Abstract
Background
Having close social relationships and being married specifically have been reliably associated with health benefits including lower morbidity and mortality.
Purpose
The purpose of this study was to examine the influence of marital status, relationship quality, and network support on measures of psychological and cardiovascular health.
Method
We examined ambulatory blood pressure (ABP) among 204 married and 99 single males and females (N = 303).
Results
We found that both marital status and marital quality were important. Married individuals had greater satisfaction with life (SWL) and blood pressure dipping than single individuals. High marital quality was associated with lower ABP, lower stress, less depression, and higher SWL. Importantly, contrasting those who are unmarried with those in low-quality marriages, we find that single individuals had lower ABP—suggesting that single individuals fare better than their unhappily married counterparts. Likewise, having a supportive network did not moderate (i.e., buffer) the effects of being single or unhappily married.
Conclusions
Findings indicate being married per se is not universally beneficial, rather, the satisfaction and support associated with such a relationship is important. However, marriage may be distinctive, as evidence further suggests that support from one’s network does not compensate for the effect of being single. These results highlight the complexities in understanding the influence of social relationships on long-term health, and they may help clarify the physiological pathways by which such associations exist.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Epidemiological research suggests that social relationships may significantly protect individuals from various causes of morbidity and mortality [1, 2]. For most adults, marriage plays a central role in their lives even compared to other social relationships. Therefore, this particular relationship has been given a great deal of importance in understanding the association with well-being. For instance, prior research suggests that married adults have lower rates of morbidity and mortality compared to unmarried adults [3]. Likewise, married individuals have greater life satisfaction, happiness, and lower risk for depression [4, 5]. However, many adults, through circumstance or by choice, remain single (unmarried). Are such individuals destined to have poorer health? It appears that prior research is not clear-cut and has several limitations.
One limitation is that many studies focused on marital status, ignoring the quality of relationships. Research suggests that past negativity in relationships predicts greater mortality [6], and unhappily married couples are unlikely to experience the same health benefits as their happily married counterparts [7, 8]. Thus, a complete understanding of the health-related consequences of marriage requires consideration of both its negative and positive aspects. Research that has examined relationship quality has almost exclusively done so separately from marital status. The few studies that examined status and quality concurrently [4, 9, 10] demonstrate that those in high-quality relationships had better outcomes than those in low-quality relationships and single individuals. However, these studies did not directly contrast groups at greater risk (i.e., unhappily married and unmarried) on measures that inform physical health.
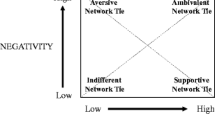
Given that social relationships have costs and benefits, it is also important to understand whether the benefits of other relationships can compensate for any costs. For instance, do single adults with sufficient network social support experience the same health benefits as those who are married? The idea that perceptions of social support in one social domain can reduce the negative effect associated with conflict in another domain was proposed and tested by Lepore [11] in what he termed cross-domain buffering. While spousal support appears to buffer stressful relationships at work [12], studies have not examined whether costs associated with the marital relationship (i.e., lack of a marriage or lack of a happy marriage) can be buffered by other supportive relationships. Presently, it is unclear whether the spousal relationship may be distinctive in impact.
Another limitation of prior studies is that despite strong evidence that social relationships are linked to important health-related outcomes, less is known regarding how social relationships influence disease processes. Marriage is purported to offer protection through processes that include economic well-being, healthier lifestyles, lower stress, and social support [8, 13]. The prevailing evidence supports the stress/social support hypothesis which can account for both the protective and detrimental effects of marriage [14, 15]. As such, marriage is thought to influence health through relevant psychological and physiological processes [see 14, 15 for reviews].
