Abstract
The objective of this prospective clinical trial (JALSG-STIM213, UMIN000011971) was to evaluate treatment-free remission (TFR) rates after discontinuation of imatinib in chronic myeloid leukemia (CML). CML patients who received imatinib treatment for at least 3 years and sustained deep molecular response for at least 2 years were eligible. Molecular recurrence was defined as loss of major molecular response (MMR). Of the 68 eligible patients, 38.2% were women, the median age was 55.0 years, and the median duration of imatinib treatment was 97.5 months. The 12-month TFR rate was 67.6%. Patients who lost MMR were immediately treated with imatinib again; all re-achieved MMR. Three-year treatment-free survival (TFS) was estimated as 64.6% using the Kaplan–Meier method. Undetectable molecular residual disease (UMRD) was defined as no BCR-ABL1 in > 100,000 ABL1 control genes using international scale polymerase chain reaction. UMRD at the study baseline was found to be predictive of continuation of TFR. Our findings suggest that CML patients who meet all the eligibility criteria that have commonly been used in the TFR trials are able to discontinue imatinib use safely. TFR may thus be valuable as a new goal for CML treatment in Japan.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Chronic myeloid leukemia (CML) is caused in hematopoietic stem cells by the BCR-ABL1 fusion gene on the Philadelphia chromosome. CML is a rare hematological malignancy, occurring at an incidence of approximately 1–2 per 100,000 person-years [1,2,3]. Without any treatment, CML in the chronic phase (CP) progresses to the accelerated phase (AP) or blast phase (BP), which are usually associated with a lethal outcome in 5 years [4, 5]. The tyrosine kinase inhibitor (TKI) imatinib, which inhibits function of BCR-ABL1 tyrosine kinase, has dramatically improved the prognosis of CML [6,7,8] and has become a standard therapy for CML [9, 10].
However, according to the Japanese Society of Hematology (JSH) guidelines [11] and the European LeukemiaNet (ELN) guidelines [12], patients with CML should not stop imatinib therapy because imatinib is unable to eradicate CML stem cells in vitro and in vivo [13,14,15]. Although allogenous hematopoietic stem cell transplantation (allo-HSCT) is the only curative treatment to eradicate CML stem cells [16], the outcome of allo-HSCT depends on treatment-related mortality, the risk of which is associated with disease status, age, complications, and donor types [17]. Furthermore, the JSH guidelines do not recommend allo-HSCT for patients with CML-CP who respond to TKI [11]. So, CML patients are generally expected to continue TKI treatment throughout their lives.
Nevertheless, a prospective treatment-free remission (TFR) study, the Stop Imatinib (STIM) trial, suggested that approximately 39% of CML patients who maintained deep molecular response (DMR) for more than 2 years could safely stop imatinib [18, 19]. Although 61 of the 100 enrolled CML patients lost DMR, no patient progressed to AP/BC and 56 patients re-achieved DMR after re-treatment with imatinib [18, 19]. Since this pivotal study, TFR has been extensively studied and several TFR trials have been published to date [20,21,22,23,24]. Although these prospective TFR studies confirmed that 40–60% of CML patients could safely stop imatinib, the definition of molecular relapse varied across studies [25]. Additionally, few of the studies included Japanese cohorts that could be used as a basis for revising the JSH guidelines for CML treatment [22, 26]. Moreover, many Japanese patients with CML have been receiving imatinib treatment for long periods and have had continued DMR. According to a survey by members of the JSH, these patients often hope to stop taking imatinib for various reasons, including mild adverse events, health care costs, and the desire to become pregnant [27].
We conducted a phase 2 clinical trial (JALSG-STIM213, UMIN000011971) to evaluate the rate of successful TFR, assess the safety of discontinuing imatinib, and define predictive factors for successful TFR after imatinib has been stopped.
Materials and methods
Study design and patients
JALSG-STIM213 is a phase 2, multicenter, single-arm study performed by the Japan Adult Leukemia Study Group (JALSG) in Japan. This study was conducted in accordance with the Declaration of Helsinki. Written informed consent was obtained from all individual participants before enrollment. The study was approved by the Ethics Committee of Akita University (no. 1051) and by the ethics committees of all institutions that participated in this study.
Figure 1a presents the study design of JALSG-STIM213. Patients with CML-CP who received imatinib treatment for at least 3 years and who sustained DMR (at least 4-log reduction of BCR-ABL1 mRNA) for at least 2 years [confirmed by 4 consecutive polymerase chain reaction (PCR) tests] were eligible. MR4.5 [BCR-ABL1 international scale (IS) < 0.0032%, 4.5-log reduction of BCR-ABL1 mRNA] was confirmed before stopping imatinib. Patients who were treated with the other TKIs or received stem cell transplantation were excluded.
