Abstract
Background
Detailed information about the characteristics of smokers who do and do not participate in smoking cessation treatment is needed to improve efforts to reach, motivate, and treat smokers.
Purpose
The aim of this study is to explore a broad range of characteristics related to participation in a smoking cessation trial.
Methods
Eligible smokers were recruited from a longitudinal birth cohort. Participants and non-participants were compared on a broad range of sociodemographics, smoking, psychiatric and substance abuse disorders, personality, and prospective measures from early childhood. Eligible smokers were compared to a matched regional subsample of the Behavioral Risk Factor Surveillance System (BRFSS).
Results
Few differences were observed, most of which were statistically significant but not clinically meaningful. Compared to non-participants, participants were more likely to be single, have lower income, be more nicotine-dependent, be more motivated to quit, and have higher levels of depressed mood and stress even after covariance of gender, income, and marital status. Sociodemographic differences between participants and the BRFSS sample reflect the skew toward lower socioeconomic status in the original birth cohort.
Conclusions
The encouraging conclusion is that smokers who enroll in cessation trials may not differ much from non-participants. Information about treatment participants can inform the development of recruitment strategies, improve the tailoring of treatment to individual smoker profiles, help to estimate potential selection bias, and improve estimates of population impact.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
The population impact of smoking cessation programs depends on the long-term effectiveness of interventions as well as the number of people who participate in them (impact = efficacy × reach) [1]. Although cessation treatments roughly double quit rates, less than half of current smokers try to quit each year [2], and the vast majority of those who try to quit do not use an evidence-based treatment method [3, 4]. Moreover, it has been estimated that only 2% of smokers participate in population-based smoking cessation research studies [5]. Relatively little is known about the characteristics of the vast majority of smokers who do not attempt to quit, do not use evidence-based treatment, or do not participate in treatment research. Information about factors related to treatment participation is needed to improve efforts to reach, motivate, and treat smokers, and ultimately, to improve the population impact of smoking cessation programs.
A growing number of studies have examined factors related to participation in cessation programs [3, 6–16]. Most of these studies focused primarily on sociodemographic factors (e.g., age, gender, race, education, income) and smoking behaviors (e.g., motivation for cessation, smoking rate, past-year quit attempts, age of smoking onset). In general, compared to non-participants, study participants are often more educated, older, higher income earners, Caucasian, employed, more addicted and heavier smokers, more motivated to quit, with a higher number of previous quit attempts. Few studies have examined a broader range of relevant smoking, psychosocial, psychiatric, or medical co-morbid factors in relation to treatment participation. Brod and Hall [17] found that non-participants were more anxious than participants but did not differ on health locus of control or other substance use. Ahluwahlia and colleagues [18] examined predictors of cessation treatment participation among African Americans who consented and enrolled in a cessation trial but did not return for randomization. Non-participants were more likely to be heavy drinkers and less likely to attend religious services than participants [18]. No differences were observed on measures of depression, stress, or self-reported health.
More comprehensive information about predictors of treatment utilization that moves beyond typical sociodemographic and smoking measures would inform the development of recruitment strategies that can better reach the smokers most in need of treatment and the modification of treatment protocols to maximize their effectiveness in specific subgroups. Co-morbid psychiatric and medical conditions, severity of nicotine dependence, alcohol, and substance abuse, attentional disorders and other neurocognitive conditions, and personality factors are associated with tobacco use, and may play a role in whether smokers take advantage of available treatment resources. In addition, more detailed information about non-participants is crucial to interpreting results of cessation trials, evaluating the generalizability and external validity of findings [19], and determining the feasibility of replicating recruitment processes and interventions [20]. Ultimately, this information will help improve the ability to make a population impact on smoking prevalence by better understanding the characteristics of those smokers who do not participate in intervention research and by tailoring recruitment and intervention efforts to their unique needs [1, 21].
This study affords a unique opportunity to explore a broad range of individual characteristics related to participation in a cessation trial. We recruited smokers from the second generation of a multi-generational birth cohort. The original generation was recruited in the early 1960s as part of a study on birth outcomes. In addition to typical socio-demographics and smoking measures, the original database and a recent follow-up study of the cohort included a rich array of other measures not usually collected in smoking treatment outcomes research (e.g., in utero nicotine exposure, ratings of childhood temperament and cognition, patterns of tobacco use initiation, lifetime measures of co-morbid psychiatric and substance abuse disorders and personality). To date, we know of no studies that have examined in such depth and detail the possible differences in characteristics of participants versus non-participants. Although previous studies have demonstrated links between tobacco use and prenatal (e.g., in utero nicotine exposure), early childhood (e.g., conduct disorder), and lifetime psychiatric (e.g., major depression) factors, our analyses of these variables in relation to treatment participation were largely exploratory. Hypotheses concerning the traditional socio-demographics and smoking measures were consistent with previous studies where replicated results have been reported (e.g., participants are more motivated to quit than non-participants). We also compared eligible participants to age- and state-matched smokers using data from the Behavioral Risk Factor Surveillance System (BRFSS; [22]) to examine the representativeness of our findings beyond the multi-generational cohort used in this study.
Methods
Study Population
Participants were adult offspring of pregnant women enrolled in the National Collaborative Perinatal Project (NCPP) between 1959 and 1966 [23, 24]. The original aims of the NCPP were to identify the developmental consequences of medical conditions arising during pregnancy and delivery. Expectant mothers were enrolled during pregnancy, and their offspring were followed periodically through age 7. Detailed social and medical histories were obtained from mothers at the time of enrollment. Information on offspring birth outcomes and subsequent growth and development was obtained during the first year of life and again at ages 4 and 7 years.
