Abstract
Background
Few studies have evaluated how to combine dietary and physical activity (PA) interventions to enhance adherence.
Purpose
We tested how sequential versus simultaneous diet plus PA interventions affected behavior changes.
Methods
Two hundred participants over age 44 years not meeting national PA and dietary recommendations (daily fruit and vegetable servings and percent of calories from saturated fat) were randomized to one of four 12-month telephone interventions: sequential (exercise first or diet first), simultaneous, or attention control. At 4 months, the other health behavior was added in the sequential arms.
Results
Ninety-three percent of participants were retained through 12 months. At 4 months, only exercise first improved PA, and only the simultaneous and diet-first interventions improved dietary variables. At 12 months, mean levels of all behaviors in the simultaneous arm met recommendations, though not in the exercise- and diet-first arms.
Conclusions
We observed a possible behavioral suppression effect of early dietary intervention on PA that merits investigation.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Many midlife and older adults fall below nationally recommended guidelines for regular physical activity and healthful eating [1–3]. The most effective ways to improve these two key health behaviors remain unclear, particularly with respect to the timing of multiple changes (i.e., whether to promote sequential behavior changes one after the other or intervene on both behaviors at the same time). Support for sequential change is found in social cognitive theory, which emphasizes the importance of breaking complex behavior patterns into smaller, more realistic steps to enhance initial success and promote mastery and self-efficacy for progressive behavior change [4]. The strengths of this approach include building success with one behavior that may transfer to other behaviors [4], i.e., “gateway” or “spillover” effects [5, 6]. However, such spillover effects, which have been proposed for physical activity behavior change [7], may not occur naturally and may need to be specifically taught [8].
A sequential approach may be more responsive to motivational readiness for the behaviors being targeted and may better accommodate differences in the demands underlying different behaviors [9, 10]. Changing a more complex behavior in isolation of other behavior changes may produce greater self-efficacy and habit formation. However, the demands exerted by one behavior change could exact a toll on one's motivation and self-control, potentially making it more difficult to add a second behavior change [11–13].
In contrast to the sequential approach, a simultaneous approach focuses on changing multiple health behaviors at the same time [14]. The simultaneous approach is based on epidemiological evidence indicating that health behaviors tend to cluster among groups in predicting disease outcomes [5]. Certain health behaviors may also share putative social and psychological determinants [5, 6] as well as contextual factors (e.g., social influences and built environments) [15]. Finally, the simultaneous approach may tap into more general “healthy living” values or schemas [14] that encompass multiple behaviors, as well as providing early exposure to multiple health behaviors that could be advantageous for those having to leave the program early.
A potential weakness of a simultaneous approach is that chronic stress and similar life circumstances often make it difficult to initiate and maintain changes in one health behavior, let alone several at once [16].
The current evidence on sequential versus simultaneous behavior change is mixed. For example, in treating hypertension, patients instructed to lose weight and follow a low-sodium diet simultaneously were less adherent to either of these regimens compared to patients for whom the two regimens were introduced separately [17]. Yet, in another hypertension treatment study, patients given the most dietary and physical activity goals simultaneously were more successful in reaching their goals than those given fewer behavioral goals [18].
The specific health behaviors being targeted may make a difference [5]. Researchers have noted that, in particular, diet and physical activity share physiological and behavioral mechanisms that, collectively, can impact energy balance, appetite, and food choices [6, 19]. At least two studies have compared the relative effects of sequential versus simultaneous timing of dietary and physical activity instruction on behavior change. In a study by Vandenalotte et al. [20], two 50-min computer interventions delivered personalized diet and physical activity recommendations sequentially or simultaneously. Between-group differences did not reach statistical significance at either 6 or 24 months. A study by Hyman et al. [21] compared sequential versus simultaneous interventions for physical activity, dietary change (specifically reducing dietary sodium), and smoking cessation in an African-American hypertensive patient sample and found no between-arm behavioral differences across the 18-month study period (although a trend favored greater dietary sodium change in the simultaneous arm).
Goals
The Counseling Advice for Lifestyle Management trial evaluated the 12-month effects of sequentially versus simultaneously delivered telephone interventions to increase regular physical activity and healthful eating in midlife and older adults. Individuals not currently meeting national guidelines in either behavior and reporting time and stress management complaints were targeted, given their particular challenges in making multiple behavior changes [16]. Elevated stress levels can deter individuals from attempting health behavior changes [22], as well as drive premature dropout and nonadherence [23, 24].
Dietary targets were aimed at health promotion, as opposed to weight loss (i.e., caloric restriction was not targeted). We hypothesized that (1) initial behavioral changes in the simultaneous arm would be less robust than in either of the two sequential interventions that began with a single health behavior (either physical activity or dietary change), due to the greater cognitive, behavioral, and motivational demands of a simultaneous behavior change program; but (2) all three interventions would show significantly greater 12-month improvements in both physical activity and dietary behaviors relative to an attention control (stress management) intervention; and (3) given prior evidence that physical activity may be a gateway to other health behavior changes [5, 6], any differences among the two sequential interventions in changing multiple behaviors would favor the arm receiving physical activity instruction first.
