Abstract
There has been considerable interest in the health effects of cocoa products. Cocoa flavonoids have especially been associated with cardiovascular disease (CVD) risk factors. We summarize the effects of total flavonoid and cocoa flavonoid consumption on CVD endpoints in observational studies and intermediate risk factors in experimental designs. From an evidence-based review, there is strong evidence that high cocoa intake lowers blood pressure, improves vascular endothelial function, and potentially increases insulin sensitivity. However, evidence does not support effects on blood lipids and body weight. Total flavonoid intake, and potentially cocoa flavonoid intake, is associated with coronary heart disease mortality in observational studies; however, there is conflicting evidence regarding the dose at which cocoa flavonoids are beneficial. Moreover, because chocolate is often nutritionally energy dense and with added sugar, considerations must be given to caloric balance and body weight. Overall, combining the multiple lines of evidence from experimental and observational studies on the effects of cocoa flavonoids and cocoa intake on cardiovascular risk factors, there is rather strong evidence supporting and demonstrating that cocoa consumption improves several important cardiovascular risk factors and likely reduces the risk of CVD, although more research is needed to further examine etiological mechanisms, demonstrate efficacy on hard clinical CVD endpoints in large-scale randomized trials, as well as carefully estimate attributable disease burden. More importantly, as intake of cocoa is inextricably linked with increased calories in chocolate consumption, further careful risk-benefit analysis is needed to assess whether consuming cocoa in the form of energy-dense chocolate products may yield a net benefit on cardiovascular risks.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Flavonoids are a family of several bioactive substances that include flavones, flavonols, anthocyanins, and flavanols such as proantocyanidins, catechins, and epicatechins. Tea, fruits, and vegetables are rich in flavonoids, but flavonoids are notably abundant in the cocoa solids of the cocoa bean. In recent years, there has been a growing interest in high-flavonoid dark chocolate, fueled by emerging evidence for health benefits of flavonoids. Although a past literature review of total flavonoid consumption identified the potential benefits on cardiovascular disease (CVD) [1], the precise mechanisms of benefits for CVD risk are controversial. Therefore, this evidence-based review focuses on the direct benefits of cocoa and cocoa flavonoids on CVD and potential mechanisms influencing CVD risk.
Nutritional Constituents of Chocolate and Cocoa
The Aztecs and Mayans believed the cocoa tree to be of divine origin, and cocoa to be the “food of the gods” [2]. The original chocolate consumed by the Aztec was a thick, bitter, unsweetened drink, with fat contributing to almost 50% of total content by weight [3]. Adulterations of this original beverage occurred when cocoa was introduced in the 16th century in Europe, together with sugar, tea, and coffee [3]. Sugar and starches were added to mask its bitter taste.
Modern manufacturing of chocolate involves fermentation of the cocoa beans from the Theobroma cacoa followed by drying. This substance is then separated into fat-free cocoa powder and cocoa butter, which are added together in varying proportions to create different chocolate products. Cocoa butter accounts for 50% to 57% of the dry weight of cocoa beans, and the main fats are stearic acid (35%), palmitic acid (25%), and oleic acid (35%). Unsweetened cocoa powder contains 82% non-fat cocoa solids, dark chocolate 23%, and milk chocolate 6% [4]. Because the issue of saturated fat content and stearic acids in chocolate has been previously reviewed [1], this article focuses on the flavonoids of cocoa and effects of overall cocoa and chocolate consumption.
Cocoa and Flavonoid Consumption
Flavonoids as a group are a diverse class of polyphenolic antioxidants (Fig. 1), and are thought to be the primary constituent of cocoa that possesses potential health benefits. Cocoa is predominantly rich in three types of flavonoids: procyanidins, catechins, and epicatechins [2]. However, there are many foods besides cocoa that are also rich in these compounds, as well as others in the flavonoid class.
Chocolate and Cocoa Flavonoid Content
Although chocolate bars are primarily consumed in smaller quantities, they represent the main food source of cocoa flavonoids. Chocolate is especially rich in catechin, epicatechin, and procyanidin, containing an average of 41.50 mg/100 g of epicatechin and 11.99 mg/100 g of catechin [5]. However, modern manufacturing of chocolate may induce losses of more than 80% of the original flavonoids from the cocoa beans [6]. Therefore, flavonoid content of chocolate products may vary depending on the proportion of cocoa solids. Total catechin content of chocolate varies from 46.0 to 61.0 mg/100 g in dark chocolate and 15.3 to 16.3 mg/100 g in milk chocolate [7]. Procyanidin content in commercially available chocolates varies between 9 mg/100 g and 400 mg/100 g [8]. However, a concern is that a 50-g serving of dark chocolate also provides 250 kcal, which is a concern for potential weight gain [5]. In contrast, green tea contains no energy, but provides 8.47 mg/100 g of epicatechin and 2.73 mg/100 g of catechin in addition to flavan-3-ols [5].
