Abstract
It has been suggested that use of recombinant soluble thrombomodulin (rTM) is superior to conventional drugs in treatment of disseminated intravascular coagulation (DIC) complicating acute leukemia. However, its safety and efficacy have not been fully examined in prospective studies. Here, we performed a multicenter prospective study to examine outcomes of rTM treatment for DIC in patients with acute leukemia. Of 33 patients registered in this study, 13 had acute myeloid leukemia (AML), three had acute lymphoblastic leukemia (ALL), and 17 had acute promyelocytic leukemia (APL). The cumulative rates of DIC resolution at day 7 and day 35 were 56 and 81% in AML/ALL and 53 and 77% in APL, respectively. The median time from the initiation of rTM to DIC resolution was 4 days in AML/ALL and 6 days in APL patients. Adverse events related to hemorrhage occurred in two AML/ALL patients (13%) and three APL patients (18%). Of these, one AML/ALL patient died with intracranial hemorrhage, and two APL patients died with intracranial hemorrhage and pulmonary hemorrhage. These results suggest that rTM may improve the survival of acute leukemia patients with DIC by inhibiting early death related to hemorrhagic events, as reported previously.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Disseminated intravascular coagulation (DIC) is a severe condition characterized by bleeding symptoms and organ damage caused by consumptive coagulopathy and microthromboembolism [1]. Acute leukemia is often complicated with DIC due to abnormal expression of coagulation-related factors in leukemic cells and external factors, such as infection and vascular endothelial damage, caused by chemotherapy [1, 2]. Although it can be improved by treatment with the reduction of leukemic cells, until such improvement has been achieved, hemorrhage that can lead to early death may occur. The importance of DIC control has been emphasized, especially in acute promyelocytic leukemia (APL), in which bleeding events are a major cause of treatment failure [1, 3]. Since the introduction of all-trans retinoic acid (ATRA) for APL treatment, the early death rate due to bleeding events has decreased from about 20% to less than 10% in several clinical trials [4–10] with varying definitions of early death, such as death within 7 or 30 days from the start of induction chemotherapy or during induction chemotherapy. However, the results of two population-based studies suggested that in practical settings, the incidence of early death, defined as death within 1 month, was not improved (17 and 19%) even after ATRA treatment, and that control of DIC remains an important issue [11, 12].
Few drugs have been shown to be efficacious for the reduction of early death and improvement of overall survival in patients with acute leukemia and DIC. Rodeghiero et al. performed a retrospective analysis of treatments for DIC complicating APL and found no differences in effects among heparin, antifibrinolytic agent, and supportive therapy [10]. Furthermore, superior effects of dalteparin sodium (low-molecular-weight heparin), danaparoid sodium, and activated protein C for DIC with any disease were demonstrated compared to heparin [13–15]. However, recommendation levels for these drugs in DIC treatment guidelines have not been strong or consistent [16]. Also, no comparative analysis has been performed regarding the effects of proteolytic enzyme inhibitors such as nafamostat and gabexate.
Recombinant soluble thrombomodulin (rTM) is a drug with a different mechanism of action from conventional DIC treatment agents. It can bind to thrombin and activate protein C, prompting anticoagulant activity through activated protein C [17–20]. In a prospective comparative study of DIC in hematological malignancy and infection, rTM was shown to have superior efficacy to heparin [21]. A subset analysis for hematological malignancy also demonstrated the improvement of DIC resolution rate and early death rate related to bleeding. However, this study was insufficient to estimate the impact of rTM on DIC in acute leukemia precisely, since it did not focus on acute leukemia including lymphoma and myeloma cases, and some patients with hematological malignancy treated with rTM did not receive chemotherapeutic agents [21]. After this prospective analysis, several retrospective studies [22–27] were reported regarding the advantages of rTM treatment for DIC in APL and non-APL acute myeloid leukemia (AML) over conventional regimens. Furthermore, post-marketing surveillance studies showed the outcome of rTM treatment for DIC in acute leukemia in a large cohort [25, 26].
Despite the accumulation of retrospective data on the use of rTM for DIC in acute leukemia, few prospective studies on this topic have been reported. In particular, the effect of rTM on DIC in APL has not been examined prospectively, since the former study included only three APL cases [21]. Here, we conducted a multicenter prospective study to confirm the safety and efficacy of rTM for the treatment of DIC in acute leukemia.