Method
Participants and Experimental Design
The study clinical trial registration number is NCT00131105. Study eligibility criteria were the following: ages 45 years and older; not engaged in more than 60 min per week of moderate-to-vigorous physical activity (MVPA) over the previous 6 months, based on self-reported items drawn from the National Health Interview Survey [25]; intake of less than five fruit and vegetable servings per day [26]; intake of more than 10 % of total daily calories from saturated fats [26]; a score of >2 (i.e., “occurring fairly or very often”) on at least one item of the Cohen three-item perceived stress scale (which contained items on inability to control stress and control one's time) [27]; free of any medical condition that would limit participation in moderate-intensity exercise; body mass index of ≤40; free of uncontrolled hypertension and type 2 diabetes requiring oral medications; able to speak and understand English sufficiently to participate in study procedures; regular access to a telephone; not planning to move from the area; and willing to be randomized to any of the four study arms. Recruitment strategies included targeted mass mailings, newspaper ads, and promotion through informal family caregiving organizations, given that family caregivers typically report increased stress and time constraints along with challenges maintaining healthy lifestyles [24]. The study was described as a “healthy lifestyle” study (as opposed to a weight management study), and individuals interested primarily in weight loss were discouraged from enrolling. Individuals who met eligibility requirements during a telephone screen underwent baseline assessment.
Following stratification by gender and family caregiving status (yes/no), subjects were randomly assigned, using the Efron procedure [28], to one of four 12-month telephone interventions delivered by four trained health educators (who were trained to deliver all programs) as follows: (1) a sequential arm with exercise advice delivered first, then nutrition advice added at 4 months (exercise first); (2) a sequential arm with nutrition advice first, then exercise advice added at 4 months (diet first); (3) a simultaneous arm of exercise plus nutrition advice (simultaneous); or (4) a stress management attention control arm (control). Four months was chosen as the time point to introduce the second behavior in the sequential arms, given extensive evidence that significant improvements in the two behaviors occur by 4 months [29, 30]. Stanford University Institutional Review Board approved the study protocol, and individuals signed IRB-approved study informed consent forms in person prior to engaging in baseline assessment activities.
Interventions
The interventions were based on the evidence-based Active Choices program [31–33]. Active Choices has been effective in a range of populations, including improvements in physical activity and dietary quality among chronically stressed adults [24]. It draws on principles and strategies derived from social cognitive theory [4] and the transtheoretical model [34], including facilitating mastery through self-regulatory skill building (e.g., harnessing social support for behavior change, structuring realistic outcome expectations, learning cognitive and behavioral processes of change, and enacting active problem solving to overcome barriers to change) [4].
All arms began with one individual in-person introductory session. Table 1 summarizes the telephone schedule and average minutes of advice delivered in each arm. Total volume of contact was equal across study arms. During the 12-month period, the three experimental arms were scheduled for 15 health advisor telephone contacts that included physical activity advice (15–20 min per call) and 15 that included dietary advice (15–20 min per call). In the two sequential arms, the first 4 months focused on only one behavior (exercise or nutrition), followed by longer (30–40 min) telephone contacts during the remaining 8 months which included both exercise and nutrition advice. The two sequential arms included six additional “booster” calls for the second behavior in the sequence to ensure equivalent exposure to each behavior.
Physical Activity Intervention
For the three arms receiving physical activity advice, the goal was to meet national guidelines of at least 150 min/week of moderate-intensity or more vigorous physical activity, spread across most days of the week [1]. Participants determined the type, location, time of day, and weekly frequency of MVPA. The majority of participants chose to achieve this goal through brisk walking.
Telephone contacts were supplemented with informational mailings and a Yamax Digi-walker pedometer to provide individualized physical activity feedback (AccuSplit, San Jose, CA) [35]. Participants recorded their physical activity (e.g., type, frequency, duration, and pedometer steps) on simple paper calendars and reported it to their advisor during their regular telephone contacts.
Dietary Intervention
Participants randomized to the three experimental arms received a nutrition education program that was matched with the physical activity program on the amount and type of staff contact. Content was based on recommendations from the American Heart Association for a healthy diet and focused on nutritional quality rather than quantity (i.e., calorie counting was not a focus) [36]. Based on their inclusion across a range of national chronic disease prevention recommendations (e.g., cardiovascular disease, cancer, type 2 diabetes, stroke, and hypertension), participants were counseled to reduce total amount of saturated fat and increase fruit and vegetable intake to five to nine servings per day [2, 3]. Participants completed simple paper calendars to track intake and record strategies to reduce saturated fat and increase fruit and vegetable intake and reported this information during their regular telephone contacts. Different nutrition topics were targeted for monitoring and intervention (e.g., reducing high-fat snacks, reducing fats in food preparation, and increasing fruit and vegetable intake). Participants were given homework assignments and detailed reading materials (e.g., recipes).
Stress Management Control Intervention
Individuals in this arm received telephone counseling for skill building in five stress management areas, based on programs developed and evaluated by King et al. and Luskin et al. [37, 38]: progressive muscle relaxation, guided visualization, pleasant events scheduling, sleep hygiene, and time management. Participants were instructed to practice these behaviors throughout the week as a control for the home-based physical activity and dietary behavioral strategies being practiced in the other three arms.
