Abstract
Background
Physical activity (PA) is consistently linked to mental health outcomes.
Purpose
This meta-analysis synthesized depressive symptom outcomes of supervised and unsupervised PA interventions among healthy adults.
Methods
Comprehensive searching and coding were applied to PA interventions among adults without clinical depression. Analyses included random-effects standardized means, Q, and moderator analysis using analysis of variance and regression meta-analytic analogues.
Results
Treatment versus control comparisons yielded a standardized mean effect size of 0.372 among 38 supervised PA studies and 0.522 among 22 unsupervised PA studies. Preliminary moderator analyses suggested that supervised PA interventions may be more effective when they include flexibility/resistance and low-intensity exercise. Unsupervised PA interventions may be more effective when they recommend center-based PA. Methodological moderators (random assignment, control group management) were identified.
Conclusions
These findings document that PA interventions reduce depressive symptoms even in adults without clinical depression. Moderator analyses suggest directions for future research as well as practice.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Numerous studies link physical activity (PA) and mental health. Research examining the influence of exercise interventions on clinical depression has been published for more than a century [1]. The link between PA and clinical depression has been documented [2]. Narrative reviews and meta-analyses have examined the sizable empirical literature testing the effect of PA interventions on subjects with clinical depression [3–8]. Longitudinal descriptive research suggests that PA may be effective for preventing clinical depression [2, 9].
Some depressive symptoms are common among people without clinical depression. Depressive symptoms include cognitive-affective and somatic symptoms [3, 10–12]. Depressive symptoms may precede clinical depression, which is related to health state and physical disease [12]. Many PA intervention studies conducted with healthy adults have measured depressive symptom outcomes because these symptoms are an important component of mental health and quality of life [2, 3, 10]. The mechanism by which PA may reduce depressive symptoms is not well understood [3, 12]. Biochemical or physiological explanations include endogenous opiates, endocannabinoids, brain neurotransmitters, anti-inflammatory cytokines, cerebral blood flow, and hypothalamic–pituitary–adrenal axis function [3, 12]. Hypothesized psychological mechanisms include distraction and enhanced self-efficacy, self-esteem, behavioral activation, sense of achievement/mastery, and self-determination [2, 5, 12]. The relationship between PA and depressive symptoms may be reciprocal. People who experience reduced depressive symptoms may be more likely to continue PA performance. Given the potential importance of depressive symptoms in adults without clinical depression, this meta-analysis synthesized the body of work examining depressive symptom outcomes of PA interventions.
Previous meta-analyses of PA interventions for subjects without clinical depression have focused on older adults [10], included diverse measures of negative mood outcomes without specifically addressing depressive symptoms [10, 13], or included not only studies that targeted subjects with clinical depression but also studies of participants without clinical depression [8, 11, 13, 14]. Only one previous meta-analysis examined the impact of PA interventions on depressive symptoms among subjects without clinical depression [14]. North [14] synthesized depressive symptom outcomes of PA interventions from studies of subjects with and without clinical depression. North et al. reported a standardized mean difference of 0.59 for depressive symptom scores among studies focused on adults without clinical depression. North et al. conducted moderator analyses across studies including subjects with and without clinical depression. They reported larger effect sizes in published studies (vs. unpublished reports), those with home-based exercise (vs. center-based PA), studies with random assignment of subjects, studies with more males, studies with clinically depressed subjects (vs. subjects without clinical depression), studies with resistance PA (vs. endurance PA), and studies with 21- to 24-week interventions (vs. less than 21 weeks or more than 24 weeks) [14].
No previous meta-analyses have reported moderator analyses focused on studies of subjects without clinical depression. Moderator analyses are important to determine if depressive symptom outcomes are associated with characteristics of samples, research methods, or interventions. For example, moderator analyses can determine if intervention effects are similar among women and men or across sample ages. This quantitative synthesis moves beyond previous reviews by focusing on studies of adults without clinical depression, by greatly expanding primary study search strategies to achieve a comprehensive synthesis, and by conducting moderator analyses. This meta-analysis addressed the following research questions:
-
(1)
What are the overall effects of supervised PA and unsupervised PA interventions on depressive symptoms in healthy adults without clinical depression?
-
(2)
Do interventions’ effects on depressive symptom outcomes vary depending on intervention, sample, and research design characteristics?
-
(3)
What are the effects of interventions on depressive symptoms among studies comparing treatment subjects before versus after interventions?
Methods
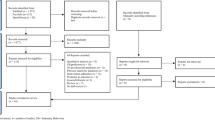
We used standard procedures for conducting meta-analysis research to identify and obtain potential primary study reports, determine eligibility, extract data from reports, conduct meta-analysis statistical procedures, and interpret findings [15]. The project received approval from the university institutional review board for the protection of human subjects.