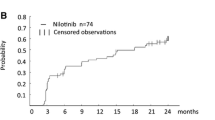
a STIM213 study design. TFR* was defined as no findings of loss of MMR (IS > 0.1%) after discontinuation of treatment. Molecular responses were assessed regularly by IS-PCR every month for the first 6 months, every 2 months for the next 6 months, and every 3 months thereafter in the TFR phase. Re-treatment was started immediately at the loss of MMR without a re-examination of IS-PCR. b The kinetics of BCR-ABL transcript in the TFR phase. Twenty-five patients lost MMR (IS > 0.1%) and 5 patients showed fluctuation in the value of BCR-ABL1 transcript that was below MMR level. c Kaplan–Meier estimates of treatment-free survival (TFS) after discontinuation of imatinib among all patients. TFS was defined as the time from the start of discontinuation of imatinib until loss of MMR. For patients without any molecular recurrence, survival times were censored at the date of the last assessment. d Cumulative incidence of MMR regained after re-treatment by imatinib (Re-MMR). The median duration to re-MMR was 40 days. e Estimated treatment-free survival after discontinuation of imatinib according to the molecular responses at the enrollment in this study. UMRD was defined as undetectable BCR-ABL1 transcripts in > 100,000 control ABL1 gene by IS-PCR. f Correlation between the TFR rate and median duration of TKI across JALSG-STIM213 and the previously published TFR trials: STIM [18, 19], TWISTER [20], DADI [22], A-STIM [21], KEIO-STIM [26], STOP-2G [24], KID study [23], EURO-SKI [31], and ENEStop [39]
In the TFR phase after stopping imatinib, BCR-ABL1 IS % was regularly monitored by IS-PCR testing every month for the first 6 months, every 2 months for the next 6 months, and every 3 months thereafter. Molecular recurrence was defined as loss of major molecular response (MMR). When a molecular recurrence was detected, patients started imatinib treatment immediately, without confirmation of loss of MMR by IS-PCR. In the re-treatment phase, BCR-ABL1 IS % was monitored by IS-PCR every month. The study protocol was terminated at the time that MMR was achieved again, when BCR-ABL1 IS % increased 3 times consecutively in 6 months, or at 6 months even if the patient had never re-achieved MMR.
Real-time quantitative reverse transcription polymerase chain reaction
During the TFR and re-treatment phases, IS-PCR analyses were performed using Ipsogen BCR-ABL1M-BCR IS-PCR kits in a central laboratory (Sysmex, Kobe, Japan). The Ipsogen IS-PCR kit possesses sufficient sensitivity to score MR4.5 according to the strictest conditions for avoiding false-negative results, as previously reported [28]. MMR was defined as 3-log reduction (BCR-ABL1 IS < 0.1%), MR4.5 was defined as 4.5-log reduction in BCR-ABL1 transcript (BCR-ABL1 IS < 0.0032%), and undetectable molecular residual disease (UMRD) was defined as no BCR-ABL1 transcripts. At least 100,000 control genes (ABL1) were required in IS-PCR analyses based on the kit-specific limit of detection (LoD) of 3 BCR-ABL1 copies/assay for the sample to be classified adequately [28].
Study endpoints and assessments
The primary endpoint was the TFR rate at 12 months after stopping imatinib. Secondary endpoints were the 3-year treatment-free survival (3y-TFS), MMR rate and time to MMR achieved by imatinib re-treatment. To establish predictive factors that were associated with TFR, we evaluated patients’ characteristics, including sex, Sokal score, European Treatment and Outcome Study (EUTOS) score, prior interferon-α treatment, duration of imatinib treatment, time to MMR, time to DMR, and UMRD before TFR phase. Safety was evaluated during the TFR phase, especially symptoms related to withdrawal syndrome. Adverse events were classified using the Common Terminology Criteria for Adverse Events, version 4.03.
Statistical analysis
The planned sample size was calculated using the 1-arm binomial program from Southwest Oncology Group (SWOG) statistical tools (https://stattools.crab.org/Calculators/oneArmBinomialColored.html), estimating the minimum number of patients who would be required to reject the null hypothesis for the primary endpoint (≤ 40% TFR rate at 12 months). Assuming that 15% of enrolled patients would not qualify for the TFR phase, a minimum enrollment of 62 patients was required to achieve 90% power to reject the null hypothesis with a 1-sided α-level of 5% if the true TFR rate at 12 months was ≥ 60%. With an actual enrollment of 68 patients, the power increased to 95% with all the other assumptions being the same.