Intervention Fidelity
The four intervention arms included weekly evaluation of the number, content, and length of telephone advising sessions [31]. Advisor summary forms of each contact were reviewed in case management sessions, along with independent review of audiotaped telephone contacts for appropriate content (approximately one third of telephone contacts were randomly selected for review by study investigators and doctoral level clinical psychologists).
Measures
Major study assessments occurred at baseline, 4 months, and 12 months by trained, blinded staff. Upon completion of each assessment, subjects received inexpensive incentive items commensurate with the intervention content they were receiving (e.g., exercise towels for the nutrition/exercise arms; handheld massagers for the stress management arm).
Physical Activity
Elicitation research [39], undertaken in the formative phase of study methods finalization with the stressed population under study, revealed that collection of accelerometry data was overly burdensome to participants and, therefore, not included. We sought to improve the overall stability and accuracy of self-reported physical activity through using a combination of “point prevalence” recall and “usual participation” frequency measures. The recall measure was the Stanford 7-Day Physical Activity Recall (PAR), a validated structured interview in which the participant estimates the amount of time spent each day during the past 7 days in four intensity categories of activity: sleep, and moderate, hard, and very hard physical activity [40]. Inter-rater and test–retest reliabilities are in the 0.69–0.86 range, and concurrent validity, in the 0.75–0.84 range [40, 41].
Given that recalls such as the PAR are vulnerable to “unusual week” effects (i.e., the 7 days being reported on may not reflect participant's typical activities over a longer time period), the Community Healthy Activities Model Program for Seniors (CHAMPS) physical activity questionnaire was also collected. This instrument has been found to provide a valid and reliable estimate of usual physical activity behavior in middle- and older-aged adults [24, 42]. Three-month stability coefficients are in the 0.70–0.84 range in community samples of older adults [42]. The instrument has also been shown to have concurrent validity when compared with interviewer-collected physical activity data [42], as well as sensitivity to change in a number of community samples of midlife and older women and men [24, 32, 33].
Combining these two standard, widely accepted measures promotes more reliable outcomes through stabilizing the random measurement errors of these measures and reducing the chance of type 1 error [43]. Based on national physical activity guidelines [1], average minutes/week in MVPA was the primary physical activity outcome. MVPA values from each measure were determined to have met relevant distributional assumptions prior to combining them. To combine MVPA from the two instruments (for which between-instrument Spearman r coefficient = 0.50), data from each instrument were first standardized using z scores and then averaged. For the percentage of participants for whom information from one or the other instrument was missing, data from the available instrument were used. For descriptive purposes, the z scores have been converted into mean minutes/week of MVPA in tables and figures.
Dietary Intake
Based on current recommendations for a healthy diet [2], the two primary targets for dietary change were daily fruit and vegetable intake and daily percentage of calorie intake from saturated fats. These dietary behaviors were assessed using the Block98 Food Frequency questionnaire, a revised version of the Health Habits and History questionnaire [44]. Participants self-reported the average frequency of consumption of 90 foods and average serving sizes over the past 4 months. Correlations between versions of this questionnaire and 4-day dietary records range from 0.42 to 0.71, and correlations range from 0.41 to 0.73 for essential macronutrients between the questionnaire and unannounced 24-h recalls [44, 45]. It has been shown to be sensitive to change with dietary interventions [24]. The National Cancer Institute's DIETSys program was used to estimate dietary nutrients and quantity of various food groups [46]. A food frequency questionnaire was chosen rather than alternative instruments (e.g., dietary records or repeat 24-h dietary recalls), due to subject burden and cost issues.
Intervention Quality Assurance
Intervention variables, recorded by intervention staff throughout the trial, included number of telephone call attempts for each scheduled contact, number of successful telephone contacts, and minutes per contact.
Process Variables
Parallel forms of Sallis et al.'s Social Support Scales for diet and exercise [47], which included health advisor support, the Stanford self-efficacy questionnaires for physical activity and for dietary behaviors [48], and an outcome expectations/realizations scale [49] were collected at baseline, 4 months, and 12 months.
Sample Size and Statistical Analysis
Based on the previous literature of similar interventions in similarly aged samples [24, 31, 32], a sample size of 45 participants completing the study per cell was judged to be adequate for detecting a 30-min per week difference in MVPA at 80 % power with two-sided alpha set at 0.05 [50]. A similar sample size was judged to be adequate for detecting a 1.5 % difference in percentage of daily calories from saturated fats and a difference of one daily fruit or vegetable [24]. To compensate for potential dropout, an additional 20 participants beyond the a priori powered sample (N = 180) were included, resulting in a final recruitment sample target of 200. Analysis of variance (general linear models) [51] was used to evaluate between-arm differences at baseline.
