer or malignant melanoma [26, 27].
Several groups have reported successfully treating BRAF-V600E-positive LCH with BRAF inhibitors [28, 29]. Advances in next-generation sequencing technology have revealed several other driver mutations in the MAPK and PI3K pathways, which could inform more targeted therapies. Prospective trials including targeted therapies with/without existing approaches are warranted to improve outcomes in adults and children with LCH.
References
Allen CE, Merad M, McClain KL. Langerhans-cell histiocytosis. N Engl J Med. 2018;379(9):856–68.
Vergilio JA, Badalian VG, Degar BA, MacConaill LE, Brandner B, Calicchio ML, et al. Recurrent BRAF mutations in Langerhans cell histiocytosis. Blood. 2010;116:1919–23.
Emile JF, Abla O, Fraitag S, Horne A, Haroche J, Donadieu J, et al. Revised classification of histiocytoses and neoplasms of the macrophage-dendritic cell lineages. Blood. 2016;127(22):2672–81.
Swerdlow SH, Campo E, Harris NL, Jaffe ES, Pileri SA, Stein H, et al. WHO classification of tumours of haematopoietic and lymphoid tissues. In: Weiss LM, Jaffe R, Facchetti F, editors. WHO classification of tumours of haematopoietic and lymphoid tissues. Lyon, France: IARC; 2017. p. 470–472.
Langerhans cell histiocytosis; histiocyte society evaluation and treatment guidelines; April. 2009. Available from: https://www.histiocytesociety.org/document.doc?id=290. Accessed 10 Aug 2019.
Kobayashi M, Tojo A. The BRAF-V600E mutation in circulating cell-free DNA is a promising biomarker of high-risk adult Langerhans cell histiocytosis. Blood. 2014;124(16):2610–1.
Morimoto A, Shimazaki C, Takahashi S, Yoshikawa K, Nishimura R, Wakita H, et al. Therapeutic outcome of multifocal Langerhans cell histiocytosis in adults treated with the Special C regimen formulated by the Japan LCH Study Group. Int J Hematol. 2013;97(1):103–8.
Kanda Y. Investigation of the freely-available easy-to-use software “EZR” (Easy R) for medical statistics. Bone Marrow Transplant. 2013;48:452–8.
JT’s Annual Survey Finds 17.9 % of Japanese Adults Are Smokers. Japan Tobacco Inc. https://www.jt.com/media/news/2018/pdf/20180730_02.pdf. Accessed 10 Aug 2019.
Girschikofsky M, Arico M, Castillo D, Chu A, Doberauer C, Fichter J1, et al. Management of adult patients with Langerhans cell histiocytosis: recommendations from an expert panel on behalf of Euro-Histio-Net. Orphanet J Rare Dis. 2013;8:72.
Tazi A, Lorillon G, Haroche J, Neel A, Dominique S, Aouba A, et al. Vinblastine chemotherapy in adult patients with Langerhans cell histiocytosis: a multicenter retrospective study. Orphanet J Rare Dis. 2017;12:95.
Cantu MA, Lupo PJ, Bilgi M, Hicks MJ, Allen CE, McClain KL. Optimal therapy for adults with Langerhans cell histiocytosis bone lesions. PLoS ONE. 2012;7:e43257.
Derenzini E, Fina MP, Stefoni V, Pellegrini C, Venturini F, Broccoli A, et al. MACOP-B regimen in the treatment of adult Langerhans cell histiocytosis: experience on seven patients. Ann Oncol. 2010;21(6):1173–8.
Duan MH, Han X, Li J, Zhang W, Zhu TN, et al. Comparison of vindesine and prednisone and cyclophosphamide, etoposide, vindesine, and prednisone as first-line treatment for adult langerhans cell histiocytosis: a single-center retrospective study. Leuk Res. 2016;42:43–6.
Salotti JA, Nanduri V, Pearce MS, Parker L, Lynn R, Windebank KP. Incidence and clinical features of langerhans cell histiocytosis in the UK and Ireland. Arch Dis Child. 2009;94(5):376–80.
Aricò M, Girschikofsky M, Généreau T, Klersy C, McClain K, Grois N, et al. Langerhans cell histiocytosis in adults Report from the International. Registry of the Histiocyte Society. Eur J Cancer. 2003;39(16):2341–8.