The primary endpoint was presented as a percentage with 95% confidence interval (CI). Binomial test (one sided) of the primary endpoint was performed for a predefined threshold success rate of 40%. TFS was estimated using the Kaplan–Meier method and compared between groups using the log-rank test. TFS was measured from the date of stopping imatinib to the date of first molecular recurrence in the 68 eligible patients. For patients without a molecular recurrence, the survival time was censored at the date of the last assessment. Rates of regained MMR in the re-treatment phase were reported as cumulative incidences. Deaths before regaining MMR were treated as competing-risk events. To identify covariates that predicted longer TFS, univariate and multivariate Cox regression analyses were performed. The following variables were considered: patients’ age, sex, Sokal risk, EUTOS risk, prior interferon-α (IFN-α), duration of imatinib treatment, time to MMR, time to DMR, and UMRD before TFR. A stepwise multivariate approach was used to identify the most important prognostic factors with a variable retention criterion of two-sided P < 0.05. Variables which showed associations of marginal significance (two-sided P < 0.2) were used for multivariate model building. Statistical analyses were performed with EZR, which is a graphical user interface for R (version 2.13.0; The R Foundation for Statistical Computing, Vienna, Austria) [29] and Stata (version 13.0; Stata Corporation, College Station, TX, USA).
The data presented herein are based on a cutoff date of 30 June 2017, at which time all patients who entered the TFR phase had completed ≥ 36 months of TFR, entered the re-treatment phase, or discontinued the study.
Results
Patients
From 30 November 2013 to 31 March 2014, a total of 77 patients with CML-CP from 26 institutions were screened for eligibility to enroll in this study. Nine were excluded (consent withdrawal n = 1, not MR4.5 n = 8), and 68 entered the TFR phase. Of the 68 patients, 26 (38.2%) were women (Table 1). The median age was 55.0 years. Nine (13.2%) and 11 patients (16.2%) were classified as belonging to the high-risk group according to their EUTOS and Sokal risk scores, respectively. Thirteen patients (19.1%) were treated with interferon-α (IFN-α) prior to imatinib therapy. Most patients (73.5%) were treated by a standard dose of imatinib of 400 mg per day. The median duration of imatinib treatment was 97.5 months (range 78–130 months). The duration of imatinib treatment was less than 5 years in 12%, 5–8 years in 34%, and > 8 years in 54% of patients. The median time to MMR was 11.5 months (25th–75th percentiles, 7.5–22.7 months) and the median time to DMR was 30.6 months (25th–75th percentiles, 17.6–59.9 months). UMRD (BCR-ABL1 transcripts not detected) was confirmed by IS-PCR in 54 patients (79.4%) at the enrollment of this study.
TFR rate at 12 months and 3y-TFS
At 12 months, 46 of the 68 patients who were eligible to enter the TFR phase remained in TFR without re-treatment (67.6%, 95% CI 56.5–78.8%), exceeding the predefined threshold success rate of 40% (binomial test, one sided P < 0.0001). Twenty-two patients had a loss of MMR during the first 12 months and entered into the re-treatment phase of the study. Additionally, 5 patients had loss of MR4 (but not loss of MMR) and showed fluctuations of BCR-ABL1 transcripts. Of the 5 patients, 3 finally had loss of MMR at 14.9, 34.1, and 36.0 months as late molecular recurrences (Fig. 1b). The 3y-TFS was estimated to be 64.6% (95% CI 52.0–74.7%) using the Kaplan–Meier method (Fig. 1c). All patients with molecular recurrence regained MMR within 6 months after receiving imatinib in the re-treatment phase of the study (Fig. 1d).
Analysis based on background characteristics
In univariate analyses, UMRD before TFR was the only factor that was significantly predictive of continuation of MMR in the TFR phase (hazard ratio for loss of MMR in the TFR phase: 0.36, 95% CI 0.01–0.09, P = 0.014) (Table 2). Other factors did not show significant or marginally significant associations. Therefore, multivariate analysis was not performed. As estimated using the Kaplan–Meier method, the TFS curve was significantly better in patients with UMRD than in patients with MR4.5 (3y-TFS 72.2 vs. 35.7%, P = 0.0097) (Fig. 1e). Comparison of clinical characteristics between patients with UMRD and those with MR4.5 revealed no significant differences (Supplemental Table 1).