Intent-to-treat principles were used for the primary outcomes, i.e., physical activity, percent of daily calories from saturated fat, and number of daily fruit and vegetable servings. Three participants completed only a portion of the baseline dietary questionnaire (two from the diet-first arm and one from the control arm) and were therefore not included in analyses, given the primary focus on dietary and physical activity changes across arms (see Fig. 1). For participants with missing or incomplete data at either 4 or 12 months, baseline values were used. This decision was based on evidence indicating that when loss to follow-up is modest and not differential by study arm (see “Results”), such carry-forward procedures produce more conservative estimates relative to multiple imputation procedures [52]. For physical activity, this resulted in baseline imputation for 3 participants at 4 months (1.5 % of sample) and 18 participants at 12 months (9 % of sample). For the dietary outcomes (which were more burdensome to complete, requiring about 90 min to complete at home just prior to the assessment visit relative to 30 min for the combined physical activity instruments, which were completed at the assessment visit), this resulted in baseline imputation for 40 participants at 4 months (20.3 % of sample) and 30 participants at 12 months (15.2 % of sample). There were no between-arm differences for percent of participants with missing or incomplete data at either 4 months [exercise first = 41/50 (82 %); diet first = 42/50 (84 %); simultaneous = 40/50 (80 %); control = 37/50 (74 %); X 2 = 1.82, p = 0.61] or 12 months [exercise first = 42/50 (84 %); diet first = 44/50 (88 %); simultaneous = 44/50 (88 %); control = 40/50 (80 %); X 2 = 1.72, p = 0.63].
Given, as described in the “Introduction,” the distinct questions of interest related to the 4- and 12-month time points, analysis of covariance (ANCOVA, general linear model) [53] was used to assess changes in MVPA and the two dietary targets from baseline to 4 months and baseline to 12 months. Given only three time points, within-person random effects incorporated into random regression models (RRM) become relatively unstable [54]. However, for completeness, we conducted RRM analysis (Proc Mixed, SAS) [53] and found results similar to those using ANCOVA. The more straightforward ANCOVA results are reported. The main effects for arm assignment were modeled with baseline levels of the dependent variable, gender, and family caregiving status (yes vs. no) entered as covariates. As described earlier, z scores representing the MVPA scores averaged across the PAR and CHAMPS measures were used in the analyses to improve the stability of that outcome. The least-squares adjusted means method was used to compare group means for all significant effects [53].
Results
Descriptive Statistics
Participant flow and retention is shown in Fig. 1. Of the 200 participants enrolled, 186 (93 %) were retained through 12 months. Retention was not significantly different across the four arms (exercise first = 48/50, or 96 %; diet first = 46/50, or 92 %; simultaneous = 48/50, or 96 %; control = 44/50, or 88 %; p = 0.33). Those with 12-month data were comparable to those without 12-month data (n = 14) on all major baseline demographic, health, and behavioral variables (p values of >0.14). Descriptive baseline data are shown in Table 2 for selected variables. Raw data are shown to allow for comparisons with other studies and to provide clinically meaningful information. Participants were similar across study arms on the major baseline variables of interest (all p values of ≥0.27). Similar to their age group, the average number of chronic health conditions for the sample was 1.4 ± 1.1. Across arms, approximately 46 % of participants (no between-arm differences) were on medications for chronic conditions, including hypertension, hyperglycemia, hypercholesterolemia, and asthma. The sample also reported baseline stress levels similar to a sample of chronically stressed family caregivers in the same locale [24]. As expected given the intervention focus, there were no significant weight changes across arms.
Overall volume of staff phone contacts (minutes per contact × number of contacts) did not differ significantly across the four arms (F (3, 196) = 2.0, p = 0.11) (see Table 2). Average number of call attempts per scheduled telephone contact also did not differ (range = 1.5–1.7 attempts, p = 0.19). As planned in matching total volume of staff contact, the mean length of calls in the simultaneous arm was longer, by a modest amount, compared to that in the sequential arms (F (3, 196) = 12.5, p = 0.001; see Table 2). The sequential arms did not differ significantly from each other on mean call length (p = 0.54) or number of contacts received (p = 0.58); both received a greater number of phone contacts (as planned to balance overall contact volume) compared to the simultaneous arm (F (3, 196) = 21.2, p < 0.0001).
Rated advisor support at 12 months did not differ significantly across the three experimental arms, but all three arms were higher than controls for support for diet and MVPA (p values of ≤0.03; see Table 2). As expected at 4 months, the exercise-first and simultaneous arms did not differ significantly from each other but reported significantly increased advisor support for physical activity compared to the diet-first and control arms (p values of ≤0.001; see Table 2). Similarly, the diet-first and simultaneous arms did not differ significantly from one another but reported significantly increased 4-month advisor support for dietary change relative to the exercise-first and control arms (p values of <0.0001).
Dietary Change by Arm Assignment
Daily Servings of Fruits and Vegetables
At 4 months, the diet-first and simultaneous arms did not differ significantly from one another on daily fruit and vegetable servings and had higher consumption relative to that of exercise first and control (F (3, 196) = 13.9, p < 0.0001; see Table 2). Exercise first did not differ from the control (p = 0.86). Main effects for gender and caregiver status were not significant (p values of >0.51).
By 12 months, all three experimental arms (exercise-first, diet-first, and simultaneous) did not differ significantly from one another and had higher daily servings of fruits and vegetables relative to control (F (3, 196) = 10.6, p < 0.0001; see Fig. 2, including effect size information). Main effects for gender and caregiver status did not achieve statistical significance (p values of ≥0.58).