Primary Study Search Strategies
Multiple search strategies were used to ensure a comprehensive search and thus limit bias while moving beyond previous reviews [16–18]. An expert reference librarian searched 11 computerized databases (e.g., MEDLINE, PsychINFO, EMBASE) using broad search terms (sample MEDLINE intervention terms: adherence, behavior therapy, clinical trial, compliance, counseling, evaluation, evaluation study, evidence-based medicine, health care evaluation, health behavior, health education, health promotion, intervention, outcome and process assessment, patient education, program, program development, program evaluation, self care, treatment outcome, validation study; PA terms: exercise, physical activity, physical fitness, exertion, exercise therapy, physical education and training, walking). Search terms for depressive symptoms were not used to narrow the search because many PA intervention studies report depressive symptom outcomes but do not consider these the main outcomes of the study and thus papers are not indexed by these terms. Several research registers were examined including Computer Retrieval of Information on Scientific Projects and mRCT, which contains 14 active registers and 16 archived registers. Computerized author searches were completed for project principal investigators located from research registers and for the first three authors on eligible studies. Author searches were completed for dissertation authors to locate published papers. Ancestry searches were conducted on eligible and review papers. Hand searches were completed for 114 journals which frequently report PA intervention research.
Selection Criteria
We included studies with an outcome measure of depressive symptoms following PA interventions. Two types of PA interventions were studied: researcher supervised PA such that PA performance was verified, and interventions designed to increase unsupervised PA where the PA performance was not verified. All analyses were conducted separately for supervised PA and unsupervised PA studies. Ancillary intervention strategies that might directly affect depressive symptoms were uncommon and these studies were excluded. For example, studies were excluded if they used relaxation exercise, stress management strategies, cognitive-behavior therapy, etc. These strategies were found in a few interventions designed to affect multiple health behaviors and outcomes. These psychological interventions were excluded because the project focused on the link between depressive symptoms and supervised or unsupervised PA. Supervised PA studies were included if they measured depressive symptoms 1 to 7 days after the last exercise session. Studies with immediate measurement of depressive symptoms following an acute bout of exercise were excluded. Acute bouts of exercise may influence mood when mood is measured in the minutes immediately following the exercise. This synthesis was focused on changes in depressive symptoms beyond immediate effects of exercise on depressive symptoms.
Studies with diverse measures of depressive symptoms were included. Primary studies using self-report measures of cognitive-affective and somatic depressive symptoms were included (e.g., Beck Depression Inventory, Profile of Mood States depressive symptoms subscale, and Center for Epidemiologic Studies-Depression Scale). Only studies that measured depressive symptoms separately from other symptoms were included. For example, we excluded studies reporting overall mood disturbance and those which combined measures of anxiety and depression (unless they reported depressive symptoms separately). Samples included healthy adults without acute or chronic physical or mental illness. Studies targeting subjects with clinical depression or subjects that scored above a primary study specified depressive symptom criterion score were excluded.
English language studies reported between 1969 and 2008 were included. Both published and unpublished studies were included because the single most consistent difference between published and unpublished research is the statistical significance of findings. Meta-analyses with only published primary studies may overestimate the magnitude of the true population effect [18]. We included small-sample studies with as few as five treatment group subjects, small-sample studies often lack statistical power to detect treatment effects but can contribute to meta-analysis findings. Studies were weighted so that those with larger samples had proportionally more impact on aggregate findings [19]. Pre-experimental and experimental studies were included. All analyses were conducted separately for two-group and single-group pre- and post-comparisons, with moderator analyses conducted exclusively on two-group comparisons because of validity concerns in single-group pre- and post-comparisons. We report the single-group findings only as ancillary information to the more valid two-group results.
Data Coding and Evaluation
A coding frame to extract primary study characteristics and outcomes was developed from previous meta-analyses on related topics, intervention components reported in empirical literature, and the research team’s previous meta-analyses. The coding frame was pilot tested with 20 studies prior to implementation. Year of dissemination, publication status (published articles/chapters vs. unpublished reports such as dissertations), and presence of funding were coded as report features. Gender, age, ethnicity, and subject weights were coded from descriptions of samples in primary studies. Methodological features that we coded included attrition rates, random vs. nonrandom assignment to treatment and control groups, and control group management (i.e., attention control vs. true control).
Supervised PA intervention characteristics were coded, including intervention dose (total minutes of supervised PA), exercise intensity, and whether the exercise included flexibility or resistance exercise as well as endurance exercise. For unsupervised PA interventions, the recommended PA intensity, form, and minutes per week were coded. Other coded intervention characteristics included whether the intervention was linked with worksites, whether it was delivered to individuals or groups, and whether it targeted only PA behavior or attempted to change multiple behaviors (e.g., PA plus diet). Outcome data coded included baseline and outcome sample sizes, means, measures of variability, change scores, and t statistics.
All data were independently coded by two extensively trained coders to enhance reliability. All outcome data were further verified by a doctorally prepared coder. Coding decisions not easily reconciled between coders were adjudicated by the principal investigator. All data were compared among coders until 100% agreement was achieved. Coded data were also duplicate-entered. To ensure independence among samples, we cross-checked author lists to identify reports that might contain overlapping samples. We contacted senior authors to clarify uniqueness of samples. Ancillary reports—additional publications about the same subjects—enhanced coding completion.
Data Analysis
We handled data calculations by standard meta-analytic approaches using standardized mean differences (d) effect size (ES) weighted by the inverse of variance to give larger samples more influence [20]. ESs were adjusted for bias. Random-effects models were used to acknowledge that individual ESs vary due both to subject-level sampling error and to other sources of study-level error such as variations among interventions [21]. Normal-theory standard errors were used to construct 95% confidence intervals. Between-study homogeneity was assessed with a conventional homogeneity statistic (Q)[20]. Statistical and clinical heterogeneity is common in behavior change research [22, 23]. We expected heterogeneity in this sample and handled it in four ways [22, 23]. First, random-effects analyses were used because they take into account heterogeneity not fully explained by moderators. Second, a location parameter was calculated along with quantification of heterogeneity. Third, potential heterogeneity was explored with moderator analyses. Fourth, findings were interpreted in the context of discovered heterogeneity. We explored potential publication bias by constructing funnel plots of ES against sampling variance where symmetrical distribution of ES suggested absence of bias [24].
