Abstract
Background
Although sleep is often associated with waking health behaviors (WHB) such as alcohol consumption, caffeine use, smoking, and exercise, the causal direction of these relationships is unclear.
Purpose
The present study used time series data to examine the temporal dynamics of WHB and sleep characteristics in participants of the Study of Women's Health Across the Nation Sleep Study.
Methods
Three hundred three women completed daily assessments of WHB and wore wrist actigraphs to measure sleep characteristics for the duration of the study (mean = 29.42 days, SD = 6.71).
Results
Vector autoregressive modeling revealed that weekly patterns of sleep and WHB best predicted subsequent sleep and WHB suggesting that the associations between WHB and sleep persist beyond their immediate influence. Some WHB predicted some subsequent sleep characteristics, but sleep did not predict subsequent WHB.
Conclusions
These novel findings provide insight into the temporal dynamics of 24-h behaviors and encourage consideration of both sleep and WHB in health promotion and behavior change efforts.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Chronic illness is a leading cause of morbidity and mortality worldwide [1]. Accordingly, understanding modifiable lifestyle factors that contribute to the development, maintenance, and exacerbation of these diseases, including diet, exercise, and substance use, is of public health and clinical interest [2, 3]. However, an exclusive focus on waking health behaviors (WHB) neglects approximately one third of each day dedicated to sleep. Poor sleep has also been associated with morbidity and mortality [4, 5], and, like WHB, many aspects of sleep are under voluntary behavioral control (e.g., timing, sleep environment). Thus, a 24-h approach to the study of health behaviors that includes both WHB and sleep provides a more comprehensive strategy in which to elucidate behavioral influences on health. Critical to this 24-h approach is a greater understanding of the dynamic relationship between sleep and waking behaviors as each plausibly influences the other.
Several epidemiologic and cross-sectional studies have demonstrated correlations between individual WHB and sleep suggesting that poor WHB and poor sleep often co-occur [6–11]. However, the extent to which this relationship is causal and bidirectional remains to be established. The conceptual framework of 24-h health behaviors posits that WHB influence the homeostatic sleep drive and circadian regulation via a number of physiological and psychosocial pathways. Sleep, in turn, influences WHB through its effects on neural circuitry underlying affective, motivational, and perceptual processes. Thus, sleep and WHB may create a circular pattern which may either enhance or disrupt healthy behaviors. Research endeavors have identified several specific, plausible psychophysiological mechanisms through which WHB may influence sleep and vice versa.
For example, stimulants (e.g., caffeine and nicotine) elicit central nervous system arousal, which can delay sleep onset and decrease time spent in slow-wave (deep) sleep. Further, as stimulant levels decrease throughout the night, withdrawal symptoms increase and disrupt sleep maintenance [6, 12]. As a sedative, alcohol decreases sleep latency, allowing people to initiate sleep more quickly, and increases slow-wave sleep early in the sleep period. However, after the alcohol is metabolized, a rebound effect occurs, increasing time spent in light sleep stages and leading to more frequent awakenings [7, 13]. Exercise may promote sleep via transient increases in pro-inflammatory cytokines [14] and adenosine levels [15]. Exercise may also indirectly improve sleep by promoting other positive health behaviors or reducing depressive or anxiety symptoms [16]. Taken together, these works provide clear theoretical and empirical support for the impact of WHB on sleep.
Conversely, a case may be made for the influence of sleep on WHB. For example, insufficient sleep results in daytime fatigue and impairments in motivation, emotion, and cognitive performance [17, 18], which may, in turn, reduce the practice of healthy behaviors such as exercise. Experimental evidence has demonstrated reduced physical activity in individuals with curtailed sleep, though these findings are not entirely consistent [19]. In addition, an increase in negative affect resulting from poor sleep may increase use of caffeine, alcohol, or nicotine as coping strategies [20, 21]. Further, individuals may increase intake of substances like alcohol in response to poor sleep to “self-medicate” and avoid sleep problems on subsequent nights despite the likely counter-productive effects of this behavioral choice [7, 22]. Individuals may also increase use of stimulants like caffeine or nicotine to combat daytime sleepiness [8].
At present, the extant literature on sleep and WHB suggests the relationship between night and day may be bidirectional. These conclusions are further complicated by inconsistencies in study methodologies and results. Overall, it remains to be seen whether methodological limitations have masked the true temporal patterns between WHB and sleep and the extent to which more temporally distal patterns of behavior may contribute additional predictive power to more proximal mechanisms. Thus, valuable insights may be obtained by more careful examination of the temporal relationships between WHB and sleep.