Mean daily servings of fruits and vegetables at 12 months, by arm. Means were adjusted by baseline values. *p ≤ 0.0004 vs. control. Effect sizes (Cohen's d): exercise first vs. control, 0.80; diet first vs. control, 1.10; simultaneous vs. control, 0.77; exercise first vs. diet first, 0.28; exercise first vs. simultaneous, 0.07; diet first vs. simultaneous, 0.36
At 12 months, a greater percentage of subjects in diet first (78 %) achieved the national recommendation of five to nine fruit and vegetable servings relative to control (33 %), X 2 (1) = 18.2, p < 0.0001, and exercise first (54 %), X 2 (1) = 5.1, p = 0.02. Other between-arm differences reaching significance were comparisons between exercise first and control, X 2 (1) = 3.8, p = 0.05, and simultaneous (59 %) and control, X2 (1) = 5.9, p = 0.02.
Percent Daily Calories from Saturated Fat
At 4 months, the diet-first and simultaneous arms did not differ significantly from one another and had significantly lower percentages of daily calories from saturated fat relative to exercise first and control (F (3, 193) = 13.2, p < 0.0001; Table 2). Exercise first did not differ significantly from control (p = 0.18). No significant main effects were observed for gender or caregivers status (p values of ≥0.11).
By 12 months, the three experimental arms did not differ from one another and had generally lower percentages of daily calories from saturated fat relative to controls (F (3, 196) = 6.0, p = 0.0006; see Fig. 3, including effect size information), although the least-squares adjusted means test indicated that the difference between exercise first and control was marginally significant (p = 0.056) (p values for other two arms vs. control of ≤0.0008). No significant main effects for either gender or caregiver status were observed.
Mean daily percent calories from saturated fat at 12 months, by arm. Means were adjusted by baseline values. *p ≤ 0.0008 vs. control; †p = 0.056 vs. control. Effect sizes (Cohen's d): exercise first vs. control, 0.34; diet first vs. control, 0.70; simultaneous vs. control, 0.80; exercise first vs. diet first, 0.28; exercise first vs. simultaneous, 0.36; diet first vs. simultaneous, 0.10
At 12 months, a significantly greater percentage of subjects in the diet-first (57 %) and simultaneous arms (57 %) achieved the national recommendation of less than 10 % of daily calories from saturated fat relative to control (31 %), X 2 (1) = 6.0, p = 0.02. All other between-arm differences did not reach statistical significance (exercise-first arm = 40 %). As expected, no significant weight loss was observed across arms at either 4 or 12 months (p values of >0.20).
Physical Activity Change by Arm Assignment
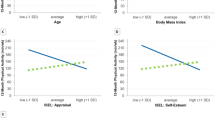
At 4 months, exercise first had significantly greater mean MVPA minutes per week than the other three arms, which did not differ significantly from one another (F (3, 196) = 5.0, p = 0.002; see Table 2). By 12 months, both the exercise-first and simultaneous arms did not differ significantly from one another but had significantly greater MVPA minutes/week than control (F (3, 196) = 2.8, p = 0.04; see Fig. 4, which contains effect size information). For these two arms, the mean MVPA minutes/week was above national recommendations [1]. The diet-first mean MVPA minutes/week fell between those of the other arms and control and did not differ significantly from the other arms (see Fig. 4). While there was no significant main effect for caregiver status, the gender main effect did achieve significance (p = 0.028), with men reporting an imputed mean [standard error (SE)] of 192.6 [36.9] MVPA min/week, while women reported an imputed mean [SE] of 118.3 [11.5] MVPA min/week.
Moderate to vigorous physical activity, mean minutes per week at 12 months, by arm. Means were adjusted by baseline values. *p < 0.02 vs. control. Effect sizes (Cohen's d): exercise first vs. control, 0.56; diet first vs. control, 0.29; simultaneous vs. control, 0.53; exercise first vs. diet first, 0.37; exercise first vs. simultaneous, 0.10; diet first vs. simultaneous, 0.27
At 12 months, a greater percentage of subjects in exercise first (48 %) achieved the nationally recommended guidelines relative to control (22 %), X 2 (1) = 6.3, p = 0.01. Other between-arm comparisons were not statistically significant (diet first = 38 %; simultaneous = 40 %).
Additional Analyses
Evaluation of 12-month multiple behavior change index scores (formed by summing z scores for each health behavior) [43] indicated a significantly higher index score for each of the three experimental arms relative to control, with the experimental arms not differing significantly from each other (F (3, 196) = 6.7, p < 0.001) (data not shown).
Exploration of between-arm changes in social cognitive theory process variables (self-efficacy, outcome expectations/realization, and social support) yielded few between-arm differences or insights pertaining to the pattern of between-arm outcomes observed (data not shown).
As captured on the outcome realizations scale, at 12 months, stress management participants reported significantly greater improvements in stress than the diet-first and simultaneous arms, though not the exercise-first arm (F (3, 160) = 2.7, p < 0.045). The stress management arm also reported significantly greater 12-month improvements in coping with stress relative to the other three arms (F (3, 161) = 3.8, p < 0.01). No other between-arm differences were found on these variables. Paired comparison t tests showed that all four arms had significant decreases in perceived stress levels from baseline to 12 months (p values of <0.003).