Building on the NCPP, the Transdisciplinary Tobacco Use Research Center–New England Family Study (TTURC–NEFS) was established in 1999 to examine nicotine dependence across the lifespan and across generations. The three major projects of TTURC–NEFS were designed to identify familial, early childhood, and lifetime psychiatric factors that influence (1) lifetime smoking patterns and the natural course of cessation (project 1), (2) trajectories of progression from smoking initiation to dependence among adolescents (project 2), and (3) response to treatment (project 3). The present study describes recruitment into project 3, the TTURC–NEFS smoking cessation treatment study. The study received human subject protections approval from The Miriam Hospital institutional review board.
Cohort Retention and Generalizability
TTURC–NEFS attempted to locate and interview a subset of the surviving NCPP offspring at the Providence, Rhode Island, and Boston, Massachusetts sites (N = 15,721). These included (a) all Providence offspring with one or more siblings enrolled in the NCPP, (b) a sample of all remaining Providence offspring, and (c) a sample of Boston offspring with one or more siblings enrolled in the NCPP. Screening questionnaires were mailed to 4,579 adult offspring and were completed by 3,121 participants (68.2%). Of the screened sample, 2,271 were eligible for enrollment based on the combined inclusion criteria of the three component studies, and 1,674 of these completed the full baseline assessment for project 1 (73.7%).
Table 1 presents demographic characteristics of the full cohort of surviving offspring (n = 15,721), those that were mailed a screening questionnaire (n = 4,579), those that completed the questionnaire (n = 3,121), and those that were interviewed as adults (n = 1,674). Socioeconomic status at birth was based on a composite index adapted from the United States Bureau of the Census that averaged percentiles derived from the education and occupation of the head of the household, as well as family income. This resulted in a continuous measure ranging from 0.3 to 9.3, where 5.0 represents the median socioeconomic status for the USA at the time of the study (1960) and 9.3 indicates the highest socioeconomic status. We conducted two sets of comparisons to examine the generalizability of the screened sample and the final interviewed sample compared to the surviving cohort: (1) the sample that was mailed the screener (N = 4,579) versus those that were not selected for screening (N = 11,142) and (2) the final interviewed sample (N = 1,674) versus those that were not interviewed (N = 14,047).
The groups are highly comparable, with two primary exceptions. First, individuals in the group that was mailed screening questionnaires (N = 4,579) are of lower family socioeconomic status and maternal education (approximately 0.20 standard deviations) compared to the full sample of surviving offspring that were not selected for screening (N = 11,142). This is the result of our emphasis on families who had multiple births during the six-year period of study enrollment (1960–1966). In addition, males were less likely to complete the study interview, resulting in a lower proportion of males in the interviewed sample compared to the remainder of the study cohort. However, in each case, these differences are moderate. Participation rates in various phases of the study did not differ according to maternal race/ethnicity or maternal smoking history.
Information collected as part of the screening questionnaire (N = 3,121) permits us to compare adult characteristics of those eligible participants who did and did not participate in project 1. According to these screening data, rates of current smoking did not differ among those who completed the baseline assessment for project 1 (32.9%) and those who did not (32.3%). Likewise, there were no differences in educational attainment, self-reported health status, or family socioeconomic status. As noted above, those who completed the baseline assessment were more likely to be female than those not interviewed (59.2% versus 49.1%, chi square = 32.1, p < 0.0001). Age at screening was also statistically significant (interviewed = 41.9 ± 0.9 versus non-interviewed = 42.0 ± 1.0, p < .0001), although this difference is not clinically meaningful.
Project 3 Eligibility Criteria
The baseline assessment for project 1 included measures of lifetime patterns of smoking and nicotine dependence, comorbid psychiatric and substance use disorders, self-report personality and social functioning measures, cognitive assessments, and interviews of health and socioeconomic outcomes. Based on this assessment, individuals were eligible for project 3 if they were daily smokers (at least five cigarettes per day), had not been in acute psychiatric crisis in the past 3 months, were not actively abusing alcohol or other drugs, and were not suicidal or unable to provide fully informed consent due to mental illness. The exclusion requirements for study enrollment were minimal to include as many smokers as possible to reach a diverse, heterogeneous population.
Recruitment to Project 3
Following the project 1 assessment, eligible individuals were recruited to project 3. All smokers were encouraged to participate regardless of their motivation or interest in quitting. Recruitment materials emphasized the following benefits of participation: (1) learn easy and manageable ways to improve your health, (2) receive individual support via telephone from a quit smoking expert, (3) receive a free copy of the American Lung Association’s “Freedom from Smoking” booklet, (4) get information and discounts on nicotine gum or the nicotine patch, (5) earn up to $50 for completing follow-up assessments.
Interventions
TTURC–NEFS Project 3 was a randomized controlled trial that compared brief and sustained cessation treatment: (a) the brief treatment condition (BTC; 3 months) consisted of the Freedom From Smoking® Self-Help Manual, a personalized welcome letter, three proactive telephone counseling calls delivered over 3 months, and discounted nicotine replacement therapy ($5 coupon); (b) the sustained multi-modal condition (SMC; 12 months) consisted of the same self-help manual and personalized welcome letter but also included up to two free courses of nicotine gum or patch, three tailored reports, and seven proactive telephone counseling calls. Also, SMC subjects were eligible to receive booklets and additional support calls related to stress/depression, alcohol use, and weight concerns.
Measures
We examined differences between TTURC–NEFS Project 3 participants and non-participants on the following measures.
Demographic Information
Sociodemographic variables assessed at baseline included age, race, ethnicity, gender, marital status, education, household income, and employment.