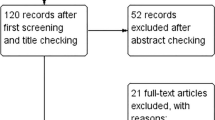
This review is divided into sections on observational studies with CVD endpoints and randomized controlled trials on intermediate CVD risk factors. We begin with the latter, covering different etiologic pathway risk factors.
Effect of Cocoa Flavonoids on Cardiovascular Intermediate Risk Factors in Experimental Trials
Although no long-term trial of cocoa or chocolate yet exists to evaluate hard clinical CVD endpoints, such as myocardial infarction (MI) or stroke, a sizeable body of short-term experimental trials exists to demonstrate effects on intermediate endpoints on various CVD etiology pathways. Notably, short-term randomized clinical trials suggest that flavonoids in chocolate may affect cardiovascular risk through effects on blood pressure (BP), endothelial function, nitric oxide (NO), anti-platelet and anti-inflammatory effects, blood lipids, and insulin resistance [9•].
Blood Pressure
There is strong evidence that high-flavonoid cocoa supplementation lowers systolic (SBP) and diastolic blood pressure (DBP). Four meta-analyses have evaluated the effect of high-flavonoid cocoa products on BP from randomized controlled trials and found strong evidence for a protective association [10–13•]. Changes in mean SBP ranged from −3.2 to −5.88 mmHg and changes in DBP ranged from −2.0 to −3.30 mmHg. The most recent meta-analysis of 21 trials on BP change revealed that dark chocolate (50–70% cocoa), compared to cocoa-free controls, or high-flavanol cocoa compared to low-flavanol cocoa, lowered BP (−3.2 mmHg SBP, −2.0 mmHg DBP). The effects were consistent across flavonoid dose, quality, and duration of trials as well as population demographics; reductions were most notable observed among hypertensive patients (−5 mmHg). These reductions in BP, possibly through effects on angiotensin-I-converting enzyme inhibitor and enhancing NO synthase activity [14–16], are quite pronounced in magnitude of BP reduction and likely of clinical and public health importance. Indeed, a 3- to 5-mm Hg reduction in SBP would yield significant decreases in overall population-wide CVD and mortality burden [17]. Indeed, a recent 3-cohort-pooled prospective study found that two cocoa-rich flavonoids, catechin and epicatechin, was notably associated with lower risk of developing hypertension [18].
Endothelial Function
Short-term cocoa supplementation increased flow-mediated dilation (FMD) in several trials. Eight randomized controlled trials (339 subjects) reported FMD after short-term (15 days to 12 weeks) supplementation with high-flavonoid cocoa among primarily hypertensive or high-risk patients (with history of obesity, diabetes, hypercholesterolemia, or coronary artery disease) [19–25•, 26]. The majority of these trials reported an increased FMD among the treatment arm [19–23, 25•, 26], and improved vascular dilation was observed in primarily high-risk populations [20–25•, 26], although one study even found effects in healthy subjects as well [19]. However, brachial artery FMD systemic arterial compliance was not affected by a flavonol-rich cocoa supplementation [27], and the effect on FMD was lower when sugar was added to the cocoa products [25•, 26–28]. Also for vasodilation, it has been found that cocoa consistently induces NO-dependent vasodilation in the finger or forearm circulation of healthy subjects [15, 19, 29] and in subjects with previous cardiovascular risk factors [20, 22, 30–32], again favorable for vascular function.
Overall, there is a consistent and very strong body of evidence from randomized trials that indicates cocoa flavonoids improve vascular health via reduction of BP and improvement of endothelial function.
Lipid Concentrations
There is conflicting evidence for the effects of high-flavonoid cocoa supplementation on blood lipids. A meta-analysis of five studies, including both short- and long-term clinical trials, found no association between cocoa supplementation and high-density lipoprotein (HDL) or low-density lipoprotein (LDL) cholesterol [12]. A more recent meta-analysis of eight short-term randomized controlled trials (15 days to 12 weeks), with a total of 215 participants, reported a decrease in LDL cholesterol by 5.87 mg/dL (95% CI, −11.13 to −0.61) and a marginal decrease in total cholesterol by 5.82 mg/dL (95% CI, −12.39 to 0.76) [33]. However, there was a large amount of heterogeneity and the association was not observed among high-quality studies. These findings were also limited to low doses of cocoa among participants with cardiovascular risk factors. No difference was observed for triglycerides and HDL cholesterol. In summary, the evidence does not support the effects of cocoa flavonoids on blood lipids.
Insulin Sensitivity
Although few experimental studies have been conducted, preliminary evidence suggests that cocoa flavonoids are associated with insulin sensitivity. Four published randomized controlled trials have evaluated the effect of high-flavonoid cocoa supplementation on Homeostatic Model Assessment of Insulin Resistance (HOMA-IR) and Quantitative Insulin-Sensitivity Check Index (QUICKI) [20, 23, 24, 26]. All studies observed a decrease in HOMA-IR and an increase in QUICKI compared to controls, among both healthy and hypertensive populations. In the three studies that measured Insulin Sensitivity Index (ISI) scores, an increase in ISI score was found, which corresponds to improved insulin sensitivity [20, 24, 34]. Although preliminary evidence from a few randomized controlled trials suggests beneficial effects of cocoa flavonoids on insulin sensitivity, additional large randomized controlled trials are warranted to evaluate this potential effect.