One important biological pathway by which marriage and/or social relationships more generally may impact health is via cardiovascular functioning. While evidence links social support and marital conflict to heart rate and blood pressure (BP) in laboratory studies, much less is known about relationship effects within daily life. Importantly, studies suggest that elevated ambulatory BP (ABP) is a stronger predictor of cardiovascular outcomes, including severity of complications in essential hypertension, left ventricular hypertrophy, and overall morbidity and mortality, than are clinic BP readings [16]. In addition to BP during waking hours, nocturnal BP may be important. There is typically a 15–20% reduction in BP (or dipping) that occurs during the night. A lack of nocturnal BP dipping may occur among healthy individuals, and stress has been implicated as a cause [17]. Decreased BP dipping is thought to contribute to an increase in overall pressure load, over time leading to organ damage. Importantly, a lack in BP dipping is an independent predictor of negative health outcomes, including cardiovascular morbidity [18] and even increased mortality [19, 20]. In fact, evidence from large prospective studies indicates that for each 5% increment in the dipping ratio (i.e., night BP/daytime BP), there is a 20–30% increase in cardiovascular morbidity and mortality [20, 21]. Thus, decreased BP dipping may have important long-term health implications. Given the substantial body of research linking social relationships to cardiovascular outcomes, it is surprising that currently, no studies have examined the influence of marriage or relationship quality on BP dipping.
Present Study
Despite the large literature linking social relationships (including marriage) to both mental and physical health, many questions remain unanswered. This study attempted to answer the question: Are some relationships more beneficial/detrimental than others? Specifically, we examined the relative importance of marital status and quality, whether unmarried individuals may potentially benefit from other close supportive relationships, and whether the quality of the marital relationship is more impactful than other relationships.
Method
Subjects and Procedures
Our sample consisted of 303 adults, ages 20 to 68, recruited from the community through paid advertisement. Within this sample, there were 204 married (99 men, 105 women) and 99 single (48 men, 51 women) individuals. The sample was primarily Caucasian (82%) and educated (16.41 years of education). No unmarried participants were cohabitating with a romantic partner. We used self-reported inclusion criteria consistent with prior research [e.g., 22] to select healthy participants. Participants were also excluded if pregnant. Qualified participants came to the lab, and after informed consent was obtained, completed a packet of questionnaires, and a trained research assistant placed the ABP monitor on them. Participants left the lab and were instructed to go about their normal activities while wearing the monitor throughout the day and night. They returned to the lab 24 h later.
Measures
Self-Report Questionnaires
Participants completed a packet of questionnaires that assessed basic demographics of our sample, marital quality, network support, and mental health. To assess marital relationship quality, we used the short Marital Adjustment Test (MAT) and the Dyadic Adjustment Scale (DAS). The MAT assesses major areas of adjustment and has demonstrated ability to discriminate between well-adjusted and maladjusted marriages [23]. We also included the satisfaction subscale of the DAS [24]. Both measures of marital quality demonstrated adequate reliability (α = 0.79) within this study. The Interpersonal Support Evaluation List (ISEL) was used to assess total social support and includes the specific dimensions of appraisal, self-esteem, belonging, and tangible support. The ISEL has demonstrated reliability [25]. The internal consistency for this sample was also high (α = 0.95). We also administered the Center for Epidemiological Studies Depression Scale [26], Satisfaction With Life Scale (SWL) [27), and the Perceived Stress Scale [28]. Each of these measures is widely used and validated within the literature and demonstrated high internal consistency (i.e., α = 0.85, α = 0.88, α = 0.85, respectively) within this study.
Ambulatory Blood Pressure
The Accutracker II (Suntech Medical Instruments, Raleigh, NC) was used to estimate ambulatory readings of systolic and diastolic BP (SBP, DBP) using the auscultatory method. The Accutraker II is well-validated, as readings correspond with intra-arterial BP assessments during rest, isometric exercise, and bicycle exercise [29]. The monitor was set to randomly take a reading approximately every 20 min during the day and 60 min during the night. Based on prior research [30, 31], we deleted readings based on established criteria associated with test codes and outliers indicating artifactual readings. We examined ambulatory readings according to three segments: 24-h ABP, an average of all readings to examine overall BP load; daytime ABP, an average across the readings during daytime hours when social interaction would be most likely; and BP dipping, a change score, subtracting the average nighttime ABP (11 p.m.–6 a.m.) from the average daytime ABP (6 a.m.–11 p.m.) [22]. Thus, higher scores indicate more dipping.