Medical History Information
Two questions asked whether subjects had received any medical care in the past year for cardiovascular or respiratory conditions.
Smoking History
Smoking history was assessed with the Lifetime Interview of Smoking Trajectories (LIST) developed for TTURC–NEFS. The LIST gathered detailed information on participants’ experiences with tobacco smoking starting with experimentation to progression to regular smoking, levels of consumption, and patterns/duration of quit attempts. Participants also provided information on their ages of first experimentation with smoking and the onset of regular (weekly) and daily smoking.
Fagerstrom Test for Nicotine Dependence
The Fagerstrom Test for Nicotine Dependence (FTND) is a continuous measure of nicotine dependence and is considered to be a standard instrument in the field. The FTND has shown good internal consistency, a single-dimension factor structure, and positive relationships with degree of nicotine intake as assessed by saliva cotinine [25].
Wisconsin Inventory of Smoking Dependence Motives
The Wisconsin Inventory of Smoking Dependence Motives (WISDM-68) [26] is a theory-driven measure that utilizes a multidimensional model of nicotine dependence and includes 13 subscales assessing motivational factors associated with smoking and relapse. The WISDM-68 has shown convergent validity with the FTND and four subscales (automaticity, behavioral choice/melioration, cognitive enhancement, negative reinforcement) have shown predictive validity [26].
Motivational Readiness
Motivation to quit was assessed as a continuous measure using the Readiness Ladder [27]. Validity studies have demonstrated that the Ladder is associated with intention to quit, nicotine dependence, and number of prior quit attempts [27–29]. The Ladder also includes the stages of change algorithm [30], which we report for cross-comparison to other cessation studies.
Quit Methods
Information on quitting history was obtained, including number and recency of lifetime and past-year quit attempts, and lifetime and past-year use of behavioral (e.g., pamphlet, individual counseling, telephone quitline), pharmacological, and other (e.g., acupuncture, hypnosis) quit methods.
In Utero Nicotine Exposure
At each prenatal visit, NCPP mothers reported current smoking and daily smoking rate. The maximum number of cigarettes smoked at any point during pregnancy was determined from these repeated measurements [31]. In utero nicotine exposure was classified as follows: mother never smoked, mother smoked less than a pack during any pregnancy day, and mother smoked a pack or more during any of their pregnancy days.
Center for Epidemiological Studies Depression Scale
The Center for Epidemiological Studies Depression Scale (CES-D) [32] was administered to assess depressed mood. Scores on the CES-D have been positively associated with smoking prevalence, intensity, and failure to quit [33].
Perceived Stress Scale
The four-item Perceived Stress Scale (PSS) [34] was administered because stress has been implicated in problems quitting smoking [35]. The PSS assesses the degree to which subjects perceive their environment and experiences as stressful.
Composite International Diagnostic Interview
The DSM-IV [36] version of the Composite International Diagnostic Interview (CIDI) [37] assessed nicotine dependence, lifetime and current depression, and alcohol use disorders. The CIDI is an epidemiologic diagnostic instrument, which allows non-clinicians to ask questions in a standardized fashion; DSM-IV diagnoses can be computed. Adequate inter-rater reliability, procedural validity, and cross-cultural feasibility have been demonstrated [38, 39]. Lifetime and past-year diagnoses and symptom counts were obtained for each module.
Nicotine Dependence (CIDI)
The CIDI Tobacco Module assesses nicotine dependence in terms of the seven criteria specified by the DSM-IV diagnosis of substance dependence [36]. Items were modified slightly to achieve greater consistency with each of the diagnostic criteria as specified by DSM-IV [40]. Experience of withdrawal symptoms was queried individually for each symptom rather than querying a large cluster of symptoms collectively. Several “sham” symptoms were added for analysis of symptom specificity; responses to sham symptoms are not considered in the current diagnostic scoring. This module was administered to respondents who had reported ever becoming “weekly smokers” (i.e., smoking weekly or more for 2 months or longer). An individual was classified as dependent if he/she experienced at least three of seven dependence criteria.
Depression and Mood Disturbance (CIDI)
The CIDI Depression Module has excellent test–retest reliability [38] and inter-rater reliability with kappas ranging from 0.95 to 1.00 [39, 41]. The version of the CIDI that we adapted for the TTURC-NEFS assessed lifetime and current depression. The primary change made to the CIDI was to incorporate additional questions about the nature of the depressive episode before the detailed assessment of the symptoms experienced during that episode. This procedure allowed us to exclude non-qualifying episodes (e.g., bereavement) for a more accurate categorization of depressive episodes than offered by the original instrument and to estimate the number of lifetime independent depressive episodes.
Alcohol (CIDI)
Participants completed the alcohol module if they reported on a screener repeated heavy drinking or monthly drinking with an average of three or more drinks per occasion, or reported that they or other people had thought that they had a problem with drinking. Dependence symptoms were assessed regardless of responses to abuse symptoms. Withdrawal symptoms were assessed individually with withdrawal only being coded as present if at least two symptoms were endorsed, consistent with DSM-IV.
Diagnostic Interview Schedule
Modules from the fourth version of the Diagnostic Interview Schedule (DIS) [42] were used to assess substance use disorders, conduct disorder, antisocial personality disorder (ASPD), and attention deficit and hyperactivity disorder (ADHD). We shortened the administration of the DIS by modifying it to eliminate items that are not essential for the assessment of DSM abuse and dependence symptoms. Therefore, we were able to attain abuse and dependence diagnoses for all drug classes while minimizing the amount of time used in assessing low-prevalence disorders. We report abuse and dependence findings for the two most prevalent drugs: marijuana and cocaine. We made similar modifications to the conduct disorder and ASPD modules, eliminating items that are not essential for diagnosis but retaining the key elements of the interview.