Whenever baseline data were available, treatment group pre- and post-scores were compared. These calculations require correlations between baseline and outcome scores that are not reported in primary studies [25]. These analyses were conducted under two assumptions: no correlation and high (0.80) correlation. Single-group comparisons were not combined with two-group comparisons, nor were moderator analyses conducted on single-group data. All analyses were conducted separately for supervised and unsupervised PA.
We conducted exploratory moderator analyses to determine if ESs were associated with primary study characteristics. Continuous moderators were examined by testing effects through an unstandardized regression slope, a meta-analytic analogue of regression [20]. Dichotomous moderators were examined through testing effects by between-group heterogeneity statistic (Q between), a meta-analytic analogue of analysis of variance [20].
Results
Comprehensive searches yielded 70 reports with 38 eligible supervised PA treatment vs. control comparisons, 22 eligible unsupervised PA treatment vs. control comparisons, 67 supervised PA treatment group pre- vs. post-intervention comparisons, 45 unsupervised PA treatment group pre- vs. post-intervention comparisons, 29 supervised PA control group pre- vs. post-intervention comparisons, and nine unsupervised PA control group pre- vs. post-intervention comparisons [26–95]. The supervised PA two-group comparisons included 1,598 subjects. The unsupervised PA two-group comparisons included 1,081 subjects. The treatment single-group comparisons included 1,639 supervised PA and 3,420 unsupervised PA subjects. The pre- and post-comparisons included 676 control subjects in supervised PA studies and 198 control participants in unsupervised PA studies. Most primary studies were published articles (s = 54), and the remainder were dissertations (s = 14), book chapter (s = 1), and conference presentation materials (s = 1; s indicates the number of reports). Publication bias was evident in the funnel plots for supervised PA and unsupervised PA two-group outcome comparisons and for treatment group, pre- vs. post-intervention supervised PA and unsupervised PA comparisons. The control group pre- and post-comparison distributions on the funnel plots suggested less publication bias than plots of treatment groups. Unless otherwise specified, all results are from the treatment vs. control comparisons.
Attrition ranged from 0% to 54%. Interventions designed to increase unsupervised PA ranged from 1 day in length to 1 year between starting and completing the intervention. Supervised PA interventions typically lasted 45 to 60 min, with thrice weekly meetings, and a mean of 62 sessions (range 8 to 156 sessions). Unsupervised PA studies typically recommended 30 to 60 min of PA thrice weekly. Many unsupervised PA studies measured depressive symptoms within a week after PA interventions were completed. Among studies measuring outcomes later, the number of days between the intervention and outcome assessment ranged from 30 to 1,825 days. The most commonly used measures of depressive symptoms were the Profile of Mood States, Beck Depression Inventory, and Center for Epidemiologic Studies-Depression Scale. Studies averaged 65% female subjects. The mean age across samples ranged from 31 to 81 years, with a mean of 48.5 years. The mean weight was 75.9 kg, with a range from 62 to 90 kg. Body mass index means ranged from 25 to 31, with a mean of 27.6.
Effects of Interventions
Table 1 shows the effects of interventions on depressive symptom outcomes. We found a mean ES of 0.372 among the 38 supervised PA studies comparing treatment and control groups following interventions. Supervised PA treatment group pre- vs. post-intervention comparisons yielded mean ESs of 0.258 and 0.281 under the assumptions of high correlation and no correlation, respectively. ESs for two-group and treatment group pre- and post-comparisons of supervised PA were statistically significant with the confidence interval not including 0. For unsupervised PA interventions, the two-group comparison yielded an ES of 0.522. Treatment group pre- vs. post-intervention comparisons of unsupervised PA yielded mean ESs of 0.474 and 0.519 under the assumptions of high correlation and no correlation, respectively. All two-group and treatment pre- vs. post-intervention comparisons for supervised and unsupervised PA were significantly heterogeneous (Q in Table 1). Control group pre- vs. post-intervention comparisons for both supervised and unsupervised PA were much smaller, with all confidence intervals including 0.
Moderator Findings
We report moderator analyses for two-group comparisons for both supervised and unsupervised PA (Table 2: continuous moderators, Table 3: dichotomous moderators) when adequate data were reported in primary studies. Results of some potential moderator analyses (e.g., study focused on overweight subjects, worksite interventions) should be interpreted cautiously given small-sample sizes for these variables.
Report Moderators
Year of publication was unrelated to ES for supervised PA studies. Unsupervised PA studies published more recently had slightly smaller ESs than studies published earlier (Table 2). The magnitude was small, although statistically significant. For both supervised and unsupervised PA, unpublished studies reported larger ES (0.564, 0.870) than published studies (0.321, 0.432; Table 3). Although more distinct in unsupervised PA studies, a similar trend was apparent for unfunded studies having larger ES than funded studies for supervised PA (0.506 vs. 0.313) and unsupervised PA (1.090 vs. 0.192) studies.