To further clarify the relationships between WHB and sleep, the present study had two primary research objectives. First, we sought to evaluate the temporal dynamics of 24-h health behaviors by identifying the length of time over which WHB influence sleep and vice versa (i.e., number of past days with the strongest prediction power). As most physiological mechanisms proposed to underlie these relationships would suggest, we hypothesized the length of effect would be relatively brief, suggesting that WHB on any given day would most strongly influence sleep that night and that sleep on any given night would most strongly influence WHB the following day. Second, we examined the directionality of these temporal relationships. The overall pattern of associations between individual WHB (alcohol use, cigarette smoking, caffeine use, and exercise) and sleep characteristics (sleep efficiency, sleep latency, wake after sleep onset, total sleep time, and sleep fragmentation) informed the general question of whether the temporal relationship between WHB and sleep was bidirectional, as the present literature may suggest. In addition, we explored the specific pairs of WHB and sleep characteristics to identify the strongest relationships.
Method
Participants
The Study of Women's Health across the Nation (SWAN) Sleep Study recruited 370 midlife women from four of the seven clinical sites participating in the larger SWAN protocol. The core SWAN Study is an ongoing, longitudinal assessment of women's health and well-being during the menopausal transition [23]. Briefly, participants for the SWAN Sleep Study were recruited from Chicago, IL, Detroit area, MI, Oakland, CA, and Pittsburgh, PA. Participants were excluded from the present analyses if their actigraphy data were invalid (n = 38) or insufficient (i.e., less than 7 consecutive days of daily data, n = 15) or if they were missing covariates (n = 14), resulting in a final sample of 303 women. Excluded participants did not differ from those included in the present analyses on sociodemographic or health characteristics with the exception of medication use. Those excluded were more likely than those included to use medications that impact sleep (p = 0.03).
Procedures
Informed consent was obtained for both core SWAN and SWAN Sleep studies and the Institutional Review Boards of each participating institution approved both study protocols. Length of study duration was one menstrual cycle or up to 35 days, whichever came first, with participants providing an average of 29.4 days of consecutive data (SD = 6.71). Participants completed daily diaries each night at bedtime, which assessed WHB (alcohol use, cigarette smoking, caffeine use, and exercise), and wore a wrist actigraph 24 h per day to ascertain behavioral indices of sleep for the duration of the study. In addition, self-report questionnaires were completed on days 4, 14, and the final day of the study including the Quick Inventory of Depressive Symptomatology (QIDS) [24] and a 10-item version of the State Anxiety Inventory (STAI) [25]. Demographic and health information was collected during the core SWAN annual assessment preceding the SWAN Sleep study.
Measures
Waking Health Behaviors
WHB were assessed by self-report in a daily diary. At bedtime each day, participants were asked to report the number of alcoholic and caffeinated beverages consumed that day and the number of cigarettes they had smoked that day. In addition, women were asked to categorize their exercise for the day as either none, light (e.g., walking or shopping), moderate (e.g., jogging or heavy housework), or vigorous (e.g., running or tennis). Exercise categories were coded as 0–3, respectively.
Sleep
Minimitter Actiwatch-64 devices (AW-64™ MiniMitter by Philips Respironics, Bend, OR, USA) were worn continuously on the nondominant wrist for the duration of the study. Participant movement was recorded in 1-min epochs. Diary data were used to identify the sleep period and sleep/wake status was estimated with a validated algorithm (Actiware version 5.04, Mini-Mitter Co. Inc) [26] using the medium sensitivity threshold for wake detection. From these data, five sleep characteristics were estimated. Total sleep time (TST) was calculated as the total number of minutes spent asleep during the night (not including daytime naps). Sleep latency (SL) was calculated as the number of minutes between the start of the nocturnal sleep period and the onset of sleep. Wake after sleep onset (WASO) was defined as the total minutes of wakefulness during the sleep period after sleep onset. The Fragmentation Index was calculated to quantify the amount of movement and restlessness during the nocturnal sleep period. Finally, sleep efficiency (SE) was calculated as the ratio of TST to the total rest interval, with higher values indicating more efficient sleep.
Covariates
Sociodemographic, health, and menopausal characteristics were evaluated as covariates due to their recognized association with sleep. Current age and marital status (married/living as married, single, or widowed/divorced/separated) were reported by participants and race/ethnicity was self-identified as Caucasian, African-American, or Chinese. Financial strain (a proxy for socioeconomic status) was estimated by a single item that measured difficulty paying for “basics” such as housing, utilities, medical care, and food. Participants indicated whether paying for basics were “very hard”, “somewhat hard”, or “not hard at all”.
Body mass index (BMI; in kilogram per square meter) was computed from measured height and weight as part of the annual core SWAN protocol. General health status was estimated with a single item from the MOS Short-Form Health Survey [27], which asked participants to rate their overall health on a five-point scale (1 = excellent, 2 = very good, 3 = good, 4 = fair, 5 = poor). For the present study, health status ratings were collapsed into two groups (excellent/very good/good and fair/poor). Use of medication that affects sleep was assessed over the course of the study protocol. Both prescription and over-the-counter medications were coded according to the World Health Organization Anatomical Therapeutic Chemical (ATC) classification system; medications with the following ATC codes were considered to affect sleep: N02A (opioids), N03A (antiepileptics), N05B (anxiolytics), N05C (hypnotics and sedatives), N06A (antidepressants), and R06A (antihistamines). Across medication categories, participants were categorized as users (intermittent or frequent) or nonusers.