Childhood and adult ADHD were assessed using a modified version of the DIS, known as the Longitudinal Interview for Symptoms of Attention (LISA) [43]. This approach involves establishing specific criteria as set forth in DSM-IV and querying retrospectively whether these symptoms were experienced in childhood and whether these symptoms have persisted into adulthood (cf. [44]). These modifications retain the original order and content of the standard DIS ADHD module. We examined symptom counts for the number of symptoms of inattention (0–9), hyperactivity (0–9), and total ADHD symptoms (0–18) experienced during childhood. For all symptoms endorsed for childhood, subjects also reported whether these had occurred within the past 6 months.
Multidimensional Personality Questionnaire
A shortened version of the Multidimensional Personality Questionnaire (MPQ) [45] assessed personality traits that contribute to susceptibility to nicotine dependence. This version included all but two subscales (the absorption primary scale or items from the primary scales related to positive emotionality) because of their weak associations with psychopathology [46, 47]. The MPQ yields higher order factors of negative emotionality (containing the primary scales of stress reaction, alienation, and aggression) and constraint (control, harm avoidance, and traditionalism), the two primary personality dimensions of interest in relation to nicotine dependence.
Early Childhood Risk Factors
Cognitive performance at age seven was assessed using seven subtests from the Wechsler Intelligence Scale for Children (WISC) [48]. The WISC provided estimates of full scale (FSIQ), verbal (VIQ), and performance IQ (PIQ). The mean FSIQ in this sample was 97.5 with a standard deviation of 12.8. In the general population, the mean FSIQ is 100 with a standard deviation of 15.
Ratings of child behavior problems at age 7 were based upon psychologist observations. Observers completed 15 items, including fearfulness, rapport with examiner, emotional reactivity, degree of cooperation, duration of attention span, level of activity, assertiveness, and hostility. A subsequent principal components analysis yielded two primary scales reflecting internalizing behavior (e.g., shy/withdrawn, fearful/apprehensive, passive, limited communication) and externalizing behavior (resistive, assertive, hostile, acts out, and impulsive). Cronbach’s alphas were 0.85 and 0.80, respectively, for the internalizing and externalizing scales.
Analytic Plan
Relative frequencies for categorical variables and descriptive statistics for continuous variables were used to summarize demographic and socio-economic characteristics, substance use rates, and psychiatric comorbidity rates. Univariate analyses were conducted to examine differences in these variables between participants and non-participants in the smoking cessation trial. Statistical significance levels were calculated using t tests for examining mean differences in continuous variables, and chi square tests for examining differences in proportions for categorical variables. For categorical variables with more than two levels, squared Pearson residuals were investigated to examine the source of any statistically significant differences. When cell counts were small (<5), p values were based on Fisher’s exact test. Age-of-onset data from the LIST was compared using non-parametric survival analysis techniques for possibly censored data available in PROC LIFEREG and PROC LIFETEST of SAS/STAT 8.2 [49]. Post hoc logistic regression analyses were conducted to examine whether differences between participants and non-participants remained significant after controlling for important covariates.
We compared the TTURC–NEFS smokers to the broad population of smokers in Rhode Island and Massachusetts using data from the BRFSS [22]. The BRFSS is an annual telephone-based survey of health and health-risk behaviors that has samples representative of each state. Most TTURC–NEFS participants were recruited in 2003 and were between the ages of 35–43. To make the samples comparable, we selected individuals in Rhode Island and Massachusetts of the same age range interviewed in 2003 (N = 563). Population quantities were measured using sample survey weights that accounted for unequal probabilities of selection. Testing of differences between the two samples included variance adjustments to account for the complex sampling design.
Results
Recruitment Results
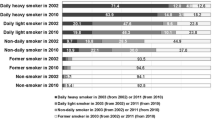
Of the 1,674 interviews completed by project 1, 1,494 were conducted during the TTURC–NEFS Project 3 enrollment period (June 2001–December 2003): 160 (10.7%) were never smokers, 898 (60.1%) were former smokers, and 436 (29.2%) were current smokers. Of the 436 current smokers, 421 were eligible for project 3 (28.2% of the original sampling frame). Reasons for ineligibility included never/no longer smoking or smoking less than five cigarettes per day (N = 1053, 98.1%), problematic drug use in the past 3 months (N = 14, 1.3%), problematic alcohol use in the past 3 months (N = 21, 2.0%), medical hospitalization in the past 3 months (N = 3, 0.3%), or psychiatric hospitalization in the past 3 months (N = 4, 0.4%). Individuals could be ineligible for more than one reason. Of the 421 eligible current smokers who were invited to participate in project 3, 244 (58%) agreed to participate. Baseline assessment data from TTURC–NEFS Project 1 are available on all project 3 participants (N = 244) and non-participants (N = 177).
TTURC–NEFS Smokers Versus General Population
Although many of the absolute differences were small, as indicated in Table 2, TTURC–NEFS smokers differed from the general population as follows: TTURC–NEFS smokers were slightly younger (M = 38.9, SD = 1.8 versus M = 39.3, SD = 2.5, p < .0001), less likely to be Hispanic (1.2% versus 7.9%, p < .0001), and more likely to be female (61.6% versus 49.7%, p < 0.0001), never married (32.3% versus 22.7%, p < 0.0001) and have a high school degree or less (64.1% versus 50.3%, p < .0001). Compared to the population average, the TTURC–NEFS sample was younger when they began smoking (age in years, M = 13.3, SD = 3.8 versus M = 14.8, SD = 3.4, p < .0001) and when they became regular smokers (age in years, M = 15.8, SD = 4.3 versus M = 17.3, SD = 3.7, p < 0.0001). Additionally, the TTURC–NEFS smokers were less likely to have made a quit attempt in the previous year (42.5% versus 59.1%, p < 0.0001).