Safety and TKI withdrawal syndrome
No patients progressed to AP/BC in this study. There were no severe adverse events in the TFR phase. In contrast, 10 patients (15%) showed “TKI withdrawal syndrome”, which is transitory musculoskeletal pain within several weeks after imatinib discontinuation. Two patients had continued withdrawal syndrome of grade 1, but the remaining patients recovered completely with or without treatments, such as non-steroidal anti-inflammatory drugs (NSAIDs) (Table 3). Among 10 patients with TKI withdrawal syndrome, 7 patients (70%) had continued TFR throughout the 36-month follow-up.
Discussion
Recently, National Comprehensive Cancer Network (NCCN) guidelines have recommended discontinuation of TKI therapy outside of clinical trials for CML patients who meet several criteria, including having received TKI therapy for at least 3 years, DMR (BCR-ABL1 < 0.01%) for at least 2 years, no history of resistance to any TKI, and monthly molecular monitoring by IS-PCR [30]. All these criteria follow the common eligibility criteria reported in previous prospective TFR studies [18, 20, 21, 24], and they are also the same as the eligibility criteria used in the present TFR trial. In JALSG-STIM213, 67.6% of patients remained in TFR at 12 months and the 3y-TFS was estimated to be 64.6%, including 3 late recurrences after 12 months, which was consistent with results from other TFR studies. The most important observation is that no one progressed to AP/BC in JALSG-STIM213 or any of the other clinical trials under scheduled monitoring with IS-PCR. Our findings suggest that CML patients who meet the above eligibility criteria (those listed in the NCCN guidelines and used in the present trial) could safely stop imatinib outside the setting of clinical trials. This suggestion is also supported by the NCCN guidelines [30], as well as the new ELN guidelines that will be revised in the end of 2017 as a result of the EURO-SKI study [31].
There were 3 late molecular recurrences after 12 months in this trial. This finding is different from the STIM trial, in which there have not been any patients with molecular recurrence after 7 months [18, 19]. It seems that the presence or absence of late molecular recurrences depends substantially on the definition of molecular recurrence that is used. A stricter definition of recurrence was used in the STIM trial and, if we had used this stricter definition, the 3 patients who showed fluctuation of BCR-ABL1 transcripts would have been re-treated by imatinib within the first 12 months. Therefore, if a different definition of recurrence had been used, there might not have been any late molecular recurrences in this trial, as was observed in the STIM trial. Although the mechanisms of the late molecular recurrences were not clarified, they might be related to the immunological effects of NK/T cells against minimal residual disease [32].
The TFR rate in JALSG-STIM213 was slightly higher than the rates that have previously been reported for TFR trials. Using data from the previously published TFR trials, we performed a basic meta-regression analysis of the association between the median duration of TKI and the TFR rate. Simple linear regression was used, and revealed that relationship was approximated by (TFR rate, %) = 0.4386 (median TKI duration, months) + 20.447 (R 2 = 0.485) (Fig. 1f). This finding suggested that JALSG-STIM213 might have included a larger proportion of patients who were treated with imatinib for longer durations and achieved much deeper molecular responses, which may have resulted in the slightly higher TFR rate that we observed. Duration of TKI treatment was one of the predictive factors for successful TFR in previous TFR studies [18, 21, 31, 33]. According to the mathematical models [34,35,36], BCR-ABL1 clones are gradually decreased by TKI therapy and, depending on the treatment duration, these declines are expected to extend even below the minimum detectable level by IS-PCR. The linear correlation between the TFR rate and the duration of TKI therapy might indicate that TKIs can gradually erode residual BCR-ABL1 clones in bone marrow, in association with the duration of treatment, even though they cannot eradicate CML stem cells easily.