Other Mechanisms
Other pathophysiologic pathways have been proposed by which cocoa flavonoids may affect CVD risk. Daily consumption of cocoa beverages led to significant reductions in platelet activation markers and primary platelet aggregation among healthy volunteers [35]. An in vitro study also suggests immunoregulatory effects of an enriched polyphenol fraction purified from cacao liquor [36]. Additionally, cocoa procyandins may reduce the inflammatory effects of various cytokines (eg, interleukin-5, tumor necrosis factor-α, transforming growth factor-β) [37–41].
Observational Studies on Flavonoids and Cardiovascular Disease
Although flavonoids are a diverse polyphenol class, it is important for etiologic compatibility and robustness to examine cocoa flavonoids in the overall context of total flavonoids on CVD risk. Observational evidence exists for associations between flavonoids from fruits, vegetables, tea, and cocoa consumption and CVD endpoints. Several cross-sectional and prospective cohort studies have found inverse associations between total or specific flavonoid intake and mortality.
First, total flavonoid consumption varies widely between countries. High flavonoid intakes are found in Japan and Australia: among 516 Japanese women, average flavonoid intake was 1,597 μmol/day (380 mg/day), as estimated by 24-hour weighted dietary records. The main sources of flavonoids were tea, onions, grapefruit, and tofu [42]. In a study of 13,858 Australians, total flavonoid consumption was 454 mg/day in adults, with the most important sources being tea (76% of intake) and oranges [43]. Lower flavonoid intakes of approximately 200 mg/day were reported in Europe and the United States. In the UK and Ireland, total daily flavonoid intake was 182 mg and 177 mg (estimated from Food and Agriculture Organization [FAO] Food Balance Sheets), respectively [44]. In a study among 2007 Finnish adults, total flavonoid intake was 207 mg/day, mostly from fruit consumption [45]. In the United States, flavonoid intake was 189.7 mg/day and tea was the major contributor to intake (83% of intake) [46].
Total Flavonoid Intake and Coronary Heart Disease Mortality
The most consistent finding is the association between total flavonoid intake with CVD mortality. A meta-analysis of prospective cohort studies found a combined risk ratio of 0.80 (95% CI, 0.69–0.93) for higher dietary flavonoid intake and coronary heart disease (CHD) [47]. Eight observational studies have found lower risk of CVD mortality for high intakes compared with low intakes of flavonoids [48–57]. Because of the observational nature of these studies, residual confounding by other lifestyle factors may explain part of the association with CVD. For example, in the Zutphen Elderly Study, smoking, lower social economic status, and lower intake of fruits and vegetables were associated with lower intake of flavonoids [58]. Furthermore, it is also of note that total flavonoids include flavones, flavonols, and anthocyanins, which are not present in cocoa. Thus, caution should first be taken when interpreting these findings for cocoa per se.
However, among these cohort studies, one study among Welsh men found no association between flavonoid intake and CHD mortality, possibly because of a high background intake of milk with tea. High milk consumption might affect intestinal flavonoid absorption [59, 60]; however, this mechanism has been debated [60–63]. In the study by Mink et al. [57], other major flavonoid-rich foods were bran, apples, pears, red wine, grapefruit, and strawberries, although it is of note that flavonoids from chocolate alone were independently associated with reduced CVD risk. Main sources in the study by Knekt et al. [56] were onions and apples, which together contributed to 64% of the total intake, and other sources were fruits, berries, sweetened juices and jams (mainly from berries), and vegetables. In the study by Yochum et al. [54], tea, apples, and broccoli were the major contributors to flavonoid intake. In the Zutphen Elderly Study, chocolate accounted for only 3% of catechin intake, whereas black tea accounted for 87% and could be interpreted as perhaps a major factor behind the inverse association with ischemic heart disease [48]. Nevertheless, the Zutphen Elderly Study, in a later report on cocoa [64], found that cocoa intake was, itself, also strongly associated with lower mortality (see later section on cocoa observational studies).
Total Flavonoid Intake and Stroke
There is no evidence for an association between total flavonoid intake and stroke. Most prospective studies found no association between total flavonoid intake and risk of stroke [52, 53, 65]. Only one small study found a significantly lower risk of stroke with higher total flavonoid intake [66]. However, these studies were again for total flavonoids and not cocoa or cocoa flavonoids per se.