Participants Versus Non-Participants
As shown in Table 3, there were relatively few differences between participants and non-participants on the demographic and health variables we examined. Participants were more likely to have never married (37.3% versus 25.4%, p = .025) and to have a household income below $35,000 (34.3% versus 19.6%, p = .01) than non-participants.
Among the smoking variables examined in Table 4, participants scored higher on several measures of nicotine dependence than non-participants: CIDI symptom count (M = 5.2, SD = 1.6 vs. M = 4.8, SD = 1.6, p = .01), DSM-IV symptom count (M = 4.3, SD = 1.5 vs. M = 3.9, SD = 1.5, p = .005), and the WISDM-68 (M = 3.6, SD = 1.1 vs. M = 3.4, SD = 1.1, p = .042). Participants were more motivated to quit smoking than non-participants as indicated by the continuous measure on the Readiness Ladder (M = 5.6, SD = 1.4 vs M = 5.1, SD = 1.7, p = .003) and categorical data on the Stages of Change (23.6% vs. 16.2% in preparation, p = .049). Participants also reported greater lifetime usage of behavioral quit methods (M = 0.3, SD = 1.2 vs. M = 0.1, SD = 0.4, p = .026) than non-participants. Finally, participants were more likely to have had higher levels of in utero nicotine exposure than non-participants (44.4% vs. 33.9%, p = .03) using the dichotomous threshold [31].
As shown in Table 5, there were few differences in comorbid conditions between participants and nonparticipants. Participants had higher average scores on the CES-D (M = 8.9, SD = 6.6 versus M = 7.0, SD = 5.7, p = .005) and Perceived Stress Scale (M = 6.1, SD = 3.1 versus M = 5.3, SD = 3.5, p = .021). Participants also had higher scores on a measure of Internalizing Behavior and lower scores on the verbal IQ subscale of the WISC.
Post hoc logistic regression analyses were conducted to determine if differences between participants and non-participants remained significant after controlling for important covariates. Gender was included as a covariate in the models, given its association with stress, depression, internalizing behavior, and verbal IQ. We also controlled for marital status and income because participants and non-participants differed on these variables. From Table 4, motivational readiness and the three measures of nicotine dependence remained statistically significant predictors of participation, with higher scores among participants: Ladder (OR = 1.43, 95% CI = 1.17–1.74, p = 0.000), CIDI (OR = 1.26, 95% CI = 1.08–1.46, p = .003), DSM-IV (OR = 1.29, 95% CI = 1.10–1.51, p = 0.002), WISDM-68 (OR = 1.26, 95% CI = 1.01–1.57, p = .045). From Table 5, only CES-D (OR = 1.05, 95% CI = 1.00–1.10, p = .039) and stress (OR = 1.10, 95% CI = 1.02–1.20, p = .016) remained statistically significant predictors of participation.
Discussion
This study extends our knowledge about the characteristics of participants versus non-participants recruited for a randomized clinical trial (RCT) of smoking cessation. Of all eligible smokers available in the cohort, a respectable 58% were proactively enrolled. Participants were recruited from a defined sample embedded within a larger study of a longitudinal birth cohort that provided rich information about participants and non-participants, with both prospective and retrospective data. Moreover, participants were also compared with a representative, matched regional subsample of the BRFSS. This is the only study we are aware of that has examined factors related to participation in a smoking cessation RCT in this depth and breadth.
Few measures differentiated the participants in the RCT from the non-participants; most of those differences were statistically significant but of small magnitude, and many differences also became non-significant after covariate analyses controlled for gender, income, and marital status. On early childhood measures, small but statistically significant differences emerged between participants and non-participants on verbal IQ (94 versus 96) and internalizing behavior (1.3 versus 0.8). All differences became non-significant after adjustment for covariates. There were no differences on any other early childhood measures, such as attention or hyperactivity. The retrospective adult measures of lifetime alcohol/drug disorders, attention/hyperactivity, personality, cognition, conduct, or antisocial personality disorder did not distinguish participants from non-participants. Finally, there were no differences between participants and non-participants on measures of smoking initiation, the age of progression from first puff to regular and daily smoking, or on smoking rate.
Participants in the RCT were significantly more likely than non-participants to have been exposed in utero to a pack a day or more of maternal smoking. The nature of this relationship is unclear but may parallel links between in utero exposure and nicotine dependence. In a prior study [31], the offspring of TTURC–NEFS mothers who smoked a pack or more on any pregnancy day were almost twice as likely to progress from smoking experimentation to nicotine dependence and to meet DSM criteria for lifetime nicotine dependence. Finally, it is noteworthy that the difference in in utero exposure between participants and non-participants was no longer significant when controlling for gender, income, and marital status.
Participants in this study also reported higher scores on several measures of nicotine dependence, including the WISDM-68, and symptom-counts using both CIDI and DSM-IV criteria. However, there were no differences on the FTND, DSM-IV diagnosis of nicotine dependence, or time to first cigarette. The reasons for inconsistency across different measures of dependence are unclear but may be due to statistical power (i.e., power is lower for binary than continuously scaled data) or differences in measurement approaches to the construct of dependence. For example, CIDI and DSM-IV symptoms counts were designed to be more sensitive approaches to assessing specific aspects of nicotine dependence that may not have been picked up by diagnostic instruments such as the DSM-IV. Differences in the conceptualization of the construct of nicotine dependence (i.e., multidimensional in the WISDM-68 versus unidimensional in the FTND and DSM-IV; e.g., [26, 50, 51, 52]) may also have contributed to these results. The differences between participants and non-participants on the CIDI, DSM-IV, and WISDM-68 persisted even after covariance of gender, income, and marital status.