Research Methods Moderators
Unsupervised PA studies with random assignment of subjects to treatment and control conditions reported smaller ES (0.201) than studies without random assignment (0.932). A similar trend among supervised PA studies (0.334 vs. 0.514) did not achieve statistical significance. The difference between unsupervised PA studies with true control groups (0.596) and studies with attention control groups (0.191) was borderline statistically significant. Neither sample size nor attrition rates were related to depressive symptom outcome ESs.
Primary Study Sample Characteristic Moderators
Unsupervised PA studies with more women reported slightly smaller depressive symptom ES (Table 2). Sample age was unrelated to outcomes for supervised PA studies. Gender was not a significant predictor of ESs. Primary study mean sample weight and whether studies focused on overweight subjects were both unrelated to depressive symptom outcomes in supervised PA studies (Tables 2 and 3). Inadequate primary study report information prevented a similar analysis for unsupervised PA studies.
Intervention Characteristic Moderators
Interventions that targeted only PA behavior were not significantly more effective than interventions attempting to change multiple behaviors (Table 3). The social setting of the intervention (group vs. individual) was not a statistically significant moderator of ES. Worksite-based unsupervised PA interventions reported similar ESs (0.512) compared to interventions not linked with workplaces (0.529).
The number of days over which the intervention to increase unsupervised PA was delivered was a statistically significant predictor, but the ES magnitude was very small. The relationship between the ES and the magnitude of the dose of supervised PA (minutes per session times the number of sessions) was small and not statistically significant. Low intensity supervised PA interventions resulted in a significantly larger ES (0.907) than moderate intensity interventions (0.271). The pattern of findings for three analyses addressing the exercise form (endurance, resistance, flexibility) suggested interventions are most effective when the intervention is not exclusively focused on endurance exercise (Table 3). The addition of either flexibility or resistance exercise improves depressive symptom outcomes.
Among unsupervised PA studies, neither the recommended PA intensity nor the recommended form of PA were related to outcome ES. Although only three of the unsupervised PA studies recommended subjects exercise at a fitness center, these studies reported significantly larger ES (0.922) than studies which recommended home exercise (0.425). Unsupervised PA interventions that recommended more minutes per week of PA reported smaller ES. Shorter unsupervised PA interventions (days over which the intervention was delivered) resulted in larger ES outcomes. The magnitude of the effects for both recommended minutes and intervention days were quite small.
Discussion
This research synthesis documented that both supervised and unsupervised PA interventions significantly improve depressive symptoms among healthy adults. The moderate ESs (0.372 and 0.522) are between the ES reported for negative affect among older adults (0.35) [10] and the 0.59 ES for non-depressed subjects reported in 1990 [14]. Meta-analyses of PA interventions delivered to adults with clinical depression have reported larger ESs of 0.72 [6], 1.10 [5], and 1.42 [7]. The smaller effects among subjects without clinical depression may partially reflect a floor effect where healthy subjects have less room to improve depressive symptoms than subjects with clinical depression [8]. The moderate ESs document that even subjects who are not clinically depressed experience improvement in depressive symptoms following either supervised or unsupervised PA interventions. Unfortunately, none of the studies reported subsequent episodes of clinical depression to determine the extent to which the interventions reduced clinical depression episodes such as Major Depressive Disorder, Dysthymic Disorder, or Depressive Disorder Not Specified [5, 96–98]. Longer follow-up would be necessary to determine the protective benefit of PA interventions.
As expected, the primary studies were heterogeneous. The exploratory moderator analyses of report, methods, and intervention characteristic may help explain existing heterogeneity. The findings indicated a tendency for unpublished and unfunded studies to report larger ESs than published and funded studies. Unpublished dissertation research may contain studies with heightened investigator involvement in especially strong interventions. Unfunded studies may include pilot projects where investigators are strongly vested in providing exceptional interventions to ensure subsequent funding of larger projects. Moderator analyses suggest cautious interpretation of research with some design characteristics. Studies without random assignment or without attention control groups may overestimate the benefits of PA interventions [5].
Encouraging findings, consistent with previous research with clinically depressed subjects [14], suggest that both supervised and unsupervised PA interventions may be broadly beneficial across age groups and weight distributions. Both men and women seem to experience positive results from PA interventions. Interventions delivered to groups are as effective as those focused on individuals, which is important for delivering interventions in a cost-effective manner.
Previous research has documented that interventions that target only PA behavior (vs. those attempting to change multiple behaviors) are more effective in increasing the amount of PA after interventions [23, 99]. These depressive symptom findings suggest that interventions targeting multiple health behaviors may be as effective as interventions focused only on PA behavior. The pattern of findings in this project, including the larger ES for unsupervised than supervised PA interventions, suggests changes in depressive symptoms are affected by something beyond actual PA behavior. Complex inter-related factors likely affect depressive symptoms.