Materials and methods
Patients
Between 2011 and 2015, patients were prospectively registered for this study at eight centers belonging to the Tohoku Hematology Forum. Patients aged 18 years or older with acute leukemia who developed DIC at the onset or during treatment were considered eligible. Patients with DIC mainly caused by infection and patients who had not received treatment for acute leukemia were excluded. The diagnosis of DIC was based on the Japan Ministry of Health, Labour and Welfare criteria [28]. This study was carried out in accordance with the principles of the Declaration of Helsinki and approved by all institutional review boards. Written informed consent was provided by all patients according to institutional guidelines. All patients were registered after obtaining informed consent. This study was registered with UMIN, ID000008466.
Treatment
After diagnosis of DIC, administration of rTM at a dose of 380 units/kg was started. In patients with severe renal failure, the dose of rTM was reduced to 130 units/kg. Patients within 7 days after starting chemotherapy, those who developed differentiation syndrome in APL, and those complicated with severe organ failure or with a rapid increase of DIC score were considered to have a high risk of bleeding. In such high-risk patients, it is recommended to perform blood transfusion to maintain platelet count >5 × 107/mL and serum fibrinogen level >150 mg/dL. In the other patients, a platelet count of >3 × 107/mL and fibrinogen level of 100 mg/µL were recommended. Use of freeze-dried concentrated human antithrombin III was allowed, while anticoagulants and fibrinolytic agents other than rTM were not.
Endpoints and statistics
The primary endpoint of this study was DIC resolution rate at 7 days after starting treatment with rTM. DIC resolution was defined as reduction of the DIC score to a level below the DIC criteria [28]. Secondary endpoints were improvement of bleeding symptoms at 7 days after starting treatment, time period between starting rTM treatment and DIC resolution, overall survival at day 35, and total units of blood transfusion until 14 days after starting treatment. DIC resolution rate was assessed as cumulative incidence, considering death without DIC resolution as a competing event. Overall survival was estimated by the Kaplan–Meier method. The Mann-Whitney U test was used to compare laboratory data between cases of bleeding and non-bleeding. p values less than 0.05 were considered significant. Statistical analyses were performed with EZR software version 1.32 [29].
Results
Patient characteristics
Patient characteristics are shown in Table 1. Sixteen patients had AML (n = 13) or acute lymphoblastic leukemia (ALL, n = 3), and 17 had APL. Bleeding symptoms at the start of rTM were observed in four patients with AML/ALL (25%) and nine patients with APL (53%). The hemorrhagic sites were one or two of the following: skin, respiratory tract, nasal cavity, gastrointestinal tract, and genital organs. Although three patients with purpura, genital bleeding, and gastrointestinal bleeding were diagnosed as severe, corresponding to grade 3 with the National Cancer Institute Common Terminology Criteria for Adverse Events (NCI-CTCAE) v4.03, these symptoms were transient and controlled with transfusion of platelets or fresh frozen plasma before starting rTM treatment. The median duration of rTM treatment in AML/ALL patients was 6 days (range 2–17 days), and that in APL patients was 5 days (range 1–34 days).
Efficacy of rTM treatment
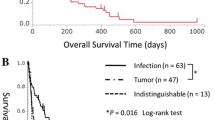
The cumulative incidence of DIC resolution in AML/ALL was 56% [95% confidence interval (CI), 29–77%] on day 7, which increased to 81% (95% CI, 49–94%) at day 35; that for APL was 53% (95% CI, 27–74%) on day 7 and 77% (95% CI, 45–91%) at day 35. As shown in Fig. 1, DIC resolution was achieved before day 14 in most patients. The median times to DIC resolution were 4 days (range 2–12 days) in AML/ALL and 6 days (range 4–12 days) in APL. Among patients with bleeding symptoms at the start of rTM, the disappearance of these symptoms before day 7 occurred in three cases (75%) of AML/ALL and seven cases (78%) of APL. Overall survival at day 35 and the median blood transfusion volume until day 14, in each leukemia type, are shown in Table 2. One AML/ALL patient died with intracranial hemorrhage, and three APL patients died with intracranial hemorrhage, pulmonary hemorrhage, and worsening of acute leukemia. The mortality rates were 6% in AML/ALL and 18% in APL at day 35.