Yağci B, Varan A, Cağlar M, Söylemezoğlu F, Sungur A, Orhan D, et al. Langerhans cell histiocytosis: retrospective analysis of 217 cases in a single center. Pediatr Hematol Oncol. 2008;25(5):399–408.
Götz G, Fichter J. Langerhans'-cell histiocytosis in 58 adults. Eur J Med Res. 2004;9(11):510–4.
Sasaki Y, Guo Y, Arakawa F, Miyoshi H, Yoshida N, Koga Y, Nakashima K, Kurita D, Niino D1, Seto M, Ohshima K. Analysis of the BRAFV600E mutation in 19 cases of Langerhans cell histiocytosis in Japan. Hematol Oncol. 2017;35(3):329–34.
Go H, Jeon YK, Huh J, Choi SJ, Choi YD, Cha HJ, et al. Frequent detection of BRAF(V600E) mutations in histiocytic and dendritic cell neoplasms. Histopathology. 2014;65:261–72.
Tong C, Jia X, Jia Y, He Y. Langerhans cell histiocytosis in Chinese adults: absence of BRAF mutations and increased FOXP3+ regulatory T cells. Int J Clin Exp Pathol. 2014;7:3166–73.
Berres ML, Lim KP, Peters T, Price J, Takizawa H, Salmon H, et al. BRAF-V600E expression in precursor versus differentiated dendritic cells defines clinically distinct LCH risk groups. J Exp Med. 2015;212(2):281.
Héritier S, Emile JF, Barkaoui MA, Thomas C, Fraitag S, Boudjemaa S, et al. BRAF mutation correlates with high-risk langerhans cell histiocytosis and increased resistance to first-line therapy. J Clin Oncol. 2016;34(25):3023–30.
Sahm F, Capper D, Preusser M, Meyer J, Stenzinger A, Lasitschka F, et al. BRAFV600E mutant protein is expressed in cells of variable maturation in langerhans cell histiocytosis. Blood. 2012;120(12):e28–34.
Méhes G, Irsai G, Bedekovics J, Beke L, Fazakas F, Rózsa T, et al. Activating BRAF V600E mutation in aggressive pediatric Langerhans cell histiocytosis: demonstration by allele-specific PCR/direct sequencing and immunohistochemistry. Am J Surg Pathol. 2014;38(12):1644–8.
Yoon HH, Shi Q, Alberts SR, Goldberg RM, Thibodeau SN, Sargent DJ, Sinicrope FA. Alliance for clinical trials in oncology. Racial differences in BRAF/KRAS mutation rates and survival in stage III colon cancer patients. J Natl Cancer Inst. 2015;107(10):djv186.
Kim SY, Kim SN, Hahn HJ, Lee YW, Choe YB, Ahn KJ. Metaanalysis of BRAF mutations and clinicopathologic characteristics in primary melanoma. J Am Acad Dermatol. 2015;72(6):1036–46.
Haroche J, Cohen AF, Emile JF, Arnaud L, Maksud P, Charlotte F, et al. Dramatic efficacy of vemurafenib in both multisystemic and refractory Erdheim-Chester disease and Langerhans cell histiocytosis harboring the BRAF V600E mutation. Blood. 2013;121(9):1495–500.
Diamond EL, Subbiah V, Lockhart AC, Blay JY, Puzanov I, Chau I, et al. Vemurafenib for BRAF V600-Mutant Erdheim-chester disease and Langerhans cell histiocytosis: analysis of data from the histology-independent, phase 2. Open-label VE-BASKET Study JAMA Oncol. 2018;4(3):384–8.
Acknowledgments
We thank Mizuho Yamashita for outstanding assistance with the experiments. We also thank Dr. Shinsaku Imashuku, Dr. Akira Morimoto, and all the members of Japan LCH study group. Finally, we would like to offer special thanks to our LCH patients and their families.
Author information
Authors and Affiliations
Contributions
M.K. and A.T. designed the study; M.K. performed the experiments, analyzed data and wrote the paper; A.T supervised the study. All authors participated in patient care and have read and approved the manuscript.
Corresponding author
Ethics declarations
Conflict of interest
None of the authors declares that support, financial or otherwise, has been received from any organization that may have an interest in the submitted work.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
About this article
Cite this article
Kobayashi, M., Ando, S., Kawamata, T. et al. Clinical features and outcomes of adult Langerhans cell histiocytosis: a single-center experience. Int J Hematol 112, 185–192 (2020). https://doi.org/10.1007/s12185-020-02892-z
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12185-020-02892-z