The Quick Inventory of Depressive Symptomatology-Self Report [24] is a 16-item questionnaire that measures symptoms which represent the nine Diagnostic and Statistical Manual of Mental Disorders, fourth edition diagnostic criteria for major depressive disorder. Possible scores ranged from 0 to 27, with higher scores indicating more depressive symptoms. An abbreviated 10-item form of the STAI [25] was administered to evaluate anxiety symptoms during the past week. Possible scores ranged from 10 to 40 with higher scores indicating higher anxiety. The QIDS and STAI were assessed on days 4, 14, and the final day; values in the present analyses represent the average of each measure across time. Finally, three vasomotor symptoms (VMS; cold sweats, hot flashes, and night sweats) were assessed in the daily diaries. Each night was categorized as having nighttime VMS present (at least one VMS endorsed) or absent (no VMS endorsed), and the percentage of nights that VMS were experienced was calculated for each participant. Nocturnal VMS occur in most women during menopause [28, 29] and may affect both sleep and WHB [30, 31].
Data Analysis
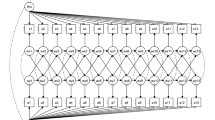
Vector autoregressive (VAR) models and associated tests of Granger causality were used to analyze the data [32, 33]. This approach addressed our two primary research questions: (1) What length of observation provides the strongest prediction in the temporal relationship between WHB and sleep? (2) Is the relationship between WHB and sleep bidirectional and are these patterns consistent across specific WHB and sleep characteristics?
Data were represented as 24-h days. Thus, the present analyses included a total of approximately 5,000 observations (days) reflecting data from the 303 women (exact number of observations varied slightly between models due to missing data). A bivariate VAR model [33] was built for each pair of WHB (alcohol use, caffeine use, cigarette smoking, and exercise) and sleep characteristics (TST, SL, WASO, SE, and sleep fragmentation). These models were fit through maximum likelihood estimation in SAS version 9.2 (Proc Varmax, SAS Institute, Cary, NC, USA). Fixed effects were included to control for sociodemographic and health covariates often associated with sleep and WHB, including age, race, marital status, study site, BMI, general health, use of medications that affect sleep, vasomotor symptoms, menopausal status, and depressive and anxiety symptoms. A random effect was included in the model to account for between-participant variability. Skewed outcome variables were transformed prior to analyses.
Results of VAR models were examined to identify the length of time over which the associations between WHB and sleep were maintained. Due to the weekly nature of many social and occupational rhythms, models of up to 7 days were evaluated. The Bayesian information criterion (BIC) was used for order selection [33] with lower BIC values indicating better model fit. Likelihood ratio tests comparing VAR models (ranging from 2 to 7 days) to first-order models (i.e., models in which only the previous 24 h are included) were used to formally test whether associations between night and day persist beyond a single 24-h period.
To determine whether the relationship between WHB and sleep was bidirectional, we computed F tests of Granger causality from the VAR models. Although results of these analyses do represent a form of temporal causation, the term “predict” is used in place of “cause” in the present manuscript to avoid confusion in interpretation. In a test of Granger causality, a variable X predicts a variable Y if past values of X predict Y after adjusting for past values of Y and other covariates [32]. For example, caffeine consumption predicts SL in a Granger causality model if better predictions of SL in subsequent nights can be obtained by not only considering SL in past nights, but also caffeine consumption during previous days. We individually tested if each of the WHB predicted each of the sleep characteristics and vice versa, which allows for observation of overall patterns and provides information about specific relationships. Interpretation of the direction of significant effects of X on Y is complicated by the inherent multicollinearity stemming from the autocorrelation of each time series. Therefore, individual regression models were conducted to reveal directionality of significant effects of X on Y after controlling for sociodemographic and health covariates. To obtain clear estimates of relationship direction by accounting for natural variability and tolerance effects, values for WHB were recalculated as daily variation from individual's averages, and these values were tested as predictors in these regressions.
Results
The sample was racially/ethnically diverse, with 46.5 % Caucasian, 36.3 % African-American, and 17.2 % Chinese (Table 1). Ages ranged from 48 to 58 years (mean = 52.20, SD = 2.15 years), and most women were pre- or early perimenopausal (68.3 %).
Participants' WHB and sleep characteristics are presented in Table 2. Caffeine consumption was the most frequently endorsed WHB. Participants averaged approximately one-and-a-half caffeinated beverages per day, with only 7.6 % of the sample abstaining from caffeine. Approximately half (51.2 %) of the sample consumed some alcohol and only 10.6 % smoked any cigarettes during the study period. Overall, women did not engage in much daily exercise with 55.5 % averaging less than light daily exercise and an additional 6.9 % reporting no exercise for the duration of the study.