In the present trial, we also found an association between relapse risk and the level of deep molecular response that was obtained with imatinib. The only identified predictive factor for successful TFR was undetectable BCR-ABL1 transcript in > 100,000 ABL1 control genes before discontinuation of imatinib. This suggests that deeper responses are better for TFR in CML treatment. In the EURO-SKI trial, there were no differences in TFR between MR4 and MR4.5 values measured before TFR [31]. However, the sensitivity of the IS-PCR that was used in EURO-SKI might have been lower than the IS-PCR kit used in our study. In Japan, we can usually (and routinely) detect BCR-ABL1 transcripts in cDNA with > 100,000 ABL1 control genes in 1 PCR assay [28]. Cross et al. proposed defining molecular response as MR4, which refers to either detectable disease with 0.01% BCR-ABL1 IS or undetectable disease in cDNA with 10,000 ABL1 transcripts [37]. On the other hand, MR4.5 refers to either detectable disease with 0.0032% BCR-ABL1 IS or undetectable disease in cDNA with 32,000 ABL1 transcripts [37]. So, in the EURO-SKI trial, some patients who were classified as MR4 (according to Cross et al.’s definition) might have actually achieved MR4.5 or much deeper responses because of the low sensitivity of PCR. Moreover, ELN proposed that the limit of detection (LoD) of BCR-ABL1 transcripts should be 1 copy per IS-PCR assay [12]. Although the sensitivity for scoring MR4.5 depended on the kit-specific LoD of 3 BCR-ABL1 copies per assay and in cDNA with > 100,000 ABL1 in our study, it roughly equaled the sensitivity for scoring MR5 based on the LoD of 1 copy per assay in the ELN proposal. As defined in this study, UMRD was probably one of the deepest molecular levels analyzed in the TFR trials that included monitoring with IS-PCR. In the ISAV study [38] and the KID study [23], UMRD by IS-PCR and digital PCR was also one of the predictive factors for TFR. Although the sensitivity of IS-PCR is lower than that of digital PCR, our findings also suggest that deeper responses are better for TFR in CML treatment. Deininger proposed a sustenance limit of BCR-ABL1 clones based on the findings of the STIM study. We do not know the molecular level of the sustenance limit exactly, because it is far below the detection limit of quantitative PCR [36]. To address this uncertainty, TFR trials will need to use digital PCR or other new technologies that offer better quantitative accuracy than IS-PCR for MR4.5.
In conclusion, the results of JALSG-STIM213 suggest that TFR would be valuable as a new goal for CML treatment in Japan.
References
Garcia-Manero G, Faderl S, O’Brien S, Cortes J, Talpaz M, Kantarjian HM. Chronic myelogenous leukemia: a review and update of therapeutic strategies. Cancer. 2003;98(3):437–57.
Jemal A, Tiwari RC, Murray T, Ghafoor A, Samuels A, Ward E, et al. Cancer statistics, 2004. CA Cancer J Clin. 2004;54(1):8–29.
Redaelli A, Bell C, Casagrande J, Stephens J, Botteman M, Laskin B, et al. Clinical and epidemiologic burden of chronic myelogenous leukemia. Expert Rev Anticancer Ther. 2004;4(1):85–96.
Cortes JE, Talpaz M, Kantarjian H. Chronic myelogenous leukemia: a review. Am J Med. 1996;100(5):555–70.
Faderl S, Talpaz M, Estrov Z, Kantarjian HM. Chronic myelogenous leukemia: biology and therapy. Ann Intern Med. 1999;131(3):207–19.
O’Brien SG, Guilhot F, Larson RA, Gathmann I, Baccarani M, Cervantes F, et al. Imatinib compared with interferon and low-dose cytarabine for newly diagnosed chronic-phase chronic myeloid leukemia. N Engl J Med. 2003;348(11):994–1004.
Druker BJ, Guilhot F, O’Brien SG, Gathmann I, Kantarjian H, Gattermann N, et al. Five-year follow-up of patients receiving imatinib for chronic myeloid leukemia. N Engl J Med. 2006;355(23):2408–17.
Hochhaus A, Larson RA, Guilhot F, Radich JP, Branford S, Hughes TP, et al. Long-term outcomes of imatinib treatment for chronic myeloid leukemia. N Engl J Med. 2017;376(10):917–27.
Kizaki M, Okamoto S, Tauchi T, et al. Current and future perspectives on the TARGET system: the registration system for Glivec established by the JSH. Int J Hematol. 2008;88(4):409–17.
Tauchi T, Kizaki M, Okamoto S, Tanaka H, Tanimoto M, Inokuchi K, et al. Seven-year follow-up of patients receiving imatinib for the treatment of newly diagnosed chronic myelogenous leukemia by the TARGET system. Leuk Res. 2011;35(5):585–90.
JSH. Clinical practice guidelines in hematology malignancy. In: Usui N, Kizaki M, Shimoda K, Takahashi N, editors. CML/MPN. Tokyo: Kanehara Shuppan, Co. Ltd.; 2013.
Baccarani M, Deininger MW, Rosti G, Hochhaus A, Soverini S, Apperley JF, et al. European LeukemiaNet recommendations for the management of chronic myeloid leukemia: 2013. Blood. 2013;122(6):872–84.