Observational Studies of Cocoa Consumption, Cocoa Flavonoids, and Cardiovascular Endpoints
We also examined studies on cocoa intake and cardiovascular disease outcomes. Seven observational studies have looked at associations with cocoa intake specifically. In the prospective Zutphen Elderly Study, a very detailed study of a comprehensive range of dietary items related to cocoa, the highest tertile of cocoa intake (mean, 4.18 g/day) found both significantly lower BP levels (−3.7 mmHg) as well as a remarkable adjusted relative risk of 0.50 (95% CI, 0.32–0.78; P = 0.004 for trend) for cardiovascular mortality and 0.53 (95% CI, 0.39–0.72; P < 0.001) for all-cause mortality compared to the lowest tertile (exclusively those with 0 g/day) [64]. Moreover, in a prospective cohort study of 31,823 Swedish women, Mostofsky et al. [67•] found inverse associations between chocolate intake and heart failure only among elderly women consuming one to three servings of chocolate per month or one to two servings per week; rate ratios were 0.74 (95% CI, 0.58–0.95) and 0.68 (95% CI, 0.50–0.93), respectively. However, in this study, a curvilinear relationship of no association was found for higher servings: rate ratios were 1.09 (95% CI, 0.74–1.62) for those consuming three to six servings per week and 1.23 (95% CI, 0.73–2.08) for those consuming more than 1 serving per day [67•]. The authors suggested a possible J-shaped dose–response curve, where CVD benefits only occur with moderate chocolate intake. One possibility is that the attenuation of benefits with higher consumption may be in part due to excess weight or caloric intake, especially given that the majority of chocolate consumed in Sweden during this time period was milk chocolate (∼30% cocoa solids), which again may or may not have negative interaction in inhibiting effects of flavonoids [60–62]. Nevertheless, the possibility of a J-shaped relationship should not be entirely dismissed, as it was also seen in the Harvard Alumni Health study, which found moderate consumption of chocolate (and candy) associated with lower all-cause mortality (relative risk 0.73; 95% CI, 0.60–0.89), but only in moderation, as a trend toward higher risk was observed in ranges of upper intakes [68].
In the National Heart, Lung, and Blood Institute (NHLBI) Family Heart Study, chocolate consumption was associated with a reduced odds of CHD. In this cross-sectional design study, the odds ratio was 0.43 (95% CI, 0.28–0.67) for chocolate consumption of more than 5 times a week compared to no intake [69]. A reduced risk of both MI and stroke was also observed among a cohort of German adults; relative risk of both outcomes was 0.61 (95% CI, 0.44–0.87), although the inverse association was stronger for stroke [70]. Lower blood pressure only explained 12% of this reduction in risk. Furthermore, chocolate consumption was weakly associated with a decrease in total mortality and nonfatal outcomes among Swedish patients with a previous MI [71]. Conversely, in the Nurses’ Health Study (NHS), chocolate consumption was not associated with CHD incidence [72], although chocolate intake was not well defined in the NHS cohort, unlike in the earlier Zutphen Elderly Study (ZES), which comprehensively assessed cocoa intake using diet records and larger battery of cocoa food items [64]. This method leads to substantially less measurement error, and consequently a strong inverse association was reported for cocoa and mortality in ZES.
These observational studies for cocoa and chocolate consumption overall indicate a strong body of evidence that supports a general trend for an inverse association between not only total flavonoid intake, but also cocoa intake and CVD. However, residual confounding may still be present and causality is still uncertain without larger long-term trials with hard clinical endpoints. When combined with the body of evidence from short-term randomized trial evidence on intermediate CVD risk factors, multiple lines of evidence suggest that cocoa has likely beneficial effects. Nevertheless, future large-scale randomized trials of cocoa and chocolate consumption and hard clinical CVD endpoints would be highly welcome to clarify effectiveness of an intervention.
Chocolate and Body Weight
Although cocoa flavonoids are associated with lower risk of CVD, consumption of chocolate products particularly dense in energy may be a concern. Average commercially available chocolate consumption is approximately 5.5 kg per person per year, varying between 1.02 and 10.14 kg per person per year across countries [73].
On average, a typical chocolate bar contains 500 kcal per 100 g of product and might tip the energy balance toward excessive calorie consumption, increasing the risk of obesity followed by hypertension, dyslipidemia, and diabetes. Indeed, cocoa has been added as an ingredient in snacks and candy such as chocolate bars, and more recently in regularly eaten foodstuffs such as breakfast cereals (United States) and sandwich toppings (The Netherlands). Moreover, chocolate is viewed as something people claim to crave and need [74]. Competing with the potential benefits of cocoa flavonoids on vascular function, a 50-g serving of dark chocolate provides 250 kcal and added sugar makes up almost half of the weight of dark chocolate, with typical fat content around 30% [5]. Indeed, the direct daily consumption of a 50-g serving of dark chocolate may potentially add up to 91,250 kcal each year. However, it is not clear whether other foods are isocalorically replaced by chocolate, and by how much isocaloric replacement of chocolate intake occurs, which would thereby mitigate the excess calorie estimate. Moreover, dark chocolate also contains the most cocoa flavonoids, and the balance of risks and benefits is yet undetermined. To our knowledge, no experimental studies were designed to assess the effects of chocolate consumption on weight as the primary outcome. Nevertheless, in one trial, consumption of 41 g of chocolate for 6 weeks did not cause weight gain [75].