Results
Preliminary Analyses
We found no significant difference in age (m = 31.16) or body mass index (m = 24.71) between single and married participants. Most single participants had never married (89%).Footnote 1 Among married participants, length of marriage ranged from 1 to 42 (m = 8.09) years. Approximately one third (35.5%) of our sample would be classified as pre-hypertensive (ambulatory SBP ≥ 120 or DBP ≥ 80 mmHg).
Primary Analyses
To examine our research questions, covariate selection was determined by identifying factors known to independently contribute to BP or mental health measures that could potentially confound the results. All analyses of mental health measures statistically controlled for gender, while analyses of ABP statistically controlled for genderFootnote 2 and age. When examining BP dipping, we also included daytime measures of the relevant cardiovascular assessments as covariates to account for any potential effect of initial values.
Marital Status, Marital Quality, and Mental Health
We first performed separate analyses of covariance examining the effect of marital status on SWL, stress, and depression. We found a significant main effect of marital status for SWL [F(3,289) = 15.55, p < 0.0001]. SWL was higher among married (m = 21.69) than single (m = 19.22) persons. We found no significant difference between married and single persons on levels of stress or depression.
Separate regression analyses were performed to examine the prediction of each marital quality measure (i.e., marital adjustment and marital satisfaction) on the psychological measures of SWL, stress, and depression. We found that marital adjustment predicted SWL (β = 0.44, p < 0.0001), stress (β = −0.29, p < 0.0001), and depression (β = −0.19, p = 0.008). Marital satisfaction also significantly predicted SWL (β = 0.40, p < 0.0001), stress (β = −0.27, p = 0.0002), and depression (β = −0.38, p < 0.0001). Thus, as marital adjustment and satisfaction increase, so does SWL, while stress and depression decrease.
Marital Status, Marital Quality, and Ambulatory Blood Pressure
We next examined the impact of marital status on ABP. We found no differences between single and married individuals in 24-h or waking SBP or DBP (p’s > 0.05). However, we found a significant effect of marital status on nocturnal SBP [F(5,251) = 6.26, p < 0.01] and DBP [F(5,251) = 5.70, p < 0.05] dipping. SBP and DBP dipping was lower among single than married individuals (see Fig. 1).
We next performed separate regression analyses to examine if each of the marital quality measures (i.e., marital adjustment and satisfaction) predicts 24-h, waking, and nocturnal dipping of SBP and DBP. Marital adjustment significantly predicted 24-h (β = −0.16, p = 0.02) and waking (β = −0.15, p = 0.03) SBP. Likewise, marital satisfaction significantly predicted 24-h (β = −0.20, p = 0.005) and waking SBP (β = −0.19, p = 0.006). Neither marital adjustment nor satisfaction significantly predicted nocturnal SBP dipping, nor did either predict 24-h waking or nocturnal dipping of DBP (p’s > 0.05). Overall, as marital adjustment and satisfaction increase, 24-h and waking ambulatory SBP decrease.Footnote 3
Is a Bad Marriage Better or Worse than No Marriage?
To examine this question, we compared single individuals with married individuals whose MAT scores fell below the median (108.5).Footnote 4 Using this criterion, the previously significant difference between married and single individuals on SBP and DBP dipping were no longer significant (p = 0.11, p = 0.13, respectively). We also found a significant difference between single and lower MAT scoring married persons on 24-h [F(3,193) = 8.35, p < 0.001] and waking [F(3,193) = 11.65, p = 0.001] SBP as well as significant differences on 24-h DBP [F(3,193) = 6.30, p = 0.01] and waking DBP [F(3,193) = 9.64, p = 0.002]. Those with lower quality marriages had significantly higher SBP and DBP than those who are unmarried (see Fig. 2).