Not surprisingly, participants reported higher levels of motivation to quit than non-participants even after covariate analyses. Compared with non-participants, participants in the RCT were also more likely to report higher levels of stress and current symptoms of depression (even after covariance analyses). It is interesting that participants differed from non-participants on measures of current mood but not on lifetime depression. These results are consistent with previous studies that have shown no relationship between cessation and history of depression [53] but strong links between current depressed mood and difficulty quitting [54–57]. Participants were also more likely to have used behavioral cessation methods in the past, though this finding was no longer significant after covariance analysis. On sociodemographic variables, participants in the RCT were more likely to have never married and have lower incomes.
Compared to the regional subsample of the national BRFSS, eligible smokers were slightly younger, more likely to be female, never married, have a high school degree or less, and less likely to be Hispanic. The very high statistical significance of the 7-month difference in mean age simply highlights the enormous statistical power in this study to detect even very small differences, especially given that we extracted regional BRFSS subsample data using the identical age range and years of recruitment as in our sample. The other demographic differences are also small, unlikely to be clinically meaningful, and expected given the slight skew toward participants of lower socioeconomic status in the original NCPP birth cohort [58].
The study has several limitations. First, the use of the TTURC–NEFS longitudinal birth cohort froze in place of the demographic structure representative of Rhode Island and Massachusetts in the 1960s and does not reflect changes since that time (e.g., increase in Hispanic population). In addition, the TTURC–NEFS cohort had a restricted age range of about 8 years (M = 38.9, range 35–43). However, this is an age range when many smokers become interested in treatment programs [59–61]. Second, given the large number of measures taken prospectively and retrospectively across the lifespan of the cohort and the relatively small number of significant differences, we have chosen to present the results in the form of descriptive statistics, with more detailed examination of selected covariates. Some of the differences noted here could still have been obtained by chance. Finally, the original NCPP cohort and the selected subsamples of adult offspring may have had inherent selection biases of unknown implications for interpretation of these results. However, the comparisons presented in this paper revealed minimal and expected differences within the various subgroups. The comparisons reported here are all quite reassuring against large selection biases (e.g., comparing the sample of offspring completing a screener but not the full survey; the additional comparison of the NCPP cohort with the regional and representative BRFSS survey constructed at about the same time as the TTURC–NEFS survey). Few studies we know of have had access to information reported here on several of the levels of denominators.
The encouraging conclusion is that smokers who enroll in cessation trials may not differ much or in clinically significant ways from those who do not participate. Differences observed on measures of nicotine dependence, stress, and current depressed mood illustrate the importance of determining who comprises the target population before recruitment for any intervention study so as to more effectively tailor recruitment and intervention efforts. This information is also critical to interpret results of cessation trials, evaluate their generalizability, and determine whether the recruitment strategies and interventions are relevant and equally effective when applied in dissemination and implementation trials [20]. This profile of participant characteristics is also encouraging insofar as stress/depressed mood and nicotine dependence can be feasibly addressed in the context of an intervention.
This study begins to address some of the concerns about moving from RCT trials of efficacy under ideal conditions to broader effectiveness trials in the real world [62, 63]. Most treatment studies only report the characteristics of those randomized. Many studies also recruit participants reactively, obtaining self-selected volunteers from an undefined population of unknown characteristics and with an unknown denominator [64]. These gaps limit the generalizability and external validity of interventions. As a result, the impact of an intervention [1] and its efficiency [62] cannot be easily interpolated. Moreover, as the characteristics of the smokers who did not participate in treatment are unknown, their needs for treatment are largely unknown. Gathering this information is critical if we are to learn how to make cessation treatments more attractive so that smokers want them, expect them, ask for them, and use them [65].
References
Abrams DB, Orleans CT, Niaura RS, et al. Integrating individual and public health perspectives for treatment of tobacco dependence under managed health care: a combined stepped-care and matching model. Ann Behav Med. 1996; 18: 290–304.
Centers for Disease Control and Prevention. Cigarette smoking among adults—United States, 2004. Morb Mortal Wkly Rep. 2005; 54: 1121–1124.
Zhu S, Melcer T, Sun J, Rosbrook B, Pierce JP. Smoking cessation with and without assistance: a population-based analysis. Am J Prev Med. 2000; 18: 305–311.
Cokkinides VE, Ward E, Jemal A, Thun MJ. Under-use of smoking-cessation treatments: results from the National Health Interview Survey, 2000. Am J Prev Med. 2005; 28: 119–122.
McDonald PW. Population-based recruitment for quit-smoking programs: an analytic review of communication variables. Prev Med. 1999; 28: 545–557.
Glasgow RE, Klesges RC, Klesges LM, Somes GR. Variables associated with participation and outcome in a worksite smoking control program. J Consult Clin Psychol. 1988; 56: 617–620.
Linnan LA, Emmons KM, Klar N, et al. Challenges to improving the impact of worksite cancer prevention programs: comparing reach, enrollment, and attrition using active versus passive recruitment strategies. Ann Behav Med. 2002; 24: 157–166.
Mak YW, Loke AY, Lam TH, Abdullah AS. Predictors of the participation of smoking parents in a proactive telephone-based smoking cessation program. Addict Behav. 2006; 31: 1731–1743.
Holtrop JS, Wadland WC, Vansen S, Weismantel D, Fadel H. Recruiting health plan members receiving pharmacotherapy into smoking cessation counseling. Am J Manag Care. 2005; 11: 501–507.