Adverse events
Exacerbation or new onset of bleeding events was observed in two AML/ALL patients (13%) of AML/ALL and three APL patients (18%) (Table 3). Among these cases, two APL patients had experienced mild (grade 1 in NCI-CTCAE) hemorrhagic complications on starting rTM treatment, while the others had no complications related to hemorrhage. Table 3 also shows the site of bleeding, day of onset, and clinical findings for each patient at initiation of rTM treatment. Adverse events other than hemorrhage are shown in Table 4. Five (29%) of the APL patients experienced dyspnea, which was caused by differentiation syndrome.
Comparison of laboratory data between cases with and those without hemorrhage
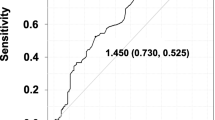
To explore the factors that can predict hemorrhagic adverse events, we compared laboratory data until day 4 in hemorrhage cases with those in non-hemorrhage cases. As shown in Fig. 2, no significant differences were noted in any factors at the day of rTM initiation (day 0) or day 1–2, while at day 3–4, WBC, FDP, D-dimer, and DIC score were significantly worse in hemorrhage cases than in non-hemorrhage cases.
The comparison of laboratory data at each time point after starting rTM between hemorrhage and non-hemorrhage cases. These box plots depict the WBC in PB, platelet count in PB, fibrinogen, FDP, D-dimer, and DIC score at each time point. White boxes indicate non-hemorrhage cases, and dark boxes indicate hemorrhage cases. The differences in data between those cases were assessed by Mann-Whitney U test. Significant difference (p value <0.05) is indicated by an asterisk
Discussion
Early death remains an important issue in the treatment of acute leukemia, and it might be prevented by the control of DIC, since one of the reasons for early death was severe hemorrhagic event associated with DIC [30, 31]. Especially in APL, the early death rate, defined as death within 30 days from diagnosis, remains high, at 17.3–29% in unselected patient cohorts [11, 12, 31, 32]. In AML (non-APL) and ALL, it has been reported that the incidence of major bleeding symptoms is higher in cases with DIC than those without DIC [33], although the early death rate improves year-on-year [34], and the complication of DIC has little impact on overall survival [35]. These results suggested that it might be necessary to reduce bleeding events in the early treatment period through sufficient control of DIC, which could improve the outcome of acute leukemia complicated by DIC.
One option expected to improve DIC treatment in acute leukemia is rTM, since some studies have already indicated that treatment of DIC in acute leukemia with rTM improved not only DIC itself but also overall survival and complications [22, 27]. The current study was performed to examine the safety and efficacy of rTM for DIC complicating acute leukemia and confirmed the results of previous studies [21–27]. The rate of DIC resolution in this study was almost comparable to that of previous studies, whereas the incidence of hemorrhagic adverse events in this study was low compared to the prospective phase III study reported by Saito et al. [21], and rather similar rate to that in previous retrospective studies. These discrepancies are probably due to differences in patient characteristics and the time period in which the treatments were received. In APL, few clinical data from prospective studies were available, and the incidence of hemorrhagic adverse event was higher in this prospective study than in previous retrospective studies [22, 25, 26].
It is unclear whether rTM can contribute to the reduction of hemorrhagic adverse events and mortality compared to other treatments. In the report by Saito et al. [21], the cumulative incidence of bleeding-related adverse events at day 7 was significantly lower in rTM-treated patients than in the heparin group (43.1 vs. 56.1%), whereas the authors did not observe any significant difference in the mortality rate of hematological malignancies at day 28 (17.2 vs. 18%). By contrast, Takezako et al. [27] retrospectively compared the outcomes of rTM treatment with those of low-molecular-weight heparin, and found significant improvement of OS in the rTM group. Since bleeding events and the mortality rate of AML/ALL in the current study were low compared to the former prospective phase III study [21], it is possible that rTM may be a superior treatment to conventional drugs for DIC in AML/ALL in recent cohorts.
With regard to DIC in APL, a few reports have suggested the superiority of rTM to other drugs. Ikezoe et al. [22] reported that treatments with rTM for DIC in APL was associated with a better survival rate than those of conventional treatments including low-molecular-weight heparin. Furthermore, in the report from Matsushita et al. [26], the incidence rates of severe hemorrhage and hemorrhagic early death were 7 and 3.5%, respectively, which are comparable to those in a multicenter prospective study of APL treatment conducted by the Japan Adult Leukemia Study Group (APL97) [7] before rTM became available. Since some population-based studies [11, 12, 31] reported a high incidence of early death in APL, in contrast to studies of selected populations such as APL97, it is possible that rTM can reduce the risk of bleeding in populations that are not eligible for typical clinical trials. However, the hemorrhagic early death rate in this study is higher than that reported by Matsushita et al [26]. One of the possible reasons for this discrepancy is the difference in patient characteristics between the studies, particularly in regard to FDP level at the start of rTM. Median FDP in this study was 109 µg/mL, whereas it was 64.8 µg/mL in the study by Matsushita et al. [26], in which significantly higher FDP was noted in hemorrhagic cases compared to non-hemorrhagic cases.