Discussion
While interest in enhancing multiple health behavior change has proliferated, few systematic investigations have evaluated the effects of intervention timing, i.e., sequential versus simultaneous delivery, on successful health behavior adoption and maintenance [20, 21]. Strengths of the current study included the matching of overall volume of intervention across the four study arms and a high 12-month retention rate (93 %). We found partial support for the first hypothesis that health behavior changes would be more robust during the initial 4-month period for the two sequential arms relative to the simultaneous arm. While this hypothesis was supported for physical activity (i.e., the exercise-first arm had significantly higher 4-month physical activity than the simultaneous arm), it was not supported for dietary change (i.e., there were no 4-month differences between diet-first and simultaneous arms; both improved relative to control).
The second hypothesis postulating 12-month improvements in diet and physical activity across all three experimental arms relative to control also was partially supported. While 12-month improvements for the simultaneous arm were statistically different from those for control for all three target behaviors (indicating that statistical power was sufficient for all three outcomes), the exercise-first arm attained marginal improvement in percent of daily calories from saturated fat relative to control (at p = 0.056), and the diet-first arm did not significantly improve MVPA relative to control. By 12 months, mean levels in only the simultaneous arm met national recommendations for saturated fat, fruits and vegetables, and MVPA. Meanwhile, at 12 months, the two sequential arms had the largest proportions of participants reaching national recommendations in the behavior area targeted first (i.e., diet for dietary first; MVPA for exercise first). This pattern suggests that changing one health behavior first may help to ensure maintenance of that health behavior but may prove detrimental (at least for some people) for the second health behavior. It is possible that the shorter 8-month advice period for the second behavior in the sequence could have disadvantaged participants. However, the fact that simultaneous arm participants showed little physical activity increase at 4 months, yet were able to reach recommended physical activity levels by 12 months, argues against this possibility.
The poorer performance of diet-first participants in achieving physical activity goals, coupled with the poorer 4-month physical activity performance in the simultaneous arm, suggests that physical activity change may be particularly difficult to achieve when dietary change is already underway. In contrast, exercise first achieved significant improvements in daily fruit and vegetable intake and marginally significant improvements in saturated fat intake, along with significant physical activity improvements. These results provide some support for the premise that initial physical activity change efforts may, at minimum, not unduly impede subsequent dietary change efforts. This may particularly be the case when positive dietary additions (i.e., increasing fruit and vegetable intake), as opposed to restrictions (i.e., reducing saturated fats), are targeted.
An alternative explanation for the differential physical activity results across arms is the intrinsically different demands of changing physical activity versus diet. Given the obligatory nature of eating (i.e., it is already embedded in daily schedules), dietary interventions such as the one targeted in this study typically focus on changes in dietary choices, i.e., substitutions, or additions or deletions to meals. In contrast, increasing physical activity typically means adding a sustained block of activity to people's daily schedules. For the stressed individuals under study, tackling the multi-faceted dietary intervention first [10] may have left less motivational or self-regulatory capacity for adding physical activity, which requires additional time and scheduling adjustments. Such an outcome is commensurate with a “cognitive load” interpretation of self-regulation [12]. This interpretation also may help to explain why participants receiving simultaneous instruction in both health behaviors from the beginning had significantly smaller 4-month MVPA increases compared to those assigned to exercise first. While the two behaviors received equal advisor attention from the start in the simultaneous arm, the dietary change effort may have required more participant attention and cognitive load.
The Active Choices telephone delivery program has demonstrated sustained efficacy for a wide range of adults [31, 32], including chronically stressed persons [24], and has been successfully disseminated in California and other portions of the USA [33, 55], as well as through automated technologies [31]. As part of this body of evidence, the self-reported increases in physical activity captured via the PAR and CHAMPS have been extensively validated through the use of objective assessment procedures [24, 31, 32], although one limitation of the current study was not including objective physical activity assessments due to subject burden constraints. While we specifically chose a population with heightened stress complaints in light of challenges in finding suitable multiple behavior interventions for them, less stressed groups could respond differently to the interventions. It could also be interesting to explore how individual preferences could affect subsequent behavior change success with these types of multiple behavior regimens.
Our interventions were not aimed at weight loss and, as a result, did not produce significant mean weight loss across the study period. It is possible that, within the context of a weight loss program, other results might be obtained [6]. However, given the practice in many weight loss programs of targeting diet earlier and more intensively than physical activity, the diet-first arm results reported here may be particularly germane to such programs.
A 4-month time period was used to sequence the health behaviors based on prior studies indicating successful behavior change by 4 months [29, 30]. It is possible, however, that either shorter or longer initial time periods could improve the results of sequential interventions.
Finally, while the two health behavior areas were brought together temporally, health advisors did not explicitly seek out ways to more fully integrate the two behaviors in the discussions that occurred with participants. Such proactive methods are recommended.
In summary, the results suggest that, in the current population, delivering physical activity and dietary interventions simultaneously may result in the most positive sustained outcomes across these two health behaviors. In addition, the potential behavioral suppression effects of dietary intervention on physical activity change are noteworthy and deserve further evaluation.
References
Physical Activity Guidelines Advisory Committee. Report of the Physical Activity Guidelines Advisory Committee, 2008. Washington, DC: U.S. Dept. of Health & Human Services; 2008.