As previously reported, sleep in the SWAN Sleep Study cohort was poor [34, 35]. On average, participants slept less than 6 h per night and exhibited significant sleep fragmentation. Although average sleep latencies were not long (<30 min), participants experienced significant WASO; 34 % of the sample had average WASO values of greater than 1 h.
Temporal Dynamics of WHB and Sleep
Results of VAR models were examined to identify the best model fit (from 1 to 7 days). For all of the WHB–sleep variable pairs, the BIC for the 7-day VAR model was smallest indicating the best model fit. In order to ensure that the 7-day model was not selected as best fitting merely because it included the greatest number of days, models of longer lags were also tested (i.e., 8 and 9 days). Examination of these BICs confirmed that, in comparison to these more extensive models, the 7-day model remained the best fit for the data. Likelihood ratio tests indicated that a 7-day pattern of behavior was significantly more predictive than the behavior of the previous 24 h alone (all ps < 0.001; see Table 3). Therefore, Granger causality tests were performed with the 7-day VAR models to examine the directionality of relationships between weekly WHB and weekly sleep.
Predictive Directionality of WHB and Sleep
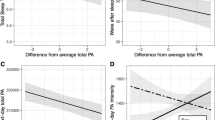
F tests of Granger causality were examined to identify the extent to which individual WHB predicted individual sleep characteristics and vice versa (Fig. 1). After adjusting for study site, age, race, marital status, financial strain, menopausal status, BMI, general health, use of medications that affect sleep, depressive and anxiety symptoms, and VMS, four WHB significantly predicted sleep. Specifically, higher caffeine consumption across the 7 days predicted longer SL (F[7, 5137] = 2.65, p = 0.01) and shorter TST (F[7, 5137] = 3.27, p = 0.002). Higher cigarette smoking (F[7, 5116] = 3.10, p = 0.003) and alcohol consumption (F[7, 4506] = 2.16, p = 0.04) predicted lower SE. No sleep variable significantly predicted any WHB.
Discussion
Despite the public health relevance of both WHB and sleep, research studies often consider them separately failing to identify the potential synergistic effects across a 24-h period. Prior to interpreting the role of 24-h health behaviors in physical or mental health outcomes, it is critical to disentangle the complex interplay between WHB and sleep. The purpose of the present study was to examine the temporal dynamics of WHB and sleep and to evaluate the directionality of these relationships.
The results provided two primary contributions. First, a 7-day model was identified as the best fit to describe temporal relationships among WHB and sleep characteristics. This suggested that weekly patterns of WHB and sleep were more useful in the prediction of subsequent WHB and sleep than more proximal (i.e., 1 day) models. This finding was counter to study hypotheses and is somewhat surprising in light of the nature of the many physiological mechanisms posited to explain these WHB–sleep associations. However, psychosocial and behavioral patterns do tend to follow a weekly cycle and it may be that habitual lifestyle factors represent more robust pathways among 24-h behaviors and possibly to physical health outcomes as well. Additionally, the physiological mechanisms purported to explain WHB–sleep associations may actually be developed and maintained with sustained WHB rather than sporadic WHB. The extent to which this weekly model of 24-h behaviors will extend to other samples is not yet clear. It is plausible that 7 days may not represent the most meaningful window of daily behaviors for all individuals. Replication is particularly important in samples with nonweekly rhythms (e.g., irregular work schedules, partial custody of children, frequent travel). If replicated, this further encourages clinical emphasis on habitual behavior change as opposed to more rigid daily adherence.
The second key finding in the present analyses was that WHB predicted sleep after controlling for previous sleep and several covariates, but sleep did not predict WHB when controlling for previous WHB. The finding that the relationship was not bidirectional was also somewhat unexpected, considering the plausible psychosocial and behavioral pathways through which sleep may influence subsequent WHB (e.g., coping with sleepiness or negative effect, self-medicating to improve subsequent sleep). Not all WHB were significant predictors of all sleep characteristics. In particular, exercise did not significantly predict any sleep characteristics. However, examination of the collection of models clearly provided support for WHB as predictors of sleep, but not vice versa. This finding may suggest that sleep serves as a pathway by which WHB affect physical health rather than contributing an additive effect of behavioral influences on health. In addition, this finding encourages the consideration of WHB assessment and modification as part of a comprehensive approach to sleep management. Sleep hygiene recommendations often encompass WHB (e.g., regular exercise; no caffeine) though the specific recommendations vary widely and the empirical support for each individual recommendations is not always clear [36]. Although sleep hygiene has been found to be ineffective as a stand-alone treatment for insomnia [37], some aspects of it may help individuals with subsyndromal or short-term sleep problems [38], particularly if specific causal relationships can be identified between individual WHB and sleep parameters, as in the present findings.