Added sugar in chocolate is also a concern. Approximately half of the content of an average dark chocolate bar is sugar, providing almost 200 cal of added sugar in the diet for a 100-g chocolate bar. The American Heart Association recommends no more than 100 cal of sugar for women per day, and 150 cal for men, equivalent to one serving of chocolate [76•]. Aside from the controversial status of sugar, it should be noted that the beneficial effects of chocolate on FMD are also reduced when sugar is added to cocoa products [25•, 28].
However, these concerns have not stopped certain researchers from recommending 100 g/day of dark chocolate, as part of a supposedly cardiopreventive “polymeal” dietary pattern [77] (although the seriousness of the recommendation has been questioned given the Christmas holiday publication timing). Ultimately, eating chocolate to increase intake of flavonoids may also be challenging. Indeed, it has been reported in one study that 50% of participants given a chocolate treatment found it difficult to consume 50 g of dark chocolate every day, and 20% considered it an unacceptable long-term treatment option. In contrast, all participants found it easy and acceptable to take a capsule each day for blood pressure [78]. Regarding real-world efficacy, again, no studies have been done to assess whether chocolate consumption replaces consumption of nutrient-dense, low-caloric foods. Therefore, considerations of chocolate consumption, in addition to the potentially beneficial cocoa flavonoid constituents, must also be viewed in the light of its caloric content, body weight implications, degree of isocaloric replacement, and the quality and nutrition of the foods it would displace.
Conclusions
Combining the multiple lines of evidence from experimental and observational studies on the effects of cocoa flavonoids and cocoa intake on cardiovascular risk factors shows there is rather strong evidence supporting and demonstrating that cocoa consumption improves several important cardiovascular risk factors and likely reduces the risk of CVD, although more research is needed to further examine etiologic mechanisms, demonstrate efficacy on hard clinical CVD endpoints in large-scale randomized trials, as well as carefully estimate attributable disease burden. More importantly, as intake of cocoa is inextricably linked with increased calories in chocolate consumption, further careful risk-benefit analysis is needed to assess whether consuming cocoa in the form of energy-dense chocolate products may yield a net benefit on cardiovascular risks.
References
Papers of particular interest, published recently, have been highlighted as: • Of importance
Ding EL, Hutfless SM, Ding X, Girotra S. Chocolate and prevention of cardiovascular disease: a systematic review. Nutr Metab Lond. 2006;3:2.
Wollgas J. The contents and effects of polyphenols in chocolate. Qualitative and quantitative analyses of polyphenols in chocolate and chocolate raw products as well as evaluation of potential implications of chocolate consumption in human health. Gießen, Germany: University of Gießen, Faculty of Agricultural and Nutritional Sciences, Home Economics, and Environmental Management. Institute of Nutritional Sciences; 2004.
Grivetti LE, Shapiro H-Y. Chocolate: history, culture, and heritage. Wiley; 2009.
Miller KB, Hurst WJ, Flannigan N, et al. Survey of commercially available chocolate- and cocoa-containing products in the United States. 2. Comparison of flavan-3-ol content with nonfat cocoa solids, total polyphenols, and percent cacao. J Agric Food Chem. 2009;57(19):9169–80.
Anonymous. USDA database for the flavonoid content of selected foods. Release 2.1 2007. Accessed Oct 31, 2010.
Payne MJ, Hurst WJ, Miller KB, Rank C, Stuart DA. Impact of fermentation, drying, roasting, and Dutch processing on epicatechin and catechin content of cacao beans and cocoa ingredients. J Agric Food Chem. 2010;58(19):10518–27.
Arts IC, van de Putte B, Hollman PC. Catechin contents of foods commonly consumed in The Netherlands. 1. Fruits, vegetables, staple foods, and processed foods. J Agric Food Chem. 2000;48(5):1746–51.
Kris-Etherton PM, Keen CL. Evidence that the antioxidant flavonoids in tea and cocoa are beneficial for cardiovascular health. Curr Opin Lipidol. 2002;13(1):41–9.
• Corti R, Flammer AJ, Hollenberg NK, Luscher TF. Cocoa and cardiovascular health. Circulation. 2009;119(10):1433–41. This is a systematic review of cocoa and cardiovascular disease, with a focus on mechanisms.
Taubert D, Roesen R, Schomig E. Effect of cocoa and tea intake on blood pressure: a meta-analysis. Arch Intern Med. 2007;167(7):626–34.
Desch S, Schmidt J, Kobler D, et al. Effect of cocoa products on blood pressure: systematic review and meta-analysis. Am J Hypertens. 2009;23(1):97–103.
Hooper L, Kroon PA, Rimm EB, et al. Flavonoids, flavonoid-rich foods, and cardiovascular risk: a meta-analysis of randomized controlled trials. Am J Clin Nutr. 2008;88(1):38–50.
• Ried K, Sullivan T, Fakler P, Frank OR, Stocks NP. Does chocolate reduce blood pressure? A meta-analysis. BMC Med. 2010;8:39. This is an updated meta-analysis evaluating randomized controlled trials of cocoa supplementation and blood pressure.