The findings that supervised low-intensity interventions were more effective than moderate or high intensity interventions is consistent with a previous meta-analysis examining overall mood outcomes [10]. These findings do not support the common contention that insufficient training intensity is the reason for poor outcomes in some studies [10, 97]. It is possible that subjects were so unfit that low intensity PA was more achievable than more intense exercise [10]. Low intensity PA may elicit immediate positive feelings that may not be as apparent in more vigorous exercise [97]. Although most research has emphasized endurance type exercise, these novel findings suggest that including flexibility and resistance exercise may be important for improving depressive symptoms. Lawlor and Hopker [5] found no difference between endurance and resistance exercise in major depression symptoms. A meta-analysis of PA interventions among older adults reported lower ES among studies with endurance exercise than studies with resistance exercise [10]. Neither previous published meta-analysis included any primary studies with flexibility exercise. Our findings regarding exercise intensity and achieved exercise dose in supervised PA studies suggest that improved aerobic fitness may not be the mechanism by which depressive symptoms improve [11, 12, 98]. Although endurance exercise has cardiovascular benefits, our findings suggest that additional forms of exercise may have significant depressive symptom benefits. Studies that systematically manipulate dimensions of the exercise stimulus are needed. Center-based PA may offer advantages beyond PA itself that account for these studies’ larger improvements in depressive symptoms. Exercise centers may offer structured experiences, social interaction, and positive regard from others that may enhance the depressive symptom benefits of the PA.
This meta-analysis was limited by the primary studies and by inherent meta-analysis method limitations. Some potentially important moderators were inadequately reported for analyses. For example, few studies reported sample ethnicity. Challenges in designing adequate placebo/attention control groups for testing interventions on psychosocial outcomes are obvious in many primary reports. Studies comparing PA modes and intensities are infrequently reported. Moderator analyses must be interpreted cautiously given the observational nature of meta-analysis and the potential for confounding unknown variables. This synthesis focused on depressive symptoms among samples without clinical depression. A broader meta-analysis comparing interventions among subjects with and without clinical depression would be informative. This project excluded studies that used both PA interventions and psychological treatments. Meta-analyses of these studies would be useful to determine potential additive effects of both intervention types.
In conclusion, these meta-analysis findings document that both supervised and unsupervised PA interventions are effective in reducing depressive symptoms among adults without clinical depression. Subjects benefitting from the interventions included those of both genders and of diverse weights. Intriguing moderator analyses suggest that further examination is in order regarding the influence of the PA stimulus (e.g., flexibility vs. resistance vs. endurance PA) on depressive symptom outcomes.
References
Franz SL, Hamilton GV. Effect of exercise upon the retardation in condition of depression. Am J Insanity. 1905; 62: 239–256.
Martinsen EW. Physical activity in the prevention and treatment of anxiety and depression. Nord J Psychiatry. 2008; 62(Suppl 47): 25–29.
Deslandes A, Moraes H, Ferreira C, et al. Exercise and mental health: Many reasons to move. Neuropsychobiology. 2009; 59: 191–198.
Dunn AL, Trivedi MH, O'Neal HA. Physical activity dose-response effects on outcomes of depression and anxiety. Med Sci Sports Exerc. 2001; 33: S587–S597; S609–S510.
Lawlor DA, Hopker SW. The effectiveness of exercise as an intervention in the management of depression: Systematic review and meta-regression of randomised controlled trials. BMJ. 2001; 322: 763–767.
Craft LL, Landers DM. The effects of exercise on clinical depression and depression resulting from mental illness: A meta-regression. J Sport Exerc Psychol. 1998; 20: 339–347.
Stathopoulou G, Powers MB, Berry AC, Smits JAJ, Otto MW. Exercise interventions for mental health: A quantitative and qualitative review. Clin Psychol Sci Pract. 2006; 13: 179–193.
Pinquart M, Duberstein PR, Lyness JM. Effects of psychotherapy and other behavioral interventions on clinically depressed older adults: A meta-analysis. Aging Ment Health. 2007; 11: 645–657.
aan het Rot M, Collins KA, Fitterling HL. Physical exercise and depression. Mt Sinai J Med. 2009; 76: 204–214.
Arent S, Landers DM, Etnier J. The effects of exercise on mood in older adults: A meta-analytic review. J Aging Phys Act. 2000; 8: 407–430.
Sjosten N, Kivela SL. The effects of physical exercise on depressive symptoms among the aged: A systematic review. Int J Geriatr Psychiatry. 2006; 21: 410–418.
Daley A, Daley A. Exercise and depression: A review of reviews. J Clin Psychol Med Settings. 2008; 15: 140–147.
Penedo FJ, Dahn JR. Exercise and well-being: A review of mental and physical health benefits associated with physical activity. Curr Opin Psychiatry. 2005; 18: 189–193.
North TC, McCullagh P, Tran ZV. Effect of exercise on depression. Exerc Sport Sci Rev. 1990; 18: 379–415.
Cooper H, Hedges L, Valentine J, eds. The Handbook of Research Synthesis and Meta-Analysis. 2nd ed. New York: Russell Sage; 2009.
White H. Scientific communication and literature retrieval. In: Cooper H, Hedges L, Valentine J, eds. The Handbook of Research Synthesis and Meta-Analysis. 2nd ed. New York: Russell Sage; 2009: 51–71.
Reed J, Baxter P. Using reference databases. In: Cooper H, Hedges L, Valentine J, eds. The Handbook of Research Synthesis and Meta-Analysis. 2nd ed. New York: Russell Sage; 2009: 73–101.
Rothstein HR, Hopewell S. Grey literature. In: Cooper H, Hedges L, Valentine J, eds. The Handbook of Research Synthesis and Meta-Analysis. 2nd ed. New York: Russell Sage; 2009: 103–125.
Shadish W, Haddock C. Combining estimates of effect size. In: Cooper H, Hedges L, Valentine J, eds. The Handbook of Research Synthesis and Meta-Analysis. 2nd ed. New York: Russell Sage; 2009: 257–277.