The present analyses revealed that the temporal relationship between WHB and sleep may not be consistent across all WHB–sleep characteristic pairs. In the present sample, weekly caffeine use predicted longer sleep latency and shorter total sleep time, but not measures of sleep continuity. Use of caffeine in the present sample was reasonably low (mean = 1.51 caffeinated beverages per day) and therefore may have been insufficient to activate physiological effects on other sleep characteristics such as WASO and sleep fragmentation. Weekly alcohol and cigarette use both predicted lower sleep efficiency, but no other sleep characteristics. In the present sample, rates of cigarette use were low (11 % of participants smoked) and most alcohol use was light. As with caffeine, this level of use may have reduced the impact of physiological effects of these substances on sleep characteristics. Sleep efficiency, as the ratio of total time asleep to total time resting in bed, is a more global measure of sleep continuity and thus may have been more sensitive to the subtle effects present in this sample. Thus, the present findings suggest that even use of small amounts of caffeine and alcohol can result in specific sleep impairments.
In contrast, exercise did not significantly predict any sleep characteristics, perhaps as a result of the lack of sensitivity in the daily measure of exercise. For example, duration of exercise was not assessed daily, but duration is a key factor in determining the impact of exercise on sleep [39]. Further, exercise was tested as a continuous variable, but the dose–response relationship between exercise and sleep has not been clearly defined in the current literature [40]. It is possible that the exercise–sleep relationship exists only above a threshold of activity level and, thus, as a result of measurement error or low and infrequent activity of participants, may not have been sufficiently modeled in the present linear analyses. Alternatively, it may be that the bidirectional influence between exercise and sleep follows a pattern distinct from those found for substance use (i.e., caffeine, nicotine, or alcohol). Although exercise and sleep did not have a significant temporal relationship in the current sample, it remains to be seen whether this represents true null findings or simply methodological or sample limitations.
The homogeneity of the sample was a key limitation of the present study. Overall, the frequency of WHB was low, with very few women reporting levels of WHB that would be considered extreme or problematic. Conversely, their overall sleep was poor. It is plausible that the limited range in WHB provided insufficient power to detect the impact of sleep on WHB, resulting in the present null findings. Therefore, the present study cannot clearly determine if sleep exerts a temporal influence on WHB. Future research should examine a wider range of both WHB and sleep characteristics to more appropriately test the influence of sleep on WHB. Based on the present findings of the impact of WHB on sleep, it appears likely that a higher prevalence of WHB will produce similar, but stronger, effect sizes, but it is also possible that these data will reveal null or nonlinear findings. Generalizability is also reduced because women who were excluded from analyses were more likely to use medications that may affect sleep.
While the present study represents a first step toward better understanding of the temporal dynamics of 24-h health behaviors, many additional facets remain to be investigated. The focus on the menopausal transition limited generalizability of both age and gender. Clearly, replication will be required to examine possible variations across participant groups. Three sample characteristics of particular interest for future research include gender, age, and race. Research has identified differential patterns in both WHB and sleep between males and females and across the lifespan [41–46]. Our own data and those of others have shown racial/ethnic group differences in sleep and in WHB [34, 46–48]. Thus, it remains to be seen whether temporal associations between 24-h health behaviors will remain consistent across demographic groups or will require a more individualized lifespan approach.
The study was further limited by the single-item, self-report assessments of WHB, although as a daily assessment these single items did serve to minimize participant burden (as an alternative to more lengthy questionnaires or complicated assessments). Although the parent study evaluated the WHB most commonly associated with sleep, not all possible WHB were assessed. Most notably, diet was not included in daily assessments, but evidence has demonstrated links between sleep and food preference and metabolic function [19, 49]. Future research could incorporate diet assessments as part of a more comprehensive approach.
Despite methodological and sample limitations, the current findings provide a meaningful contribution to the literature and further replication in a variety of populations will help clarify the exact nature of this contribution. If the temporal dynamics of WHB and sleep are shown to be robust across heterogeneous individuals, it will support a general model of the interplay between WHB and sleep that is relevant to a broad majority. Alternatively, if replication is inconsistent across clinical or demographic groups, it encourages further exploration and personalization of the 24-h approach to health behaviors. In any case, the menopausal transition is a critical period of physiologic changes that may affect sleep and is relevant to physical and psychological well-being [50]. In particular, sleep appears to be negatively affected by hormonal changes and VMS during the menopausal transition [30, 51]. Adjusting for menopausal status and VMS in the present analyses allowed for determination of the unique associations between WHB and sleep during this critical period. However, it is important to note that the poor sleep of the women was not entirely accounted for by WHB and covariates. For example, WASO was elevated in the sample, but was not significantly predicted by any WHB or covariates, suggesting that additional factors are likely influencing sleep, such as normal age-related sleep impairment [52]. The nature of the sample also contributed strengths to the study as it was racially diverse and represented four geographic locations across the USA. The study protocol provided additional strengths, including the long duration of consecutive daily data collection (mean = 29 days), the naturalistic study design (as opposed to more artificial laboratory settings), objective assessment of daily sleep, and the assessment of a host of covariates known to be relevant to both WHB and sleep.