Actis-Goretta L, Ottaviani JI, Fraga CG. Inhibition of angiotensin converting enzyme activity by flavanol-rich foods. J Agric Food Chem. 2006;54:229–34.
Fisher ND, Hughes M, Gerhard-Herman M, Hollenberg NK. Flavanol-rich cocoa induces nitric-oxide-dependent vasodilation in healthy humans. J Hypertens. 2003;21(12):2281–6.
Taubert D, Roesen R, Lehmann C, Jung N, Schomig E. Effects of low habitual cocoa intake on blood pressure and bioactive nitric oxide: a randomized controlled trial. JAMA. 2007;298(1):49–60.
Danaei G, Ding EL, Mozaffarian D, et al. The preventable causes of death in the United States: comparative risk assessment of dietary, lifestyle, and metabolic risk factors. PLoS Med. 2009;6(4):e1000058.
http://www.ajcn.org/content/93/2/338.abstract. Accessed 24 Jan 2011.
Engler MB, Engler MM, Chen CY, et al. Flavonoid-rich dark chocolate improves endothelial function and increases plasma epicatechin concentrations in healthy adults. J Am Coll Nutr. 2004;23(3):197–204.
Grassi D, Necozione S, Lippi C, et al. Cocoa reduces blood pressure and insulin resistance and improves endothelium-dependent vasodilation in hypertensives. Hypertension. 2005;46(2):398–405.
Wang-Polagruto JF, Villablanca AC, Polagruto JA, et al. Chronic consumption of flavanol-rich cocoa improves endothelial function and decreases vascular cell adhesion molecule in hypercholesterolemic postmenopausal women. J Cardiovasc Pharmacol. 2006;47 Suppl 2:S177–86. discussion S206–S179.
Balzer J, Rassaf T, Heiss C, et al. Sustained benefits in vascular function through flavanol-containing cocoa in medicated diabetic patients a double-masked, randomized, controlled trial. J Am Coll Cardiol. 2008;51(22):2141–9.
Davison K, Coates AM, Buckley JD, Howe PR. Effect of cocoa flavanols and exercise on cardiometabolic risk factors in overweight and obese subjects. Int J Obes Lond. 2008;32(8):1289–96.
Grassi D, Desideri G, Necozione S, et al. Blood pressure is reduced and insulin sensitivity increased in glucose-intolerant, hypertensive subjects after 15 days of consuming high-polyphenol dark chocolate. J Nutr. 2008;138(9):1671–6.
• Njike VY, Faridi Z, Shuval K, et al. Effects of sugar-sweetened and sugar-free cocoa on endothelial function in overweight adults. Int J Cardiol. Dec 23 2009. This is the largest randomized controlled trial evaluating the effect of cocoa supplementation on endothelial function. It also compares cocoa products with and without sugar supplementation.
Heiss C, Jahn S, Taylor M, et al. Improvement of endothelial function with dietary flavanols is associated with mobilization of circulating angiogenic cells in patients with coronary artery disease. J Am Coll Cardiol. 2010;56(3):218–24.
Farouque HM, Leung M, Hope SA, et al. Acute and chronic effects of flavanol-rich cocoa on vascular function in subjects with coronary artery disease: a randomized double-blind placebo-controlled study. Clin Sci Lond. 2006;111(1):71–80.
Faridi Z, Njike VY, Dutta S, Ali A, Katz DL. Acute dark chocolate and cocoa ingestion and endothelial function: a randomized controlled crossover trial. Am J Clin Nutr. 2008;88(1):58–63.
Schroeter H, Heiss C, Balzer J, et al. (−)-Epicatechin mediates beneficial effects of flavanol-rich cocoa on vascular function in humans. Proc Natl Acad Sci USA. 2006;103(4):1024–9.
Heiss C, Dejam A, Kleinbongard P, Schewe T, Sies H, Kelm M. Vascular effects of cocoa rich in flavan-3-ols. JAMA. 2003;290:1030–1.
Hermann F, Spieker LE, Ruschitzka F, et al. Dark chocolate improves endothelial and platelet function. Heart. 2006;92(1):119–20.
Heiss C, Kleinbongard P, Dejam A, et al. Acute consumption of flavanol-rich cocoa and the reversal of endothelial dysfunction in smokers. J Am Coll Cardiol. 2005;46(7):1276–83.
Jia L, Liu X, Bai YY, et al. Short-term effect of cocoa product consumption on lipid profile: a meta-analysis of randomized controlled trials. Am J Clin Nutr. 2010;92(1):218–25.
Grassi D, Lippi C, Necozione S, Desideri G, Ferri C. Short-term administration of dark chocolate is followed by a significant increase in insulin sensitivity and a decrease in blood pressure in healthy persons. Am J Clin Nutr. 2005;81(3):611–4.
Murphy KJ, Chronopoulos AK, Singh I, et al. Dietary flavanols and procyanidin oligomers from cocoa (Theobroma cacao) inhibit platelet function. Am J Clin Nutr. 2003;77(6):1466–73.