Graham SM, Jorgensen HG, Allan E, Pearson C, Alcorn MJ, Richmond L, et al. Primitive, quiescent, Philadelphia-positive stem cells from patients with chronic myeloid leukemia are insensitive to STI571 in vitro. Blood. 2002;99(1):319–25.
Corbin AS, Agarwal A, Loriaux M, Cortes J, Deininger MW, Druker BJ. Human chronic myeloid leukemia stem cells are insensitive to imatinib despite inhibition of BCR-ABL activity. J Clin Investig. 2011;121(1):396–409.
Hamilton A, Helgason GV, Schemionek M, Zhang B, Myssina S, Allan EK, et al. Chronic myeloid leukemia stem cells are not dependent on Bcr-Abl kinase activity for their survival. Blood. 2012;119(6):1501–10.
Barrett AJ, Ito S. The role of stem cell transplantation for chronic myelogenous leukemia in the 21st century. Blood. 2015;125(21):3230–5.
Gratwohl A, Brand R, Apperley J, Crawley C, Ruutu T, Corradini P, et al. Allogeneic hematopoietic stem cell transplantation for chronic myeloid leukemia in Europe 2006: transplant activity, long-term data and current results. An analysis by the Chronic Leukemia Working Party of the European Group for Blood and Marrow Transplantation (EBMT). Haematologica. 2006;91(4):513–21.
Mahon FX, Rea D, Guilhot J, Guilhot F, Huguet F, Nicolini F, et al. Discontinuation of imatinib in patients with chronic myeloid leukaemia who have maintained complete molecular remission for at least 2 years: the prospective, multicentre stop imatinib (STIM) trial. Lancet Oncol. 2010;11(11):1029–35.
Etienne G, Guilhot J, Rea D, Rigal-Huguet F, Nicolini F, Charbonnier A, et al. Long-term follow-up of the French stop imatinib (STIM1) study in patients with chronic myeloid leukemia. J Clin Oncol. 2017;35(3):298–305.
Ross DM, Branford S, Seymour JF, Schwarer AP, Arthur C, Yeung DT, et al. Safety and efficacy of imatinib cessation for CML patients with stable undetectable minimal residual disease: results from the TWISTER study. Blood. 2013;122(4):515–22.
Rousselot P, Charbonnier A, Cony-Makhoul P, Agape P, Nicolini FE, Varet B, et al. Loss of major molecular response as a trigger for restarting tyrosine kinase inhibitor therapy in patients with chronic-phase chronic myelogenous leukemia who have stopped imatinib after durable undetectable disease. J Clin Oncol. 2014;32(5):424–30.
Imagawa J, Tanaka H, Okada M, Nakamae H, Hino M, Murai K, et al. Discontinuation of dasatinib in patients with chronic myeloid leukaemia who have maintained deep molecular response for longer than 1 year (DADI trial): a multicentre phase 2 trial. Lancet Haematol. 2015;2(12):e528–35.
Lee SE, Choi SY, Song HY, Kim SH, Choi MY, Park JS, et al. Imatinib withdrawal syndrome and longer duration of imatinib have a close association with a lower molecular relapse after treatment discontinuation: the KID study. Haematologica. 2016;101(6):717–23.
Rea D, Nicolini FE, Tulliez M, Guilhot F, Guilhot J, Guerci-Bresler A, et al. Discontinuation of dasatinib or nilotinib in chronic myeloid leukemia: interim analysis of the STOP 2G-TKI study. Blood. 2017;129(7):846–54.
Rea D, Cayuela JM. Treatment-free remission in patients with chronic myeloid leukemia. Int J Hematol. 2017;. doi:10.1007/s12185-017-2295-0.
Matsuki E, Ono Y, Sakurai M, Kunimoto H, Ishizawa J, Shimizu T, et al. Discontinuation of imatinib in patients with CML and sustained complete molecular response (CMR) for over 2 years in the Japanese population—an interim analysis of KEIO STIM study. Blood. 2011;118(21):1608.
Takahashi N, Kyo T, Maeda Y, Sugihara T, Usuki K, Kawaguchi T, et al. Discontinuation of imatinib in Japanese patients with chronic myeloid leukemia. Haematologica. 2012;97(6):903–6.
Mita A, Miyamura K, Hino M, Watakabe K, Takahashi K, Yoshimoto M, et al. Evaluating sensitivity of Ipsogen BCR-ABL1 Mbcr IS-MMR DX Kit for scoring molecular response. J Blood Disord Transfus. 2015;6(5):314.