A 24-h approach to the study of health behaviors will benefit scientific and public health endeavors in several ways. This comprehensive approach incorporates multiple behavioral components known to be important to both physical and mental health, thus providing a more realistic and complete representation of behavioral factors. Improved understanding of the causal associations between WHB and sleep can identify temporal patterns in the development and maintenance of these behaviors and can better inform behavior change efforts. The present findings encourage incorporation of WHB in programs intended to improve sleep, which may result in more effective and efficient programs of multiple behavior change. Additional progress toward understanding the interplay of 24-h behaviors may provide further insight into the value of incorporating WHB in the treatment of specific sleep deficits (i.e., based on the strength of relationships between specific WHB and sleep characteristics). Further, additive and synergistic effects of sleep and WHB should be more carefully considered in the development and maintenance of health outcomes. Finally, both specific and nonspecific mechanisms may be explored that represent shared and independent pathways between behavior and health.
In sum, the present study provides empirical support for the value of considering a 24-h perspective in the study of health behaviors. Our findings demonstrate that WHB likely influence subsequent sleep while sleep does not appear to affect subsequent WHB and that these relationships are strongest in the context of weekly patterns rather than proximal daily associations. Future work should explore the influence of individual characteristics such as age, gender, and race to determine whether the temporal dynamics of 24-h behaviors vary by demographic group or other psychosocial factors. This individualized understanding of 24-h health behaviors will further enhance behavioral health promotion and disease prevention efforts.
References
World Health Organization. Health topics: Chronic diseases. Accessible at http://www.who.int/topics/chronic_diseases/en/. Accessibility verified November 12, 2012.
Khaw K, Wareham N, Bingham S, Welch A, Luben R, Day N. Combined impact of health behaviors and mortality in men and women: The EPIC-Norfolk prospective population study. PLoS Med. 2008; 5: e12.
Mokdad AH, Stroup DF, Giles WH. Public health surveillance for behavioral risk factors in a changing environment: Recommendations from the Behavioral Risk Factor Surveillance team. MMWR Weekly. 2003; 52: 1-12.
Cappuccio FP, D'Elia L, Strazzullo P, Miller MA. Sleep duration and all-cause mortality: A systematic review and meta-analysis of prospective studies. Sleep. 2010; 33: 585-592.
Zaharna M, Guilleminault C. Sleep, noise and health: Review. Noise & Health. 2010; 12: 64-69.
Phillips BA, Danner FJ. Cigarette smoking and sleep disturbance. Arch Intern Med. 1995; 155: 734-737.
Roehrs T, Roth T. Sleep, sleepiness, sleep disorders and alcohol use and abuse. Sleep Med Rev. 2001; 5: 287-297.
Roehrs T, Roth T. Caffeine: Sleep and daytime sleepiness. Sleep Med Rev. 2008; 12: 153-162.
Schoenborn CA, Adams PF. Sleep duration as a correlate of smoking, alcohol use, leisure time physical inactivity, and obesity among adults: United States, 2004–2006. NCHS Health E-Stats. 2008. Available at http://www.cdc.gov/nchs/data/hestat/sleep04-06/sleep04-06.pdf. Availability verified November 12, 2012
Strine TW, Chapman DP. Associations of frequent sleep insufficiency with health-related quality of life and health behaviors. Sleep Med. 2005; 6: 23-27.
Youngstedt SD, Kline CE. Epidemiology of exercise and sleep. Sleep Biol Rythms. 2006; 4: 215-221.
Zhang L, Samet J, Caffo B, Punjabi NM. Cigarette smoking and nocturnal sleep architecture. Am J Epidemiol. 2006; 164: 529-537.
Feige B, Gann H, Brueck R, et al. Effects of alcohol on polysomnographically recorded sleep in healthy subjects. Alcohol Clin Exp Res. 2006; 30: 1527-1537.
Santos RVT, Tufik S, DeMello MT. Exercise, sleep and cytokines: Is there a relation? Sleep Med Rev. 2007; 11: 231-239.
Dworak M, Diel P, Voss S, Hollmann W, Strüder HK. Intense exercise increases adenosine concentrations in the rat brain: Implications for homeostatic sleep drive. Neurosci. 2007; 150: 789-795.
Buman MP, King AC. Exercise as a treatment to enhance sleep. Am J Lifestyle Med. 2010; 4: 500-515.
Banks S, Dinges DF. Behavioral and physiological consequences of sleep restriction. J Clin Sleep Med. 2007; 3: 519-528.
Walker MP. The role of sleep in cognition and emotion. Ann NY Acad Sci. 2007; 1156: 168-197.
Penev PD. Update on energy homeostasis and insufficient sleep. J Clin Endocrinol Metab. 2012; 97: 1792-1801.
Holahan CJ, Moos RH, Holahan CK, Cronkite RC, Randall PK. Drinking to cope, emotional distress and alcohol use and abuse: A ten-year model. J Stud Alcohol Drugs. 2001; 62: 190-198.