We also compared single individuals with married individuals low in marital satisfaction (below the median = 20). We found a significant difference between married individuals who reported lower marital satisfaction and single individuals on 24-h [F(3,174) = 3.94, p < 0.05] and waking SBP [F(3,174) = 6.47, p = 0.01]. Those with less satisfying marriages had significantly higher 24-h (m = 118.19) and waking (m = 120.49) SBP than single participants (m = 114.99, m = 116.31). There was no significant difference on ambulatory DBP. Thus, being married is not advantageous if the marriage is of poor quality.Footnote 5
Does a Supportive Network Compensate for the Negative Effects of Being Single or a Low-Quality Marriage?
To answer this question, we followed the steps detailed to test for cross-domain buffering [11]. The social support, marital status, and marital quality variables were entered hierarchically to determine the relative contributions of each in predicting changes in ABP. Following the main effect terms, the cross-products of the centered predictors (social support × marital status, social support × marital adjustment, and social support × marital satisfaction) were calculated and entered into the regression to test for cross-domain buffering. We found no statistically significant interactions for 24-h, waking, or dipping of ambulatory SBP or DBP (p’s > 0.05). Thus, network support did not buffer the ABP effects of being single or unhappily married.
Discussion
This study examined the relative impact of marital status, relationship quality, and network support on ABP and their associated implications for cardiovascular disease and mental health. Consistent with prior research indicating that marriage carries health benefits, we found that married individuals report being more satisfied with life and have greater BP dipping than unmarried individuals. When we examined marital quality, we found that marital adjustment and satisfaction significantly predict SWL, stress, depression, and ambulatory SBP (24-h and waking). Overall, our findings indicate that both marital status itself and the quality of a marriage are important. However, when we directly contrasted single individuals with individuals in low-quality marriages, the difference in BP dipping disappeared. Single individuals actually had lower 24-h and waking ABP compared to those in unhappy marriages. Therefore, marriage must be of a high quality to be advantageous. In other words, one is better off single than unhappily married.
The second aim of this study was to examine whether a supportive network could compensate for being unmarried or in a low-quality marriage. Given prior research suggesting that perceptions of support and number of supportive network ties are associated with health benefits [1, 2] and evidence of a cross-domain buffering effect [11], we expected to find similar benefits among single persons and those in a low-quality marriage. However, we found no evidence that a supportive network buffered the effects of an unhappy marriage or being unmarried. In fact, follow-up analyses among single persons reveal that even those with higher than average network support experienced significantly decreased BP dipping compared to their married counterparts [F(3,131) = 3.74, p < 0.05]. These findings suggest that the spousal relationship may be more influential than other relationships. This influence may be due to greater commitment (presumably life-long), importance, investment, and/or intimacy within marriage relative to other relationships; however, further research will be needed to systematically examine potential mechanisms.
These findings complement and build upon prior research. They corroborate other research findings that relationship quality and satisfaction is linked to lower ABP [32]. The current study extended such findings by directly contrasting groups at greater risk (i.e., unhappily married and unmarried) on measures that inform physical health and addresses an important potential moderating effect of prior results—that a supportive social network may buffer negative effects for groups at greater risk. This study also provides further clarification of the psychophysiological consequences of social relationships. ABP appears to be a strong predictor of future cardiovascular disorders [19]. Chronic, even minor, elevations in BP may place a greater strain on the system and lead to greater cardiovascular risk [20, 21, 33]. If the psychological and physiological effects of marital status and quality are reliable, presumably, exposure would be chronic and would have implications for well-being. However, longitudinal studies, among both normotensive and hypertensive samples, are needed to clarify the long-term health significance.
We also acknowledge potential limitations to this study. First, we sampled over only 1 day. Second, our sample was predominantly white and educated. In addition, we examined only legally married heterosexual couples, making our non-married sample very broadly defined. It is unclear to what extent homosexual, cohabitating, and/or dating couples differ from those not in a romantic relationship. It is also unclear whether there is a difference between individuals who are single by choice versus circumstance and if there are differences among single persons who are divorced, widowed, or never married. Likewise, we did not specifically sample clinically distressed couples. Finally, we utilized a cross-sectional design among a mostly young and healthy population.