Kanda Y. Investigation of the freely available easy-to-use software ‘EZR’ for medical statistics. Bone Marrow Transplant. 2013;48(3):452–8.
NCCN. NCCN clinical practice guidelines in oncology. Chronic myeloid leukemia; Version 2. 2017;MS18−19.
Mahon F, Richter J, Guilhot J, Hjorth-Hansen H, Almeida A, Janssen JWM, et al. Cessation of tyrosine kinase inhibitors treatment in chronic myeloid leukemia patients with deep molecular response: results of the Euro-Ski trial. Blood. 2016;128(22):787.
Ilander M, Olsson-Stromberg U, Schlums H, Guilhot J, Bruck O, Lahteenmaki H, et al. Increased proportion of mature NK cells is associated with successful imatinib discontinuation in chronic myeloid leukemia. Leukemia. 2017;31(5):1108–16.
Saussele S, Richter J, Hochhaus A, Mahon FX. The concept of treatment-free remission in chronic myeloid leukemia. Leukemia. 2016;30(8):1638–47.
Michor F, Hughes TP, Iwasa Y, Branford S, Shah NP, Sawyers CL, et al. Dynamics of chronic myeloid leukaemia. Nature. 2005;435(7046):1267–70.
Roeder I, Horn M, Glauche I, Hochhaus A, Mueller MC, Loeffler M. Dynamic modeling of imatinib-treated chronic myeloid leukemia: functional insights and clinical implications. Nat Med. 2006;12(10):1181–4.
Deininger M. Hematology: curing CML with imatinib—a dream come true? Nat Rev Clin Oncol. 2011;8(3):127–8.
Cross NC, White HE, Colomer D, Ehrencrona H, Foroni L, Gottardi E, et al. Laboratory recommendations for scoring deep molecular responses following treatment for chronic myeloid leukemia. Leukemia. 2015;29(5):999–1003.
Mori S, Vagge E, le Coutre P, Abruzzese E, Martino B, Pungolino E, et al. Age and dPCR can predict relapse in CML patients who discontinued imatinib: the ISAV study. Am J Hematol. 2015;90(10):910–4.
Hughes TP, Boquimpani CM, Takahashi N, Benyamini N, Clementino NC, Shuvaev V, et al. Treatment-free remission in patients with chronic myeloid leukemia in chronic phase according to reasons for switching from imatinib to nilotinib: subgroup analysis from ENESTop. Blood. 2016;128(22):792.
Acknowledgements
The authors would like to thank the investigators and clinical research coordinators of the sites in the JALSG study group and all of the patients who participated in this study. The Ipsogen BCR-ABL1M-BCR IS-PCR kits was provided by Sysmex Co., Ltd., and IS-PCR analysis was performed at the central laboratory of Sysmex Co., Ltd. We thank Ms. Mika Yoshimura and Mr. Yoshiro Ikeuchi at Sysmex Co., Ltd. for their collaboration. We also thank Ms. Saori Takahashi at Akita University for collecting the data and conducting central monitoring of this study. This study was supported by the Practical Research for Innovative Cancer Control program of the Japan Agency for Medical Research and Development (AMED 15ck0106189h0001, 16ck0106189h0002, 17ck0106189h0003).