Lang AR, Patrick CJ, Stritzke WK. Alcohol and emotional response: A multidimensional-multilevel analysis. In: Leonard KE, Blane HT, eds. Psychological theories of drinking and alcoholism. 2nd ed. New York: Guilford Press; 1999: 328-371.
Ancoli-Israel S, Roth T. Characteristics of insomnia in the United States: Results of the 1991 National Sleep Foundation Survey. Sleep. 2000; 22: S347-S353.
Sowers MF, Crawford S, Sternfeld B, et al. SWAN: A multi-center, multi-ethnic, community-based cohort study of women and the menopausal transition. In: Lobo R, Kelsey J, Marcus R, eds. Menopause: Biology and pathobiology. San Diego: Academic; 2000: 175-188.
Rush AJ, Carmody TJ, Arnow B, et al. The 16-item Quick Inventory of Depressive Symptomatoloty (QIDS), clinician rating (QIDS-C), and self-report (QIDS- SR): A psychometric evaluation in patients with chronic major depression. Biol Psychiatry. 2003; 54: 573-583.
Spielberger CD. Manual for the State-Trait Anxiety Inventory (Form Y). Menlo Park, CA: Mind Garden; 1983.
Kushida CA, Chang A, Gadkary C, Guilleminault C, Carrillo O, Dement WC. Comparison of actigraphic, polysomnographic, and subjective assessment of sleep parameters in sleep-disordered patients. Sleep Med. 2001; 2: 389-396.
Ware JJ, Sherbourne CD. The MOS 36-item short-form health survey (SF-36): Conceptual framework and item selection. Med Care. 1992; 30: 473-483.
Gold EB, Sternfeld B, Kelsey JL, et al. The relation of demographic and lifestyle factors to symptoms in a multi-ethnic population of 40–55-year-old women. Am J Epidemiol. 2000; 152: 463-473.
Gold EB, Colvin A, Avis N, et al. Longitudinal analysis of vasomotor symptoms and race/ethnicity across the menopausal transition: Study of Women's Health Across the Nation (SWAN). Am J Public Health. 2006; 96: 1226-1235.
Campbell IG, Bromberger JT, Buysse DJ, et al. Evaluation of the association of menopausal status with delta and beta EEG activity during sleep. Sleep. 2011; 34: 1561-1568.
Utian WH. Psychosocial and socioeconomic burden of vasomotor symptoms in menopause: A comprehensive review. Health Qual Life Outcomes. 2005; 3: 1-10.
Granger CWJ. Testing for causality: A personal viewpoint. J Econ Dyn Control. 1980; 2: 329-352.
Shumway RH, Stoffer DS. Time series analysis and its applications. New York: Springer; 2011.
Hall MH, Matthews KA, Kravitz HM, et al. Race and financial strain are independent correlates of sleep in midlife women: The SWAN Sleep Study. Sleep. 2009; 32: 73-82.
Troxel WM, Buysse DJ, Matthews KA, et al. Marital/cohabitation status and history in relation to sleep in midlife women. Sleep. 2010; 33: 973-981.
Stepanski EJ, Wyatt JK. Use of sleep hygiene in the treatment of insomnia. Sleep Med Rev. 2003; 7: 215-225.
Morgenthaler T, Kramer M, Alessi C, et al. Practice parameters for the psychological and behavioral treatment of insomnia: An update. Sleep. 2006; 29: 1415-1419.
Chen PH, Kuo HY, Chueh KH. Sleep hygiene education: Efficacy on sleep quality in working women. J Nurs Res. 2010; 18: 283-289.
Youngstedt SD, O'Connor PJ, Dishman RK. The effects of acute exercise on sleep: A quantitative synthesis. Sleep. 1997; 20: 203-214.
Kline CE, Sui X, Hall MH, et al. Dose–response effects of exercise training on the subjective sleep quality of postmenopausal women: Exploratory analyses of a randomized controlled trial. BMJ Open. 2012; 2: e001044.
Cohen-Mansfield J, Kivity Y. The relationships among health behaviors in older persons. J Aging Health. 2011; 23: 822-842.
Jung KI, Song CH, Ancoli-Israel S, Barrett-Connor E. Gender differences in nighttime sleep and daytime napping as predictors of mortality in older adults: The Rancho–Bernado Study. Sleep Med. 2012; 14(1): 12-19.
Lindberg E, Janson C, Gislason T, Björnsson E, Hetta J, Boman G. Sleep disturbances in a young adult population: Can gender differences be explained by differences in psychological status? Sleep. 1997; 20: 381-387.
Quindry JC, Yount D, O'Bryant H, Rudisill ME. Exercise engagement is differentially motivated by age-dependent factors. Am J Health Behav. 2011; 35: 334-345.
Scharff DP, Homan S, Kreuter M, Brennan L. Factors associated with physical activity in women across the lifespan: Implications for program development. Women Health. 1999; 29: 115-134.