Overall, we believe that these findings have important implications. This study suggests that marriage may provide some protective effects; however, the quality of the marriage also matters. Importantly, single individuals are not uniformly disadvantaged, as they showed some advantages over those in low-quality marriages. Still, there does appear to be something unique about the spousal relationship, as other relationships did not compensate for the lack of a satisfying marriage. While our marital status and marital quality findings are consistent with prior research and theory, the implications of our findings for single individuals are less understood. It is hoped that these findings may help guide theory and further systematic research on the psychological, behavioral, and physiological consequences (both positive and negative) of the growing demographic of single persons. Our findings also underscore an important aim for further research among married persons—whether marital therapy or improvements in the quality of marriage over time can lead to improvements in health outcomes. Overall, these results highlight the complexities in understanding the influence of social relationships on health and may help clarify one potential physiological pathway by which such associations exist.
Notes
Unmarried participants included 12 that were divorced and 1 was widowed. Analyses were repeated dropping these 13 individuals, and our findings were consistent with what is reported.
Gender was found to significantly predict 24-h and waking SBP. We found no interactions effects between marital status or quality and gender for any of our primary DVs (p > 0.05).
Pre-hypertensive status did not interact with either marital status or quality on ABP.
This median split also corresponds well with validity data [23] indicating that 96% of well-adjusted couples had scores above 100 and the 83% of maladjusted couples had scores below 100.
This finding was moderated by pre-hypertensive/normotensive status such that the effect was strongest among pre-hypertensives. When comparing unmarried to happily married (above the median for MAT and satisfaction) individuals, results were consistent with the overall marital status findings.
References
Berkman LF. The role of social relations in health promotion. Psychosom Med. 1995; 57: 245–254.
House JS, Landis KR, Umberson D. Social relationships and health. Science. 1988; 241: 540–545.
Johnson NJ, Backlund E, Sorlie PD, Loveless CA. Marital status and mortality: The National Longitudinal Mortality Study. Ann Epidemiol. 2000; 10: 224–238.
Gove WR, Hughes M, Style Briggs C. Does marriage have positive effects on psychological well-being of the individual? J Health Soc Behav. 1983; 24: 122–131.
Robins L, Regier D. Psychiatric disorders in America. New York: Free Press; 1991.
Friedman HS, Tucker JS, Schwartz JE, et al. Psychosocial and behavioral predictors of longevity: the aging and death of the “Termites”. Am Psychol. 1995; 50: 69–78.
Ross CE, Mirowsky J, Goldsteen K. The impact of the family on health: the decade in review. J Marriage Fam. 1990; 52: 1059–1078.
Coyne JC, Rohrbaugh MJ, Shoham V, et al. Prognostic importance of marital quality for survival of congestive heart failure. Am J Cardiol. 2001; 88: 526–529.
Gallo LC, Troxel WM, Matthews KA, Kuller LH. Marital status and quality in middle-aged women: associations with levels and trajectories of cardiovascular risk factors. Health Psychol. 2003; 22: 453–463.
Grewen KM, Girdler SS, Light KC. Relationship quality: effects on ambulatory blood pressure and negative affect in a biracial sample of men and women. Blood Press Monit. 2005; 10: 117–124.
Lepore SJ. Social conflict, social support, and psychological distress: evidence of cross-domain buffering effects. J Pers Soc Psychol. 1992; 63: 857–867.
Pearlin LI, McCall ME. Occupational stress and marital support: a description of microprocesses. In: Eckenrode J, Gore S, eds. Stress between work and family. New York: Plenum Press; 1990: 39–60.
Umberson D. Gender, marital status and the social control of health behavior. Soc Sci Med. 1992; 34: 907–917.
Robels TF, Kiecolt-Glaser JK. The physiology of marriage: pathways to health. Physiol Behav. 2003; 79: 409–416.
Burman B, Margolin G. Analysis of the association between marital relationships and health problems: an interactional perspective. Psychol Bull. 1992; 112: 39–63.