Borenstein M, Hedges L, Higgins JP, Rothstein HR. Introduction to Meta-Analysis. UK: Wiley; 2009.
Raudenbush SW. Analyzing effect sizes: Random-effect models. In: Cooper H, Hedges L, Valentine J, eds. The Handbook of Research Synthesis and Meta-Analysis. 2nd ed. New York: Russell Sage; 2009: 295–316.
Wood W, Eagly A. Advantages of certainty and uncertainty. In: Cooper H, Hedges L, Valentine J, eds. The Handbook of Research Synthesis and Meta-Analysis. 2nd ed. New York: Russell Sage; 2009: 455–472.
Conn VS, Hafdahl AR, Brown SA, et al. Meta-analysis of patient education interventions to increase physical activity among chronically ill adults. Patient Educ Couns. 2008; 70: 157–172.
Sutton AJ. Publication bias. In: Cooper H, Hedges L, Valentine J, eds. The Handbook of Research Synthesis and Meta-Analysis. 2nd ed. New York: Russell Sage; 2009: 435–452.
Borenstein M. Effect sizes of continuous data. In: Cooper H, Hedges L, Valentine J, eds. The Handbook of Research Synthesis and Meta-Analysis. 2nd ed. New York: Russell Sage; 2009: 221–235.
*Andersen RE, Wadden TA, Bartlett SJ, et al. Effects of lifestyle activity vs. structured aerobic exercise in obese women: A randomized trial. JAMA. 1999; 281: 335–340.
*Annesi JJ, Westcott WL. Age as a moderator of relations of physical self-concept and mood changes associated with 10 weeks of programmed exercise in women. Percept Mot Skills. 2005; 101: 840–844.
*Annesi JJ, Westcott WW, Gann S. Preliminary evaluation of a 10-wk. resistance and cardiovascular exercise protocol on physiological and psychological measures for a sample of older women. Percept Mot Skills. 2004; 98: 163–170.
*Annesi JJ. Sex differences in relations of cardiorespiratory and mood changes associated with self-selected amounts of cardiovascular exercise. Psychol Rep. 2003; 93: 1339–1346.
*Anshel MH. Effect of chronic aerobic exercise and progressive relaxation on motor performance and affect following acute stress. Behav Med. 1996; 21: 186–196.
*Atlantis E, Chow CM, Kirby A, Singh MF. An effective exercise-based intervention for improving mental health and quality of life measures: A randomized controlled trial. Prev Med. 2004; 39: 424–434.
*Bacon L, Keim NL, Van Loan MD, et al. Evaluating a 'non-diet' wellness intervention for improvement of metabolic fitness, psychological well-being and eating and activity behaviors. Int J Obes Relat Metab Disord. 2002; 26: 854–865.
*Blair SN, Smith M, Collingwood TR, et al. Health promotion for educators: Impact on absenteeism. Prev Med. 1986; 15: 166–175.
*Blumenthal JA, Emery CF, Madden DJ, et al. Long-term effects of exercise on psychological functioning in older men and women. J Gerontol. 1991; 46: P352–P361.
*Boileau RA, McAuley E, Demetriou D, et al. Aerobic exercise training and cardiorespiratory fitness in older adults: A randomized trial. J Aging Phys Act. 1999; 7: 374–385.
*Brown D, Wang Y, Ward A, et al. Chronic psychological effects of exercise and exercise plus cognitive strategies. Med Sci Sports Exerc. 1995; 27: 765–775.
*Brown RS, Ramirez DE, Taub JM. The prescription of exercise for depression. Phys Sportsmed. 1978; 6: 34–49.
*Byrom JM. The Effects of a Cardiovascular Fitness Program on Depression, Anxiety, Self-Concept, and Perceived Physical Fitness in College Women [dissertation]. California School of Professional Psychology; 1983.
*Casal DC. Effects of 2000 Kilocalories Per Week of Treadmill Walking and Stairclimbing on Physical Fitness and Coronary Risk Factors of Obese Young Men [dissertation]. University of Minnesota; 1984.
*Cormier A, Prefontaine M, MacDonald H, Stuart RB. Lifestyle change on the campus: pilot test of a program to improve student health practices. In: Davidson PO, Davidson SM, eds. Behavioral Medicine: Changing Health Lifestyles. New York: Brunner/Mazel; 1980: 222–255.
*Craft L, Freund KM, Culpepper L, Perna FM. Intervention study of exercise for depressive symptoms in women. J Womens Health. 2007; 16: 1499–1509.
*Cramer SR, Nieman DC, Lee JW. The effects of moderate exercise training on psychological well-being and mood state in women. J Psychosom Res. 1991; 35: 437–449.
*Dennis KD, Pane, KW, Adams BK, Qi BB. The impact of a shipboard weight control program. Obes Res. 1999; 7: 60–67.
*DiLorenzo TM, Bargman EP, Stucky-Ropp R, et al. Long-term effects of aerobic exercise on psychological outcomes. Prev Med. 1999; 28: 75–85.
*Dunai A, Novak M, Chung SA, et al. Moderate exercise and bright light treatment in overweight and obese individuals. Obes Res. 2007; 15: 1749–1757.
*Eby JM. An investigation into the effects of aerobic exercise on anxiety and depression [dissertation]. University of Toronto; 1984.