Several factors such as serum creatinine, fibrinogen, performance status, and peripheral blast count were reported as prognostic for the prediction of fatal hemorrhage during induction chemotherapy for APL [7, 8, 36]. In the period after the introduction of rTM for DIC in APL, Matsushita et al. [26] reported total bilirubin, age, and DIC score as risk factors for severe hemorrhage and early hemorrhagic death. In the current study, one of the two fatal APL patients had high peripheral blast count (27795/µL) and age (79 years old), while the other patient was also older (61 years old) than the median age, although blast count was low (400/µL) (Table 3). Before rTM was clinically available, Park et al. found that age over 55 years was a significant risk factor for early death in APL. A similar result could be applicable to the APL cases treated with rTM. As shown in Fig. 2, none of the examined factors could predict hemorrhagic adverse events. However, the significant differences in WBC, FDP, D-dimer, and DIC score at day 3–4 after starting rTM may reflect differences in treatment response, and suggest that the early control of disease and DIC might be important to prevent hemorrhage. Furthermore, Yanada et al. [7] reported that most severe hemorrhage cases in their study did not reach the recommended levels for platelet count and fibrinogen (platelet count >5 × 107/mL and serum fibrinogen level >150 mg/µL) at the onset of bleeding. In one of our hemorrhagic death cases, it took a few days for platelet count to reach the recommended level, and this time to platelet count elevation might influence the outcome. As described in a previous paper [37], it may be important for preventing hemorrhage to continue frequent blood transfusion based on daily blood tests until coagulation abnormality improves.
This study has some limitations, the first of which is the small number of cases, which prevented accurate estimation of the influence of rTM. Also, this study was not comparative and did not assess the superiority of rTM to conventional treatments. As the purpose of DIC treatment in acute leukemia should be the improvement of survival by reduction of early death related to hemorrhagic events, further prospective studies are needed to confirm the advantages of rTM treatment for DIC in acute leukemia over conventional treatments.
References
Barbui T, Falanga A. Disseminated intravascular coagulation in acute leukemia. Semin Thromb Hemost. 2001;27:593–604.
Rickles FR, Falanga A, Montesinos P, Sanz MA, Brenner B, Barbui T. Bleeding and thrombosis in acute leukemia: what does the future of therapy look like? Thromb Res. 2007;120:S99–106.
Fenaux P. Management of acute promyelocytic leukemia. Eur J Haematol. 1993;50:65–73.
Rodeghiero F, Castaman G. The pathophysiology and treatment of hemorrhagic syndrome of acute promyelocytic leukemia. Leukemia. 1994;8(Suppl 2):S20–6.
Mandelli F, Diverio D, Avvisati G, Luciano A, Barbui T, Bernasconi C, et al. Molecular remission in PML/RAR alpha-positive acute promyelocytic leukemia by combined all-trans retinoic acid and idarubicin (AIDA) therapy. Gruppo Italiano-Malattie Ematologiche Maligne dell’Adulto and Associazione Italiana di Ematologia ed Oncologia Pe. Blood. 1997;90:1014–21.
Fenaux P, Chastang C, Chevret S, Sanz M, Dombret H, Archimbaud E, et al. A randomized comparison of all transretinoic acid (ATRA) followed by chemotherapy and ATRA plus chemotherapy and the role of maintenance therapy in newly diagnosed acute promyelocytic leukemia. The European APL Group. Blood. 1999;94:1192–200.
Yanada M, Matsushita T, Asou N, Kishimoto Y, Tsuzuki M, Maeda Y, et al. Severe hemorrhagic complications during remission induction therapy for acute promyelocytic leukemia: incidence, risk factors, and influence on outcome. Eur J Haematol. 2007;78:213–9.
Di Bona E, Avvisati G, Castaman G, Luce Vegna M, De Sanctis V, Rodeghiero F, et al. Early haemorrhagic morbidity and mortality during remission induction with or without all-trans retinoic acid in acute promyelocytic leukaemia. Br J Haematol. 2000;108:689–95.