U.S. Department of Health and Human Services and U.S. Department of Agriculture. Dietary Guidelines for Americans, 2005. 6th ed. Washington, DC: U.S. Govt. Printing Office; 2005.
U.S. Department of Health & Human Services. Healthy People 2010, Final Review. Washington, DC: US Department of Health and Human Services, Office of Disease Prevention and Health Promotion; 2011.
Bandura A. Social cognitive theory: An agentic perspective. Ann Rev Psychol. 2001;52:1-26.
Kremers SPJ, de Bruijn GJ, Schaalma H, Brug J. Clustering of energy balance-related behaviours and their intrapersonal determinants. Psychol Health. 2004;19:595-606.
Mata J, Silva MN, Vieira PN, et al. Motivational “spill-over” during weight control: Increased self-determination and exercise intrinsic motivation predict eating self-regulation. Health Psychol. 2009;28:709-716.
Emmons KM, Marcus BH, et al. The relationship between smoking, physical activity, and dietary fat intake among manufacturing workers. Prev Med. 1994;23:481-489.
Wilcox S, King AC, Castro C, Bortz W II. Do changes in physical activity lead to dietary changes in middle and older age? Am J Prev Med. 2000;18:276-283.
Wansink B, Sobal J. Mindless eating: The 200 daily food decisions we overlook. Environ Behav. 2007;39:106-123.
King AC, Frey-Hewitt B, Dreon DM, Wood PD. Diet vs exercise in weight maintenance. The effects of minimal intervention strategies on long-term outcomes in men. Arch Intern Med. 1989;149:2741-2746.
Hagger MS, Wood C, Stiff C, Chatzisarantis NL. Ego depletion and the strength model of self-control: A meta-analysis. Psychol Bull. 2010;136:495-525.
Baumeister RF, Vohs KD, Tice DM. The strength model of self-control. Curr Dir Psychol Sci. 2007;16:351-355.
Kiernan M, King AC, Stefanick M, Kraemer HC. Characteristics of successful and unsuccessful dieters: An application of signal detection methodology. Ann Behav Med. 1998;20:1-6.
Kendzierski D. A self-schema approach to healthy eating. J Am Psychiatr Nurses Assoc. 2007;12:350-357.
Wood W, Neal DT. A new look at habits and the habit–goal interface. Psychol Rev. 2007;114:843-863.
Oman RF, King AC. The effect of life events and exercise program format on the adoption and maintenance of exercise behavior. Health Psychol. 2000;19:605-612.
Hypertension Prevention Trial Research Group. The Hypertension Prevention Trial: Three-year effects of dietary changes on blood pressure. Arch Intern Med. 1990;150:153-162.
Young DR, Vollmer WM, King AC, et al. Can individuals meet multiple physical activity and dietary behavior goals? Am J Health Behav. 2009;33:277-286.
Lluch A, King NA, Blundell JE. Exercise in dietary restrained women: No effect on energy intake but change in hedonic ratings. Eur J Clin Nutr. 1998;52:300-307.
Vandelanotte C, Bourdeaudhuij ID, Brug J. Two-year follow-up of sequential and simultaneous interactive computer-tailored interventions for increasing physical activity and decreasing fat intake. Ann Behav Med. 2007;33:213-219.
Hyman DJ, Pavlik VN, Taylor WC, Goodrick GK, Moye L. Simultaneous vs sequential counseling for multiple behavior change. Arch Intern Med. 2007;167:1152-1158.
Aspinwall LG, Taylor SE. A stitch in time: Self-regulation and proactive coping. Psychol Bull. 1997;121:417-436.
King AC, Kiernan M, Oman RF, et al. Can we identify who will adhere to long-term physical activity? Signal detection methodology as a potential aid to clinical decision making. Health Psychol. 1997;16:380-389.
King AC, Baumann K, O'Sullivan P, Wilcox S, Castro C. Effects of moderate-intensity exercise on physiological, behavioral, and emotional responses to family caregiving: A randomized controlled trial. J Gerontol: Med Sci. 2002;57A:M26-M36.
National Center for Health Statistics. National Health Interview Survey. Washington, DC: National Center for Health Statistics; 2002.
Block G, Gillespie C, Rosenbaum EH, Jenson C. A rapid food screener to assess fat and fruit and vegetable intake. Am J Prev Med. 2000;18:284-288.
Cohen S, Williamson G. Perceived stress in a probability sample of the United States. In: Spacapam S, Oskamp S, eds. The social psychology of health: Claremont Symposium on applied social psychology. Newbury Park: Sage; 1988:31-67.
Efron B. Forcing a sequential experiment to be balanced. Biometrika. 1971;58:403-417.
King AC, Oman RF, Brassington GS, Bliwise DL, Haskell WL. Moderate-intensity exercise and self-rated quality of sleep in older adults. A randomized controlled trial. JAMA. 1997;277:32-37.
Eakin EG, Lawler SP, Vandelanotte C, Owen N. Telephone interventions for physical activity and dietary behavior change: A systematic review. Am J Prev Med. 2007;32:419-434.
King AC, Friedman RM, Marcus BH, et al. Ongoing physical activity advice by humans versus computers: The Community Health Advice by Telephone (CHAT) Trial. Health Psychol. 2007;26:718-727.