*Elavsky S, McAuley E. Physical activity and mental health outcomes during menopause: A randomized controlled trial. Ann Behav Med. 2007; 33: 132–142.
*Elliot DL, Goldberg L, Duncan TE, et al. The PHLAME firefighters' study: Feasibility and findings. Am J Health Behav. 2004; 28: 13–23.
*Emery CF, Blumenthal JA. Effects of exercise training on psychological functioning in healthy type A men. Psychol Health. 1988; 2: 367–379.
*Emery CF, Gatz M. Psychological and cognitive effects of an exercise program for community-residing older adults. Gerontologist. 1990; 30: 184–188.
*Engels HJ, Drouin J, Zhu W, Kazmierski JF. Effects of low-impact, moderate-intensity exercise training with and without wrist weights on functional capacities and mood states in older adults. Gerontology. 1998; 44: 239–244.
*Galletly C, Clark A, Tomlinson L, Blaney F. A group program for obese, infertile women: Weight loss and improved psychological health. J Psychosom Obstet Gynaecol. 1996; 17: 125–128.
*Glisky ML: Interventions for Cognitive and Psychosocial Functioning in Older Adults: a Comparison of Aerobic Exercise and Cognitive Training [dissertation]. University of Arizona; 1997.
*Guest RS, Klose KJ, Needham-Shropshire BM, Jacobs PL. Evaluation of a training program for persons with SCI paraplegia using the Parastep 1 ambulation system: Effect on physical self-concept and depression. Arch Phys Med Rehabil. 1997; 78: 804–807.
*Gusi N, Reyes MC, Gonzalez-Guerrero JL, Herrera E, Garcia JM. Cost-utility of a walking programme for moderately depressed, obese, or overweight elderly women in primary care: a randomised controlled trial. BMC Public Health [serial online]. 2008; 8: 231. Available from http://www.biomedcentral.com/1471-2458/8/231. Accessed December 9, 2009.
*Harralson TL, Emig JC, Polansky M, et al. Un Corazon Saludable: Factors influencing outcomes of an exercise program designed to impact cardiac and metabolic risks among urban Latinas. J Community Health. 2007; 32: 401–412.
*Hassmen P, Koivula N. Mood, physical working capacity and cognitive performance in the elderly as related to physical activity. Aging Clin Exp Res. 1997; 9: 136–142.
*Hayward LM, Sullivan AC, Libonati JR. Group exercise reduces depression in obese women without weight loss. Percept Mot Skills. 2000; 90: 204–208.
*Hicks AL, Martin KA, Ditor DS, et al. Long-term exercise training in persons with spinal cord injury: effects on strength, arm ergometry performance and psychological well-being. Spinal Cord. 2003; 41: 34–43.
*Holder JD. The Effects of Low Level Aerobic Activity Upon Systolic Blood Pressure Heart Rate and Depression Levels among the Elderly [dissertation]. Boston University School of Education; 1982.
*Hunter M, O'Dea I. An evaluation of a health education intervention for mid-aged women: five year follow-up effects upon knowledge, impact of menopause and health. Patient Educ Couns. 1999; 38: 249–255.
*King AC, Baumann K, O'Sullivan P, Wilcox S, Castro C. Effects of moderate-intensity exercise on physiological, behavioral, and emotional responses to family caregiving: A randomized controlled trial. J Gerontol. 2002; 57: M26-M36.
*King AC, Brassington G. Enhancing physical and psychological functioning in older family caregivers: The role of regular physical activity. Ann Behav Med. 1997; 19: 91–100.
*King AC, Taylor CB, Haskell WL. Effects of differing intensities and formats of 12 months of exercise training on psychological outcomes in older adults. Health Psychol. 1993; 12: 292–300.
*Klein MH, Greist JH, Gurman AS, et al. A comparative outcome study of group psychotherapy vs. exercise treatments for depression. Int J Ment Health. 1985; 13: 148–177.
*Knittle VR. Effect of Twelve Weeks of Exercise on Depression, Self-Esteem, and Locus-of-Control in a Wellness Program Sample of Women Aged 65 and Older [thesis]. The University of Arizona; 1988.
*Kohut ML, McCann DA, Russell DW, et al. Aerobic exercise, but not flexibility/resistance exercise, reduces serum IL-18, CRP, and IL-6 independent of beta-blockers, BMI, and psychosocial factors. Brain Behav Immun. 2006; 20: 201–209.
*Lane A, Mills M, Terry P. Mood regulation among corporate workers: Effects of exercise on mood. J Sports Sci. 1998; 16: 87.
*Lennox SS. The Effect of Aerobic Exercise on Self-Reported Mood [dissertation]. State University of New York at Stony Brook; 1987.
*McDonald DG, Norton JP, Hodgdon JA. Training success in U.S. Navy special forces. Aviat Space Environ Med. 1990; 61: 548–554.
*McSherry WC, II. Effects of Aerobic Fitness Training on Migraine Headache [dissertation]. University of North Dakota; 1993.
*Melanson KJ, Dell'Olio J, Carpenter MR, Angelopoulos TJ. Changes in multiple health outcomes at 12 and 24 weeks resulting from 12 weeks of exercise counseling with or without dietary counseling in obese adults. Nutrition. 2004; 20: 849–856.