Author information
Authors and Affiliations
Consortia
Corresponding author
Ethics declarations
Conflict of interest
Naoto Takahashi reports grants from Japan Agency for Medical Research and Development, non-financial support from Sysmex Co., Ltd., personal fees from NPO JALSG, during the conduct of the study; grants and personal fees from Novartis Pharma K.K., grants and personal fees from Otsuka Pharmaceutical Co., Ltd., grants and personal fees from Pfizer Japan Inc., personal fees from Bristol-Myers Squibb K. K., outside the submitted work. Tetsuzo Tauchi reports grants and other from Novartis Pharma K.K., grants and other from Pfizer Japan Inc., other from Bristol-Myers Squibb K. K., other from Otsuka Pharmaceutical Co., Ltd., during the conduct of the study. Koichi Miyamura reports personal fees from Novartis Pharma K.K., personal fees from Otsuka Pharmaceutical Co., Ltd., personal fees from Bristol-Myers Squibb K. K., personal fees from Pfizer Japan Inc., outside the submitted work. Kensuke Usuki reports personal fees from Novartis Pharma K.K., grants from Fujimoto Pharmaceutical, grants from Otsuka Pharmaceutical Co., Ltd., grants from Sumitomo Dainippon Pharma Co., Ltd., grants from Kyowa Hakko Kirin Co., Ltd., grants from Daiichi Sankyo Co., Ltd., outside the submitted work. Itaru Matsumura reports personal fees from Novartis Pharma K.K., personal fees from Bristol-Myers Squibb K. K., personal fees from Pfizer Japan Inc., personal fees from Otsuka Pharmaceutical Co., Ltd., during the conduct of the study. Yosuke Minami reports grants from Kyowa Hakko Kirin Co., Ltd., grants from Novartis Pharma K.K., grants from Bristol-Myers Squibb K. K., outside the submitted work. Noriko Usui reports personal fees from CIMIC Co., Ltd., personal fees from Takeda Bio Development Center, personal fees from Lilly Japan, personal fees from Pfizer Japan Inc., grants from Pfizer Japan Inc., personal fees from Nippon Boehringer Ingelheim Co., Ltd., grants from Sysmex Co., Ltd., personal fees from Jansen Pharm Co, Ltd., personal fees from Zenyaku Kogyo Co, Ltd., personal fees from Kyowa Hakko Kirin Co., Ltd., grants from Kyowa Hakko Kirin Co., Ltd., personal fees from Otsuka Pharmaceutical Co., Ltd., personal fees from Celgene K. K., personal fees from SymBio Pharm Co, Ltd., personal fees from Huya Bioscience International, personal fees from Astellas Pharma Inc., personal fees from Chugai Pharmaceutical Co. Ltd., grants from Bristol-Myers Squibb K. K., personal fees from Bristol-Myers Squibb K. K., grants from Novartis Pharma K.K., grants from Nippon Shinyaku Co. Ltd., grants from Fujimoto Pharmaceutical, grants from Celgene K. K., outside the submitted work. Tetsuya Fukuda reports personal fees from Novartis Pharma K.K., outside the submitted work. Yoshiko Atsuta reports personal fees and other from Otsuka Pharmaceutical Co., Ltd., personal fees and other from Bristol-Myers Squibb K. K., personal fees from Mochida Pharmaceutical Co., Ltd., personal fees from Kyowa Hakko Kirin Co., Ltd., outside the submitted work. Yukio Kobayashi reports personal fees from Pfizer Japan Inc., personal fees from Otsuka Pharmaceutical Co., Ltd., personal fees from Daiichi Sankyo Co., Ltd., personal fees from CIMIC Co., Ltd., outside the submitted work. Hitoshi Kiyoi reports grants from Japan Agency for Medical Research and Development, during the conduct of the study; grants from Chugai Pharmaceutical Co. Ltd., grants and personal fees from Bristol-Myers Squibb K. K., grants from Kyowa Hakko Kirin Co. Ltd., grants from FUJIFILM Corporation, grants from Nippon Boehringer Ingelheim Co., Ltd., grants and personal fees from Astellas Pharma Inc., grants from Celgene K. K., personal fees from Daiichi Sankyo Co. Ltd., grants and personal fees from Pfizer Japan Inc., grants from Nippon Shinyaku Co. Ltd., grants from Eisai Co. Ltd., grants from Takeda Pharmaceutical Co. Ltd., grants from Ono Pharmaceutical Co. Ltd., grants from Japan Blood Products Organization, outside the submitted work. Yasushi Miyazaki reports personal fees from Sumitomo Dainippon Pharma Co., Ltd., grants and personal fees from Kyowa Hakko Kirin Co., Ltd., personal fees from Novartis Pharma K.K., personal fees from Celgene K. K., personal fees from Shinbio, grants from Chugai Pharmaceutical Co. Ltd., grants from Takeda Pharmaceutical Co. Ltd., outside the submitted work. Tomoki Naoe reports grants from Sumitomo Dainippon Pharma Co., Ltd., grants from Fujifilm Corporation, grants from Astellas Pharma Inc., personal fees from Nippon Boehringer Ingelheim Co., Ltd., grants and personal fees from Otsuka Pharmaceutical Co., Ltd., grants from Toyoma Chemical Co., Ltd., outside the submitted work; In addition, TN has a patent Fujifilm Corporation pending. The other authors declare that they have no conflict of interest.
Electronic supplementary material
Below is the link to the electronic supplementary material.
About this article
Cite this article
Takahashi, N., Tauchi, T., Kitamura, K. et al. Deeper molecular response is a predictive factor for treatment-free remission after imatinib discontinuation in patients with chronic phase chronic myeloid leukemia: the JALSG-STIM213 study. Int J Hematol 107, 185–193 (2018). https://doi.org/10.1007/s12185-017-2334-x
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12185-017-2334-x