Sanz MA, Martín G, Rayón C, Esteve J, González M, Díaz-Mediavilla J, et al. A modified AIDA protocol with anthracycline-based consolidation results in high antileukemic efficacy and reduced toxicity in newly diagnosed PML/RARalpha-positive acute promyelocytic leukemia. PETHEMA group. Blood. 1999;94:3015–21.
Rodeghiero F, Avvisati G, Castaman G, Barbui T, Mandelli F. Early deaths and anti-hemorrhagic treatments in acute promyelocytic leukemia. A GIMEMA retrospective study in 268 consecutive patients. Blood. 1990;75:2112–7.
Park JH, Qiao B, Panageas KS, Schymura MJ, Jurcic JG, Rosenblat TL, et al. Early death rate in acute promyelocytic leukemia remains high despite all-trans retinoic acid. Blood. 2011;118:1248–54.
McClellan JS, Kohrt HE, Coutre S, Gotlib JR, Majeti R, Alizadeh AA, et al. Treatment advances have not improved the early death rate in acute promyelocytic leukemia. Haematologica. 2012;97:133–6.
Sakuragawa N, Hasegawa H, Maki M, Nakagawa M, Nakashima M. Clinical evaluation of low-molecular-weight heparin (FR-860) on disseminated intravascular coagulation (DIC)—a multicenter co-operative double-blind trial in comparison with heparin. Thromb Res. 1993;72:475–500.
Ibbotson T, Perry CM. Danaparoid: a review of its use in thromboembolic and coagulation disorders. Drugs. 2002;62:2283–314.
Aoki N, Matsuda T, Saito H, Takatsuki K, Okajima K, Takahashi H, et al. A comparative double-blind randomized trial of activated protein C and unfractionated heparin in the treatment of disseminated intravascular coagulation. Int J Hematol. 2002;75:540–7.
Wada H, Thachil J, Di Nisio M, Mathew P, Kurosawa S, Gando S, et al. Guidance for diagnosis and treatment of disseminated intravascular coagulation from harmonization of the recommendations from three guidelines. J Thromb Haemost. 2013;11:761–7.
Nakashima M, Kanamaru M, Umemura K, Tsuruta K. Pharmacokinetics and safety of a novel recombinant soluble human thrombomodulin, ART-123, in healthy male volunteers. J Clin Pharmacol. 1998;38:40–4.
Maruyama I. Recombinant thrombomodulin and activated protein C in the treatment of disseminated intravascular coagulation. Thromb Haemost. 1999;82:718–21.
Mohri M, Sugimoto E, Sata M, Asano T. The inhibitory effect of recombinant human soluble thrombomodulin on initiation and extension of coagulation—a comparison with other anticoagulants. Thromb Haemost. 1999;82:1687–93.
Moll S, Lindley C, Pescatore S, Morrison D, Tsuruta K, Mohri M, et al. Phase I study of a novel recombinant human soluble thrombomodulin, ART-123. J Thromb Haemost. 2004;2:1745–51.
Saito H, Maruyama I, Shimazaki S, Yamamoto Y, Aikawa N, Ohno R, et al. Efficacy and safety of recombinant human soluble thrombomodulin (ART-123) in disseminated intravascular coagulation: results of a phase III, randomized, double-blind clinical trial. J Thromb Haemost. 2007;5:31–41.
Ikezoe T, Takeuchi A, Isaka M, Arakawa Y, Iwabu N, Kin T, et al. Recombinant human soluble thrombomodulin safely and effectively rescues acute promyelocytic leukemia patients from disseminated intravascular coagulation. Leuk Res. 2012;36:1398–402.
Kawano N, Kuriyama T, Yoshida S, Yamashita K, Ochiai H, Nakazaki S, et al. Clinical features and treatment outcomes of six patients with disseminated intravascular coagulation resulting from acute promyelocytic leukemia and treated with recombinant human soluble thrombomodulin at a single institution. Intern Med. 2013;52:55–62.
Kawano N, Tasaki A, Kuriyama T, Tahara Y, Yoshida S, Ono N, et al. Effects of recombinant human soluble thrombomodulin treatment for disseminated intravascular coagulation at a single institution–an analysis of 62 cases caused by infectious diseases and 30 cases caused by hematological diseases. Intern Med. 2014;53:205–13.