Pisinger C, Vestbo J, Borch-Johnsen K, Thomsen T, Jorgensen T. Acceptance of the smoking cessation intervention in a large population-based study: the Inter99 study. Scand J Public Health. 2005; 33: 138–145.
Fortmann SP, Killen JD. Who shall quit? Comparison of volunteer and population-based recruitment in two minimal-contact smoking cessation studies. Am J Epidemiol. 1994; 140: 39–51.
Pohl JM, Martinelli A, Antonakos C. Predictors of participation in a smoking cessation intervention group among low-income women. Addict Behav. 1998; 23: 699–704.
Klesges RC, Brown K, Pascale RW, et al. Factors associated with participation, attrition, and outcome in a smoking cessation program at the workplace. Health Psychol. 1988; 7: 575–589.
Kviz FJ, Crittenden KS, Warnecke RB. Factors associated with nonparticipation among registrants for a self-help, community-based smoking cessation intervention. Addict Behav. 1992; 17: 533–542.
Velicer WF, Keller S, Friedman RH, et al. Comparing participants and nonparticipants recruited for an effectiveness study of nicotine replacement therapy. Ann Behav Med. 2005; 29: 181–191.
Gritz ER, Berman BA, Bastani R, Wu M. A randomized trial of a self-help smoking cessation intervention in a nonvolunteer female population: testing the limits of the public health model. Health Psychol. 1992; 11: 280–289.
Brod MI, Hall SM. Joiners and non-joiners in smoking treatment: a comparison of psychosocial variables. Addict Behav. 1984; 9: 217–221.
Ahluwalia JS, Richter K, Mayo MS, et al. African American smokers interested and eligible for a smoking cessation clinical trial: predictors of not returning for randomization. Ann Epidemiol. 2002; 12: 206–212.
Glasgow RE, Vogt TM, Boles SM. Evaluating the public health impact of health promotion interventions: the RE-AIM framework. Am J Public Health. 1999; 89: 1322–1327.
Glasgow RE, McCaul KD, Fisher KJ. Participation in worksite health promotion: a critique of the literature and recommendations for future practice. Health Educ Q. 1993; 20: 391–408.
Abrams DB, Leslie F, Mermelstein R, Kobus K, Clayton RR. Transdisciplinary tobacco use research. Nicotine Tob Res. 2003; 5Suppl 1: S5–S10.
Centers for Disease Control and Prevention. Behavioral Risk Factor Surveillance System Survey Data. Atlanta, GA: U.S. Department of Health and Human Services, Centers for Disease Control and Prevention; 2003.
Niswander KR, Gordon M. The Women and Their Pregnancies: The Collaborative Perinatal Study of the National Institute of Neurological Diseases and Stroke. Washington: National Institute of Health; 1972.
Broman SH. The collaborative perinatal project: an overview. In: Mednick SA, Harway M, Finello KM, eds. Handbook of Longitudinal Research. New York: Praeger; 1984: 182–215.
Heatherton TF, Kozlowski LT, Frecker RC, Fagerstrom KO. The Fagerstrom test for nicotine dependence: a revision of the Fagerstrom tolerance questionnaire. Br J Addict. 1991; 86: 1119–1127.
Piper ME, Piasecki TM, Federman EB, et al. A multiple motives approach to tobacco dependence: The Wisconsin Inventory of Smoking Dependence Motives (WISDM-68). J Consult Clin Psychol. 2004; 72: 139–154.
Biener L, Abrams DB. The contemplation ladder: validation of a measure of readiness to consider smoking cessation. Health Psychol. 1991; 10: 360–365.
Abrams DB, Biener L. Motivational characteristics of smokers at the workplace: a public health challenge. Prev Med. 1992; 21: 679–687.
Curry SJ, Grothaus L, McBride C. Reasons for quitting: intrinsic and extrinsic motivation for smoking cessation in a population-based sample of smokers. Addict Behav. 1997; 22: 727–739.
Prochaska JO, DiClemente CC, Norcross JC. In search of how people change. Applications to addictive behaviors. Am Psychol. 1992; 47: 1102–1114.
Buka SL, Shenassa ED, Niaura R. Elevated risk of tobacco dependence among offspring of mothers who smoked during pregnancy: a 30-year prospective study. Am J Psychiatry. 2003; 160: 1978–1984.
Radloff LS. A new self-report depression scale for research in the general population. Appl Psychol Meas. 1977; 1: 385–401.
Anda RF, Williamson DF, Escobedo LG, et al. Depression and the dynamics of smoking. A national perspective. JAMA. 1990; 264: 1541–1545.
Cohen S, Kamarck T, Mermelstein R. A global measure of perceived stress. J Health Soc Behav. 1983; 24: 385–396.
Cohen S, Lichtenstein E, Prochaska JO, et al. Debunking myths about self-quitting. Evidence from 10 prospective studies of persons who attempt to quit smoking by themselves. Am Psychol. 1989; 44: 1355–1365.
American Psychiatric Association. Diagnostic and Statistical Manual of Mental Disorders. 4th ed. Washington, DC: American Psychological Association; 1994.
World Health Organization. Composite International Diagnostic Interview Computer Programs. Geneva: World Health Organization; 1990.
Wittchen HU. Reliability and validity studies of the WHO–Composite International Diagnostic Interview (CIDI): a critical review. J Psychiatr Res. 1994; 28: 57–84.
Wittchen HU, Robins LN, Cottler LB, et al. Cross-cultural feasibility, reliability and sources of variance of the Composite International Diagnostic Interview (CIDI). The Multicentre WHO/ADAMHA Field Trials. Br J Psychiatry. 1991; 159: 645–653, 658.