Sanbongi C, Suzuki N, Sakane T. Polyphenols in chocolate, which have antioxidant activity, modulate immune functions in humans in vitro. Cell Immunol. 1997;177(2):129–36.
Mao T, Van De Water J, Keen CL, Schmitz HH, Gershwin ME. Cocoa procyanidins and human cytokine transcription and secretion. J Nutr. 2000;130(8S Suppl):2093S–9S.
Mao TK, Powell J, Van de Water J, et al. The effect of cocoa procyanidins on the transcription and secretion of interleukin 1 beta in peripheral blood mononuclear cells. Life Sci. 2000;66(15):1377–86.
Mao TK, Van de Water J, Keen CL, Schmitz HH, Gershwin ME. Effect of cocoa flavanols and their related oligomers on the secretion of interleukin-5 in peripheral blood mononuclear cells. J Med Food. 2002;5(1):17–22.
Mao TK, van de Water J, Keen CL, Schmitz HH, Gershwin ME. Modulation of TNF-alpha secretion in peripheral blood mononuclear cells by cocoa flavanols and procyanidins. Dev Immunol. 2002;9(3):135–41.
Mao TK, Van De Water J, Keen CL, Schmitz HH, Gershwin ME. Cocoa flavonols and procyanidins promote transforming growth factor-beta1 homeostasis in peripheral blood mononuclear cells. Exp Biol Medicine Maywood. 2003;228(1):93–9.
Otaki N, Kimira M, Katsumata S, Uehara M, Watanabe S, Suzuki K. Distribution and major sources of flavonoid intakes in the middle-aged Japanese women. J Clin Biochem Nutr. 2009;44(3):231–8.
Johannot L, Somerset SM. Age-related variations in flavonoid intake and sources in the Australian population. Public Health Nutr. 2006;9(8):1045–54.
Beking K, Vieira A. An assessment of dietary flavonoid intake in the UK and Ireland. Int J Food Sci Nutr. Sep 22. http://www.ncbi.nlm.nih.gov/pubmed/20858155.
Ovaskainen ML, Torronen R, Koponen JM, et al. Dietary intake and major food sources of polyphenols in Finnish adults. J Nutr. 2008;138(3):562–6.
Chun OK, Chung SJ, Song WO. Estimated dietary flavonoid intake and major food sources of U.S. adults. J Nutr. 2007;137(5):1244–52.
Huxley RR, Neil HA. The relation between dietary flavonol intake and coronary heart disease mortality: a meta-analysis of prospective cohort studies. Eur J Clin Nutr. 2003;57(8):904–8.
Arts IC, Hollman PC, Feskens EJ, Bueno de Mesquita HB, Kromhout D. Catechin intake might explain the inverse relation between tea consumption and ischemic heart disease: the Zutphen elderly study. Am J Clin Nutr. 2001;74(2):227–32.
Hertog MG, Kromhout D, Aravanis C, et al. Flavonoid intake and long-term risk of coronary heart disease and cancer in the seven countries study. Arch Intern Med. 1995;155(4):381–6.
Rimm EB, Katan MB, Ascherio A, Stampfer MJ, Willett WC. Relation between intake of flavonoids and risk for coronary heart disease in male health professionals. Ann Intern Med. 1996;125(5):384–9.
Hertog MG, Feskens EJ, Hollman PC, Katan MB, Kromhout D. Dietary antioxidant flavonoids and risk of coronary heart disease: the Zutphen elderly study. Lancet. 1993;342(8878):1007–11.
Hirvonen T, Virtamo J, Korhonen P, Albanes D, Pietinen P. Intake of flavonoids, carotenoids, vitamins C and E, and risk of stroke in male smokers. Stroke. 2000;31(10):2301–6.
Arts IC, Jacobs DRJ, Harnack LJ, Gross M, Folsom AR. Dietary catechins in relation to coronary heart disease death among postmenopausal women. Epidemiology. 2001;12(6):668–75.
Yochum L, Kushi LH, Meyer K, Folsom AR. Dietary flavonoid intake and risk of cardiovascular disease in postmenopausal women. Am J Epidemiol. 1999;149(10):943–9.
Knekt P, Kumpulainen J, Jarvinen R, et al. Flavonoid intake and risk of chronic diseases. Am J Clin Nutr. 2002;76(3):560–8.
Knekt P, Jarvinen R, Reunanen A, Maatela J. Flavonoid intake and coronary mortality in Finland: a cohort study. BMJ (Clin Res Ed). 1996;312:478–81.
Mink PJ, Scrafford CG, Barraj LM, et al. Flavonoid intake and cardiovascular disease mortality: a prospective study in postmenopausal women. Am J Clin Nutr. 2007;85(3):895–909.
Arts IC, Hollman PC, Feskens EJ, Bueno de Mesquita HB, Kromhout D. Catechin intake and associated dietary and lifestyle factors in a representative sample of Dutch men and women. Eur J Clin Nutr. 2001;55(2):76–81.