Perloff D, Sokolow M, Cowan R. The prognostic value of ambulatory blood pressure. JAMA. 1983; 249: 2793–2788.
Fallo F, Barzon L, Rabbia F. Circadian blood pressure patterns and life stress. Psychother Psychosom. 2002; 71: 350–356.
Verdecchia P, Schillaci G, Borgioni C, et al. Gender, day-night blood pressure changes, and left ventricular mass in essential hypertension: dippers and peakers. Am J Hypertens. 1995; 8: 193–196.
Ohkubo T, Imai Y, Tsuji I, et al. Relation between nocturnal decline in blood pressure and mortality. Am J Hypertens. 1997; 10: 1201–1207.
Ohkubo T, Hozawa A, Yamajuchi J, et al. Prognostic significance of the nocturnal decline in blood pressure in individuals with and without high 24-h blood pressure: The Ohasama Study. J Hypertens. 2002; 20: 2183–2189.
Verdecchia P, Schillaci G, Borioni C, et al. Nocturnal pressure is the true pressure. Blood Press Monit. 1996; 1: S81–S85.
Cacioppo JT, Malarkey W, Kiecolt-Glaser JK, et al. Heterogeneity in neuroendocrine and immune responses to brief psychological stressors as a function of autonomic cardiac activation. Psychosom Med. 1995; 57: 154–164.
Locke HJ, Wallace KM. Short marital-adjustment and predication tests: their reliability and validity. Marriage and Family Living. 1959; 21: 251–255.
Spanier GB. Measuring dyadic adjustment: new scales for assessing the quality of marriage and similar dyads. J Marriage Fam. 1976; 38: 15–28.
Cohen S, Hoberman HM. Positive events and social supports as buffers of life change stress. J Appl Soc Psychol. 1983; 13: 99–125.
Radloff SL. The CES-D Scale: a self-report depression scale for research in the general population. Appl Psychol Meas. 1977; 1: 385–401.
Diener E, Emmons RA, Larsen RJ. The Satisfaction With Life Scale. J Pers Assess. 1985; 49: 71–75.
Cohen S, Kamarck T, Mermelstein R. A global measure of perceived stress. J Health Soc Behav. 1983; 24: 385–396.
White WB, Lund-Johansen P, Omvik P. Assessment of four ambulatory blood pressure monitors and measurements by clinicians versus intraarterial blood pressure at rest and during exercise. Am J Cardiol. 1990; 65: 60–66.
Kamarck TW, Shiffman SM, Smithline L, et al. Effects of task strain, social conflict, and emotional activation on ambulatory cardiovascular activity: daily life consequences of recurring stress in a multiethnic adult sample. Health Psychol. 1998; 17: 17–29.
Marler MR, Jacob RG, Lehoczky JP, Shapiro AP. The statistical analysis of treatment effects in 24-hour ambulatory blood pressure recordings. Stat Med. 1988; 7: 697–716.
Baker B, Helmers K, O’Kelly B, et al. Marital cohesion and ambulatory blood pressure in early hypertension. Am J Hypertens. 1999; 12: 227–230.
MacMahon S, Peto R, Cutler J, et al. Blood pressure, stroke, and coronary heart disease. Part 1, prolonged differences in blood pressure: prospective observational studies corrected for the regression dilution bias. Lancet. 1990; 335: 765–774.
Acknowledgment
This research was generously supported by grants awarded to Dr. Julianne Holt-Lunstad from the Marchionne Foundation and the Family Studies Center at Brigham Young University.
Author information
Authors and Affiliations
Corresponding author
About this article
Cite this article
Holt-Lunstad, J., Birmingham, W. & Jones, B.Q. Is There Something Unique about Marriage? The Relative Impact of Marital Status, Relationship Quality, and Network Social Support on Ambulatory Blood Pressure and Mental Health. ann. behav. med. 35, 239–244 (2008). https://doi.org/10.1007/s12160-008-9018-y
Received:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12160-008-9018-y