Dierker LC, Donny E, Tiffany S, et al. The association between cigarette smoking and DSM-IV nicotine dependence among first year college students. Drug Alcohol Depend. 2007; 86: 106–114.
Andrews G, Peters L, Guzman AM, Bird K. A comparison of two structured diagnostic interviews: CIDI and SCAN. Aust N Z J Psychiatry. 1995; 29: 124–132.
Robins LN, Helzer JE, Croughan J, Ratcliff KS. National institute of mental health diagnostic interview schedule. Its history, characteristics, and validity. Arch Gen Psychiatry. 1981; 38: 381–389.
Buka SL. “Learning Disabled Children Grown Up:” Natural history from birth through adulthood. DIS Newsletter. 1999; Winter.
Murphy K, Barkley RA. Attention deficit hyperactivity disorder adults: comorbidities and adaptive impairments. Compr Psychiatry. 1996; 37: 393–401.
Tellegen A. Brief Manual for the Multidimensional Personality Questionnaire. Minneapolis: University of Minnesota; 1982.
Krueger RF, Caspi A, Moffitt TE, Silva PA, McGee R. Personality traits are differentially linked to mental disorders: a multitrait-multidiagnosis study of an adolescent birth cohort. J Abnorm Psychol. 1996; 105: 299–312.
McGue M, Slutske W, Taylor J, Iacono WG. Personality and substance use disorders: I. Effects of gender and alcoholism subtype. Alcohol Clin Exp Res. 1997; 21: 513–520.
Wechsler D. Wechsler Intelligence Scale for Children. New York: The Psychological Corporation; 1949.
SAS/STAT Software. Changes and Enhancements. Cary, NC: SAS Institute, Inc.; 2001.
Shadel WG, Shiffman S, Niaura R, Nichter M, Abrams DB. Current models of nicotine dependence: what is known and what is needed to advance understanding of tobacco etiology among youth. Drug Alcohol Depend. 2000; 59Suppl 1: S9–S22.
Etter JF. Comparing the efficacy of two Internet-based, computer-tailored smoking cessation programs: a randomized trial. J Med Internet Res. 2005; 7: e2.
Pomerleau CS, Carton SM, Lutzke ML, Flessland KA, Pomerleau OF. Reliability of the Fagerstrom tolerance questionnaire and the Fagerstrom test for nicotine dependence. Addict Behav. 1994; 19: 33–39.
Hitsman B, Borrelli B, McChargue DE, Spring B, Niaura R. History of depression and smoking cessation outcome: a meta-analysis. J Consult Clin Psychol. 2003; 71: 657–663.
Borrelli B, Bock B, King T, Pinto B, Marcus BH. The impact of depression on smoking cessation in women. Am J Prev Med. 1996; 12: 378–387.
Cinciripini PM, Wetter DW, Fouladi RT, et al. The effects of depressed mood on smoking cessation: mediation by postcessation self-efficacy. J Consult Clin Psychol. 2003; 71: 292–301.
Niaura R, Britt DM, Shadel WG, et al. Symptoms of depression and survival experience among three samples of smokers trying to quit. Psychol Addict Behav. 2001; 15: 13–17.
Berlin I, Covey LS. Pre-cessation depressive mood predicts failure to quit smoking: the role of coping and personality traits. Addiction. 2006; 101: 1814–1821.
Buka SL, Tsuang MT, Lipsitt LP. Pregnancy/delivery complications and psychiatric diagnosis. A prospective study. Arch Gen Psychiatry. 1993; 50: 151–156.
Zhu SH, Anderson CM, Tedeschi GJ, et al. Evidence of real-world effectiveness of a telephone quitline for smokers. N Engl J Med. 2002; 347: 1087–1093.
Lancaster T, Stead LF. Individual behavioural counselling for smoking cessation. Cochrane Database Syst Rev. 2005; CD001292.
Stead LF, Lancaster T. Group behaviour therapy programmes for smoking cessation. Cochrane Database Syst Rev. 2005; CD001007.
Glasgow RE, Klesges LM, Dzewaltowski DA, Estabrooks PA, Vogt TM. Evaluating the impact of health promotion programs: using the RE-AIM framework to form summary measures for decision making involving complex issues. Health Educ Res. 2006; 21: 688–694.
Kerner J, Rimer B, Emmons K. Introduction to the special section on dissemination: Dissemination research and research dissemination: How can we close the gap? Health Psychol. 2005; 24: 443–446.
Graham AL, Bock BC, Cobb NK, Niaura R, Abrams DB. Characteristics of smokers reached and recruited to an internet smoking cessation trial: a case of denominators. Nicotine Tob Res. 2006; 8Suppl 1: S43–S48.
National Institutes of Health State-of-the-Science conference statement. Tobacco use: Prevention, cessation, and control. Ann Intern Med. 2006; 145: 839–844.
Acknowledgment
This study was supported by (or in part by) the National Institutes of Health (NIH), Transdisciplinary Tobacco Use Research Center (TTURC) Award (P50 CA084719), the National Cancer Institute, the National Institute on Drug Abuse, and the Robert Wood Johnson Foundation. We thank Ms. Barbara Doll and Ms. Susan Marx for their assistance in preparing the final manuscript.
Author information
Authors and Affiliations
Corresponding author
About this article
Cite this article
Graham, A.L., Papandonatos, G.D., DePue, J.D. et al. Lifetime Characteristics of Participants and Non-participants in a Smoking Cessation Trial: Implications for External Validity and Public Health Impact. ann. behav. med. 35, 295–307 (2008). https://doi.org/10.1007/s12160-008-9031-1
Received:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12160-008-9031-1