Hertog MG, Sweetnam PM, Fehily AM, Elwood PC, Kromhout D. Antioxidant flavonols and ischemic heart disease in a Welsh population of men: the Caerphilly study. Am J Clin Nutr. 1997;65(5):1489–94.
Serafini M, Bugianesi R, Maiani G, Valtuena S, De Santis S, Crozier A. Plasma antioxidants from chocolate. Nature. 2003;424(6952):1013.
Roura E, Andrés-Lacueva C, Estruch R, et al. Milk does not affect the bioavailability of cocoa powder flavonoid in healthy human. Ann Nutr Metab. 2007;51(6):493–8.
Halliwell B. Plasma antioxidants (communication arising): health benefits of eating chocolate? Nature. 2003;426(6968):787.
Richelle M, Tavazzi I, Enslen M, Offord EA. Plasma kinetics in man of epicatechin from black chocolate. Eur J Clin Nutr. 1999;53(1):22–6.
Buijsse B, Feskens EJ, Kok FJ, Kromhout D. Cocoa intake, blood pressure, and cardiovascular mortality: the Zutphen elderly study. Arch Intern Med. 2006;166(4):411–7.
Sesso HD, Gaziano JM, Liu S, Buring JE. Flavonoid intake and the risk of cardiovascular disease in women. Am J Clin Nutr. 2003;77(6):1400–8.
Keli SO, Hertog MG, Feskens EJ, Kromhout D. Dietary flavonoids, antioxidant vitamins, and incidence of stroke: the Zutphen study. Arch Intern Med. 1996;156(6):637–42.
• Mostofsky E, Levitan EB, Wolk A, Mittleman MA. Chocolate intake and incidence of heart failure/clinical perspective. Circ Heart Fail. 2010;3(5):612–6. This is the largest, most recent prospective cohort study evaluating the effect of chocolate intake on risk of heart failure.
Lee IM, Paffenbarger RSJ. Life is sweet: candy consumption and longevity. BMJ Clin Res Ed. 1998;317(7174):1683–4.
Djoussé L, Hopkins PN, North KE, Pankow JS, Arnett DK, Ellison RC. Chocolate consumption is inversely associated with prevalent coronary heart disease: The National Heart, Lung, and Blood Institute Family Heart Study. Clinical Nutrition. 2011, Corrected Proof. http://www.clinicalnutritionjournal.com/article/S0261-5614(10)00157-3/abstract.
Buijsse B, Weikert C, Drogan D, Bergmann M, Boeing H. Chocolate consumption in relation to blood pressure and risk of cardiovascular disease in German adults. Eur Heart J. 2010;31(13):1616–23.
Janszky I, Mukamal KJ, Ljung R, Ahnve S, Ahlbom A, Hallqvist J. Chocolate consumption and mortality following a first acute myocardial infarction: the Stockholm Heart Epidemiology Program. J Intern Med. 2009;266(3):248–57.
Hu FB, Stampfer MJ, Willett WC. Reply to PM Kris-Etherton et al. Am J Clin Nutr. 2000;72(4):1059–60.
Rusconi M, Conti A. Theobroma cacao L., the Food of the Gods: a scientific approach beyond myths and claims. Pharmacol Res. 2010;6(():5–13.
Rogers PJ, Smit HJ. Food craving and food "addiction": a critical review of the evidence from a biopsychosocial perspective. Pharmacol Biochem Behav. 2000;66(1):3–14.
Kurlandsky S, Stote K. Cardioprotective effects of chocolate and almond consumption in healthy women. Nutr Res (NY NY). 2006;26(10):509–16.
• Johnson RK, Appel LJ, Brands M, et al. Dietary sugars intake and cardiovascular health: a scientific statement from the American Heart Association. Circulation. 2009;120(11):1011–20. This is a scientific statement from the American Heart Association regarding dietary sugar intake and cardiovascular disease.
Franco OH, Bonneux L, de Laet C, Peeters A, Steyerberg EW, Mackenbach JP. The Polymeal: a more natural, safer, and probably tastier (than the Polypill) strategy to reduce cardiovascular disease by more than 75%. BMJ. 2004;329(7480):1447–50.
Ried K, Frank O, Stocks N. Dark chocolate or tomato extract for prehypertension: a randomised controlled trial. BMC Complement Altern Med. 2009;9(1):22.
Disclosure
Scott R. Bauer reports no potential conflict of interest relevant to this article. Eric L. Ding reports no potential conflict of interest relevant to this article. Liesbeth A. Smit reports no potential conflict of interest relevant to this article.
Author information
Authors and Affiliations
Corresponding author
Additional information
Scott R. Bauer and Eric L. Ding contributed equally to the manuscript.
Rights and permissions
About this article
Cite this article
Bauer, S.R., Ding, E.L. & Smit, L.A. Cocoa Consumption, Cocoa Flavonoids, and Effects on Cardiovascular Risk Factors: An Evidence-Based Review. Curr Cardiovasc Risk Rep 5, 120–127 (2011). https://doi.org/10.1007/s12170-011-0157-5
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12170-011-0157-5