Castro CM, Pruitt LA, Buman MP, King AC. Physical activity program delivery by professionals vs volunteers: The TEAM randomized trial. Health Psychol. 2011;30:285-294.
Wilcox S, Dowda M, Leviton LC, et al. Active for life: Final results from the translation of two physical activity programs. Am J Prev Med. 2008;35:340-351.
Marcus BH, Simkin LR. The transtheoretical model: Applications to exercise behavior. Med Sci Sports Exerc. 1994;26:1400-1404.
Bassett DR Jr, Ainsworth BE, Leggett SR, et al. Accuracy of five electronic pedometers for measuring distance walked. Med Sci Sports Exerc. 1996;28:1071-1077.
Pearson TA, Bazzarre TL, Daniels SR, et al. American Heart Association guide for improving cardiovascular health at the community level: A statement for public health practitioners, healthcare providers, and health policy makers from the American Heart Association Expert Panel on Population and Prevention Science. Circulation. 2003;107:645-651.
King AC, Winett RA. Tailoring stress-reduction strategies to populations at risk: Comparisons between women from dual-career and dual-working families. Fam Commun Health. 1986;9:42-50.
Luskin F, Pelletier K. Stress Free for Good: 10 Scientifically Proven Life Skills for Health and Happiness. New York: Harper Collins; 2005.
Fisher JD, Fisher WA. Changing AIDS-risk behavior. Psychol Bull. 1992;111:455-474.
Sallis JF, Haskell WL, Wood PD, et al. Physical activity assessment methodology in the five-city project. Am J Epidemiol. 1985;121:91-106.
Pruitt LA, King AC, Obarzanek E, et al. Reliability of the 7-day physical activity recall in a biracial group of inactive and active adults. J Phys Act Health. 2006;3:423-438.
Stewart AL, Mills KM, King AC, et al. CHAMPS physical activity questionnaire for older adults: Outcomes for interventions. Med Sci Sports Exerc. 2001;33:1126-1141.
Prochaska JJ, Velicer WF, Nigg CR, Prochaska JO. Methods of quantifying change in multiple risk factor interventions. Prev Med. 2008;46:260-265.
Block G, Thompson FE, Hartman AM, Larkin FA, Guire KE. Comparison of two dietary questionnaires validated against multiple dietary records collected during a 1-year period. J Am Diet Assoc. 1992;92:686-693.
Boucher B, Cotterchio M, Kreiger N, et al. Validity and reliability of the Block98 food-frequency questionnaire in a sample of Canadian women. Public Health Nutr. 2006;9:84-93.
Block G, Coyle LM, Hartman AM, Scoppa SM. Revision of dietary analysis software for the Health Habits and History Questionnaire. Am J Epidemiol. 1994;139:1190-1196.
Sallis JF, Grossman RM, Pinski RB, Patterson TL, Nader PR. The development of scales to measure social support for diet and exercise behaviors. Prev Med. 1987;16:825-836.
Garcia AW, King AC. Predicting long-term adherence to aerobic exercise: A comparison of two models. J Sport Exerc Psychol. 1991;13:394-410.
Wilcox S, Castro C, King AC. Outcome expectations and physical activity participation in caregiving and non-caregiving women. J Health Psychol. 2006;11:65-77.
Kraemer HC, Thiemann S. How many subjects? Statistical power analysis in research. Newbury Park: Sage; 1987.
Spector PC, Goodnight JH, Sall JP, Sarle WS. The GLM procedure. SAS user's guide: Statistics. Version 5. Cary: SAS Institute Inc; 1985:433-506.
Wood AM, White IR, Hillsdon M, Carpenter J. Comparison of imputation and modelling methods in the analysis of a physical activity trial with missing outcomes. Int J Epidemiol. 2005;34:89-99.
SAS Institute Inc. SAS/STAT 9.2 User's Guide. 2nd ed. Cary: SAS Institute; 2009.
Singer JD, Willett JB. Applied Longitudinal Data Analysis: Modeling Change and Event Occurrence. New York: Oxford University Press; 2003.
Hooker SP, Seavey W, Weidmer CE, et al. The California active aging community grant program: Translating science into practice to promote physical activity in older adults. Ann Behav Med. 2005;29:155-165.
Acknowledgments
The research was supported by a Public Health Service Grant R01AG021010 from the National Institute on Aging (King) and a Public Health Service Training Grant 5T32HL007034 from the National Heart, Lung, and Blood Institute. The authors thank Carolyn Prosak, Catharine Cassayre, Julia Wu, Arturo Fernandez, Susannah Belding, and Sarah French for implementing the interventions; Dr. Leslie Pruitt and Stephanie Koltiska for their work with respect to study evaluations; and Dr. Judith Prochaska for comments on the manuscript.
Conflict of Interest
The authors have no conflicts of interest to disclose.
Author information
Authors and Affiliations
Corresponding author
About this article
Cite this article
King, A.C., Castro, C.M., Buman, M.P. et al. Behavioral Impacts of Sequentially versus Simultaneously Delivered Dietary Plus Physical Activity Interventions: the CALM Trial. ann. behav. med. 46, 157–168 (2013). https://doi.org/10.1007/s12160-013-9501-y
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12160-013-9501-y