Asakura H, Takahashi H, Tsuji H, Matsushita T, Ninomiya H, Honda G, et al. Post-marketing surveillance of thrombomodulin alfa, a novel treatment of disseminated intravascular coagulation—safety and efficacy in 1,032 patients with hematologic malignancy. Thromb Res. 2014;133:364–70.
Matsushita T, Watanabe J, Honda G, Mimuro J, Takahashi H, Tsuji H, et al. Thrombomodulin alfa treatment in patients with acute promyelocytic leukemia and disseminated intravascular coagulation: a retrospective analysis of an open-label, multicenter, post-marketing surveillance study cohort. Thromb Res. 2014;133:772–81.
Takezako N, Sekiguchi N, Nagata A, Homma C, Takezako Y, Noto S, et al. Recombinant human thrombomodulin in the treatment of acute myeloid leukemia patients complicated by disseminated intravascular coagulation: retrospective analysis of outcomes between patients treated with heparin and recombinant human thrombomodulin thera. Thromb Res. 2015;136:20–3.
Kobayashi N, Maekawa T, Takada M, Tanaka H, Gonmori H. Criteria for diagnosis of DIC based on the analysis of clinical and laboratory findings in 345 DIC patients collected by the Research Committee on DIC in Japan. Bibl Haematol. 1983;49:265–75.
Kanda Y. Investigation of the freely available easy-to-use software “EZR” for medical statistics. Bone Marrow Transplant. 2013;48:452–8.
Creutzig U, Zimmermann M, Reinhardt D, Dworzak M, Stary J, Lehrnbecher T. Early deaths and treatment-related mortality in children undergoing therapy for acute myeloid leukemia: analysis of the multicenter clinical trials AML-BFM 93 and AML-BFM 98. J Clin Oncol. 2004;22:4384–93.
Lehmann S, Ravn A, Carlsson L, Antunovic P, Deneberg S, Möllgård L, et al. Continuing high early death rate in acute promyelocytic leukemia: a population-based report from the Swedish Adult Acute Leukemia Registry. Leukemia. 2011;25:1128–34.
Rahmé R, Thomas X, Recher C, Vey N, Delaunay J, Deconinck E, et al. Early death in acute promyelocytic leukemia (APL) in French centers: a multicenter study in 399 patients. Leukemia. 2014;28:2422–4.
Sletnes KE, Godal HC, Wisløff F. Disseminated intravascular coagulation (DIC) in adult patients with acute leukaemia. Eur J Haematol. 1995;54:34–8.
Abrahão R, Keogh RH, Lichtensztajn DY, Marcos-Gragera R, Medeiros BC, Coleman MP, et al. Predictors of early death and survival among children, adolescents and young adults with acute myeloid leukaemia in California, 1988–2011: a population-based study. Br J Haematol. 2016;173:292–302.
Uchiumi H, Matsushima T, Yamane A, Doki N, Irisawa H, Saitoh T, et al. Prevalence and clinical characteristics of acute myeloid leukemia associated with disseminated intravascular coagulation. Int J Hematol. 2007;86:137–42.
de la Serna J, Montesinos P, Vellenga E, Rayón C, Parody R, León A, et al. Causes and prognostic factors of remission induction failure in patients with acute promyelocytic leukemia treated with all-trans retinoic acid and idarubicin. Blood. 2008;111:3395–402.
Sanz MA, Grimwade D, Tallman MS, Lowenberg B, Fenaux P, Estey EH, et al. Management of acute promyelocytic leukemia: recommendations from an expert panel on behalf of the European LeukemiaNet. Blood. 2009;113:1875–91.
Acknowledgements
The authors would like to thank all of the physicians and staff of the Tohoku Hematology Forum for their contributions. This study was supported by NPO Tohoku Hematology Expert Meeting.
Author information
Authors and Affiliations
Consortia
Corresponding author
Ethics declarations
Conflict of interest
The authors have no conflicts of interest to declare.
About this article
Cite this article
Yokoyama, H., Takahashi, N., Katsuoka, Y. et al. Evaluation of the safety and efficacy of recombinant soluble thrombomodulin for patients with disseminated intravascular coagulation associated with acute leukemia: multicenter prospective study by the Tohoku Hematology Forum. Int J Hematol 105, 606–613 (2017). https://doi.org/10.1007/s12185-017-2190-8
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12185-017-2190-8