Substance Abuse and Mental Health Services Administration (SAMHSA). Results from the 2008 National Survey on Drug Use and Health: National Findings. Rockville, MD: Substance Abuse and Mental Health Services Administration, Office of Applied Studies; 2009.
Hale L, Do DP. Racial differences in self-reports of sleep duration in a population based study. Sleep. 2007; 30: 1096-1103.
He X, Baker DW. Differences in leisure-time, household, and work-related physical activity by race, ethnicity, and education. J Gen Intern Med. 2005; 20: 259-266.
Chaput JP, Despres JP, Bouchard C, Tremblay A. The association between short sleep duration and weight gain is dependent on disinhibited eating behavior in adults. Sleep. 2011; 34(10): 1291-1297.
Kravitz HM, Zhoa X, Bromberger JT, et al. Sleep disturbance during the menopausal transition in a multi-ethnic community sample of midlife women. Sleep. 2008; 31: 979-990.
Shaver JLF, Zenk SN. Sleep disturbance in menopause. J Womens Health Gend Based Med. 2000; 9: 109-118.
Ohayon MM, Carskadon MA, Guilleminault C, Vitiello MV. Meta-analysis of quantitative sleep parameters from childhood to old age in healthy individuals: Developing normative sleep values across the lifespan. Sleep. 2004; 27: 1255-1273.
Acknowledgments
The Study of Women's Health Across the Nation (SWAN) has grant support from the National Institutes of Health (NIH), DHHS, through the National Institute on Aging (NIA), the National Institute of Nursing Research (NINR), and the NIH Office of Research on Women's Health (Grants U01NR004061, U01AG012505, U01AG012535, U01AG012531, U01AG012539, U01AG012546, U01AG012553, U01AG012554,and U01AG012495). The SWAN Sleep Study was funded by the NIH (grants AG019360, AG019361, AG019362, and AG019363). Sleep data were processed with the support of RR024153. Grant support for LAI was provided by NIH MH019986 and support for CEK was provided by NIH HL082610. Additional grant support for RTK was provided by National Science Foundation DMS-0805050 and support for SDR was provided by NIH HL 104607. The content of this paper is solely the responsibility of the authors and does not necessarily represent the official views of the NSF, NIA, NINR, ORWH, or the NIH.
Clinical Centers
University of Michigan, Ann Arbor, MI, USA (Siobán Harlow, PI 2011–present; MaryFran Sowers, PI 1994–2011); Massachusetts General Hospital, Boston, MA, USA (Joel Finkelstein, PI 1999–present; Robert Neer, PI 1994–1999); Rush University, Rush University Medical Center, Chicago, IL, USA (Howard Kravitz, PI 2009–present; Lynda Powell, PI 1994–2009); University of California, Davis/Kaiser (Ellen Gold, PI); University of California, Los Angeles, CA, USA (Gail Greendale, PI); Albert Einstein College of Medicine, Bronx, NY, USA (Carol Derby, PI 2011–present; Rachel Wildman, PI 2010–2011; Nanette Santoro, PI 2004–2010); University of Medicine and Dentistry–New Jersey Medical School, Newark, NJ, USA (Gerson Weiss, PI 1994–2004); and the University of Pittsburgh, Pittsburgh, PA, USA (Karen Matthews, PI).
NIH Program Office
National Institute on Aging, Bethesda, MD, USA (Winifred Rossi 2012–present; Sherry Sherman 1994–2012; Marcia Ory 1994–2001) and the National Institute of Nursing Research, Bethesda, MD, USA (program officers).
Central Laboratory
University of Michigan, Ann Arbor, MI, USA (Daniel McConnell (Central Ligand Assay Satellite Services).
Coordinating Center
University of Pittsburgh, Pittsburgh, PA, USA (Maria Mori Brooks, PI 2012–present; Kim Sutton-Tyrrell, PI 2001–2012) and New England Research Institutes, Watertown, MA, USA (Sonja McKinlay, PI 1995–2001).
Steering Committee
Susan Johnson, Current Chair; Chris Gallagher, Former Chair.
We thank the study staff at each site and all the women who participated in SWAN.
Conflicts of Interest
With the exception of DJB, the authors have no conflicts of interest to disclose. Dr. Buysse has served as a paid or unpaid consultant on scientific advisory boards for the following companies: Merck, Philips Respironics, Purdue Pharma and General Sleep Corporation. Dr. Buysse has also spoken at single-sponsored educational meetings for Servier. He has also spoken at a single-sponsored lecture for Astellas. Total fees from each of these sources were less than $10,000 per year.
Author information
Authors and Affiliations
Corresponding author
About this article
Cite this article
Irish, L.A., Kline, C.E., Rothenberger, S.D. et al. A 24-hour Approach to the Study of Health Behaviors: Temporal Relationships Between Waking Health Behaviors and Sleep. ann. behav. med. 47, 189–197 (2014). https://doi.org/10.1007/s12160-013-9533-3
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12160-013-9533-3