*Mellin L, Croughan-Minihane M, Dickey L. The Solution Method: 2-year trends in weight, blood pressure, exercise, depression, and functioning of adults trained in development skills. J Am Diet Assoc. 1997; 97: 1133–1138.
*Morgan WP, Costill DL, Flynn MG, Raglin JS, O'Connor PJ. Mood disturbance following increased training in swimmers. Med Sci Sports Exerc. 1988; 20: 408–414.
*Morgan WP, Roberts JA, Brand FR, Feinerman AD. Psychological effect of chronic physical activity. Med Sci Sports Exerc. 1970; 2: 213–217.
*Nagy S, Frazier S. The impact of exercise on locus of control, self-esteem, and mood states. J Soc Behav Pers. 1988; 3: 263–268.
*Nieman D, Warren B, Dotson R, Butterworth D, Henson D. Physical activity, psychological well-being, and mood state in elderly. J Aging Phys Act. 1993; 1: 22–33.
*Palmer LK. Effects of a walking program on attributional style, depression, and self-esteem. Percept Mot Skills. 1995; 81: 891–898.
*Pensabene T. Impact of a Walking Intervention on Perimenopausal Symptoms (Menopause) [dissertation]. Texas Women’s University; 1997.
*Perri S, II, Templer DI. The effects of an aerobic exercise program on psychological variables in older adults. Int J Aging Hum Dev. 1985; 20: 167–172.
*Rapoport L, Clark M, Wardle J. Evaluation of a modified cognitive-behavioural programme for weight management. Int J Obes Relat Metab Disord. 2000; 24: 1726–1737.
*Rhodes DL. Mens Sana, Corpore Sano: A Study of the Effect of Jogging on Depression, Anxiety and Self Concept [dissertation]. Duke University; 1980.
*Roth DL, Holmes DS. Influence of aerobic exercise training and relaxation training on physical and psychologic health following stressful life events. Psychosom Med. 1987; 49: 355–365.
*Simons CW, Birkimer JC. An exploration of factors predicting the effects of aerobic conditioning on mood state. J Psychosom Res. 1988; 32: 63–75.
*Sinatra S, Allen G, Camaione D, Abraham A. Effects of continuous passive motion, walking, and a placebo intervention on physical and psychological well-being. J Cardiopulm Rehabil. 1990; 10: 279–286.
*Sorensen M, Anderssen S, Hjerman I, Holme I, Ursin H. The effect of exercise and diet on mental health and quality of life in middle-aged individuals with elevated risk factors for cardiovascular disease. J Sports Sci. 1999; 17: 369–377.
*Stevenson DB. A Comparison of Group and Individual Physical Training Programs and Their Effect on Mood [dissertation]. The American University; 1990.
*Swoap RA, Norvell N, Graves JE, Pollock ML. High versus moderate intensity aerobic exercise in elderly: Psychological and physiological effects. J Aging Phys Act. 1994; 2: 293–303.
*Teixeira PJ. Weight Reduction in Middle-Aged Women: Readiness Profiles and Correlates of Success in a Lifestyle Intervention [dissertation]. The University of Arizona; 2001.
*Wadden TA, Stunkard AJ: Controlled trial of very low calorie diet, behavior therapy, and their combination in the treatment of obesity. J Consult Clin Psychol. 1996; 54: 482–488.
*Wallace JI, Buchner DM, Grothaus L, et al. Implementation and effectiveness of a community-based health promotion program for older adults. J Gerontol. 1998; 53A: M301-M306.
*Weaver DC. A Study to Determine the Effect of Exercise on Depression in Middle-Aged Women [dissertation]. Middle Tennessee State University; 1984.
*Wilson LFM. The Effects of an Exercise Conditioning Program on Reducing the Stress Response in Nurses [dissertation]. Wayne State University; 1985.
*Young RJ. The effect of regular exercise on cognitive functioning and personality. Br J Sports Med. 1979; 13: 110–117.
*Zigun SM. Multimodal Approach to Treatment of Obesity [dissertation]. The Union Institute; 1989.
Paluska SA, Schwenk TL. Physical activity and mental health: Current concepts. Sports Med. 2000; 29: 167–180.
Teychenne M, Ball K, Salmon J. Physical activity and likelihood of depression in adults: A review. Prev Med. 2008; 46: 397–411.
Ernst C, Olson AK, Pinel JP, Lam RW, Christie BR. Antidepressant effects of exercise: Evidence for an adult-neurogenesis hypothesis? J Psychiatry Neurosci. 2006; 31: 84–92.
Conn VS, Valentine JC, Cooper HM. Interventions to increase physical activity among aging adults: A meta-analysis. Ann Behav Med. 2002; 24: 190–200.
Acknowledgement
Financial support provided by a grant from the National Institutes of Health (R01NR009656) to Vicki Conn, principal investigator. The content is solely the responsibility of the author and does not necessarily represent the official views of the National Institutes of Health.
Conflict of interest
The author declares no conflicts of interest. The author has no financial relationship with the funding agency (NIH). The author has full control of all primary data and agrees to allow the journal to review the data.
Author information
Authors and Affiliations
Corresponding author
Additional information
Primary studies included in the meta-analysis marked with asterisk.
About this article
Cite this article
Conn, V.S. Depressive Symptom Outcomes of Physical Activity Interventions: Meta-analysis Findings. ann. behav. med. 39, 128–138 (2010). https://doi.org/10.1007/s12160-010-9172-x
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12160-010-9172-x