Abstract
Purpose
This study evaluated the usefulness of SUV analysis of 99mTc-galactosyl human serum albumin (99mTc-GSA) scintigraphy including SUV analysis of the cardiac blood pool normalized by blood volume as a predictor of short-term survival in severe liver failure.
Patients and methods
We enrolled 24 patients with severe liver failure who underwent 99mTc-GSA scintigraphy and were admitted to the intensive care unit. Patients were divided into survival and non-survival groups at 7, 14, and 28 days from the performance of 99mTc-GSA scintigraphy. From SPECT images we calculated SUVs of the cardiac blood pool, performing normalization for body weight, lean body weight, Japanese lean body weight, and blood volume and we calculated SUVs of the liver, normalizing by body weight, lean body weight, and Japanese lean body weight. We also calculated the uptake ratio of the heart at 15 min to that at 3 min (HH15) and the uptake ratio of the liver at 15 min to the liver plus the heart at 15 min (LHL15) from planar images of 99mTc-GSA scintigraphy.
Results
There were significant differences between the 7 day survival and non-survival groups for all SUVs of the heart and the liver and HH15, for 14 day survival groups in SUVs of the heart normalized by Japanese lean body weight and blood volume, and no significant differences between 28 day survival groups for any SUVs, HH15, or LHL15. Although the difference was not significant, SUV analysis of the heart normalized by blood volume showed the highest value for the area under the receiver-operating-characteristics curve for both 7 day and 14 day survival.
Conclusion
SUV analysis of 99mTc-GSA including SUV analysis of cardiac blood pool normalized by blood volume is of value for prediction of short-term survival in cases with severe liver failure.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Liver failure is one of the most lethal factors in multiple organ dysfunction syndrome, and severe hepatic dysfunction sometimes requires admission to the intensive care unit [1,2,3,4]. The severity of critically ill patients with liver failure can be evaluated by the model for end-stage liver disease (MELD), which is useful for the prediction of 3 month survival [2,3,4,5]. On the other hand, we reported that findings of 99mTc GSA scintigraphy are of value for 28 day survival using the index of the uptake ratio of the heart at 15 min to that at 3 min (HH15) and the uptake ratio of the liver at 15 min to the liver plus the heart at 15 min (LHL15) [1]. But the usefulness of these indexes for survival for a very short term, i.e., within 28 days of scintigraphy, has not been sufficiently discussed. Thus, here we evaluated the usefulness of the MELD score and 99mTc GSA scintigraphy for 7 day, 14 day, and 28 day survival. We performed SUV analysis of the 99m-Tc GSA scintigram as well as analysis of the MELD score and HH15 and LHL15 indexes because of concerns that the latter two measurements require discrimination of the cardiac and liver regions on planar images, which is difficult to do (strong remnants of 99mTc GSA in the blood pool of the heart and less physiological accumulation in severely diseased livers). SUV analysis has been more prevalent on the clinical scene recently. Moreover, we evaluated the usefulness of SUV analysis of 99mTc-GSA scintigraphy including SUV analysis of the cardiac blood pool normalized by blood volume, which makes sense theoretically. There are significant differences between this report (ethics approval number 342–239) and the one published ten years ago investigating the usefulness of HH15 and LHL15 for 28 days survival (ethics approval number 24–5006); we evaluated survival for a shorter period and mainly evaluated SUV analysis, which is different index from HH15 or LHL15. Additionally, patients in the previous report were recruited from 1999 to 2006 and patients in this report were recruited from 2012 to 2023 without overlap of patients [1].
Patients and methods
Patients
This retrospective study was approved by our hospital’s institutional review board (ethics approval number 342–239), and the requirement for direct informed consent was waived. From May 2012 and February 2023 at our hospital, 99mTc-GSA scintigraphy including SPECT was performed in 25 patients with hepatic failure who had been admitted to the intensive care unit of our hospital. We excluded one patient because the patient was under 18 years old. Finally, we evaluated the remaining 24 cases. We calculated the MELD score using serum bilirubin, serum creatinine, and prothrombin time-international normalized ratio [5]. Patient characteristics are summarized in Table 1. For investigation of the prediction of short-term survival, we divided patients into survival (SV) and non-survival (NSV) groups at 7, 14, and 28 days from 99mTc-GSA scintigraphy.
99mTc-GSA scintigraphy
We performed Scintigraphy under providing intensive medical care accompanying by intensivist. SPECT/CT scans were obtained by a SPECT/CT scanner (Discovery NM/CT 670 pro, GE Healthcare, Tokyo, Japan) equipped with a 16-slice CT scanner for attenuation correction. We obtained dynamic planar images for 16 min after intravenous administration of 3 mg of 99mTc-GSA (185 MBq; Nihon Medi-physics Co, Ltd, Tokyo, Japan); then SPECT/CT images of the heart and liver were performed. The SPECT/CT scan was acquired using a low-energy high-resolution collimator, a 128 × 128 matrix with a 4.4 mm pixel size, and a total of 60 projections (30 steps) over 360° with a dwell time of 10 s/step. After the SPECT acquisition, a low-dose CT transmission scan was performed with 120 kV, 10 mA using a 512 × 512 matrix size. The CT data were generated with a 4.4 mm slice thickness.
Measurement of HH15 and LHL15
Indexes of HH15 and LHL15 were calculated on planar images [1, 6, 7]. We calculated the uptake ratio of the heart at 15 min to that at 3 min as HH15 and the uptake ratio of the liver at 15 min to the liver plus the heart at 15 min as LHL15. While the HH15 ratio reflects the rate of disappearance in blood, the LHL15 ratio reflects the rate of accumulation in the liver. A representative case is shown in Fig. 1.
Analysis of HH15 and LHL15 on planar image of the case with drug-induced liver failure (case 16). H3, radioactivity of the heart 3 min after injection of 99mTc-GSA; H15, radioactivity of the heart 15 min after injection of 99mTc-GSA; L15, radioactivity of the liver 15 min after injection of 99mTc-GSA; HH15, H15/H3; LHL15, L15/ (L1 + H15). Values for H3, H15, L15, HH15, and LHL15 were 27,402 counts/minute, 24,680 counts/minute, 76,026 counts/minute, 0.901, and 0.775, respectively
SUV measurement
Quantitative SPECT/CT parameters normalized by body weight were calculated using a commercial software package (GI-BONE, AZE Co., Tokyo) that is widely available in Japan. The measurements of SUVs of all 24 cases were performed by a nuclear physician who confirmed carefully the accuracy of the volume of interest while checking 3-plane images. The maximum and the peak SUV normalized by body weight (SUVbwmax and SUVbwpeak) were calculated for quantitative analysis of 99mTc-GSA uptake as follows: SUVbw = (tissue radioactivity/voxel volume)/(injected radioactivity/body weight), where ‘tissue radioactivity’ indicates the tissue radioactivity concentration measured by SPECT. The tissue radioactivity concentration was obtained by multiplying the SPECT counts and Becquerel calibration factor, which was determined by scanning a cylindroid phantom filled with a known radioactivity concentration. The following were also calculated: SUVbwmax = (max. radioactivity/voxel volume)/(injected radioactivity/body weight) and SUVbwpeak = (averaged radioactivity obtained within a 1 cm3 sphere of interest centered on the voxel of the SUVbwmax/voxel volume)/(injected radioactivity/ body weight).
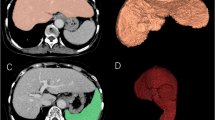
We determined the SUVbwmax and SUVbwpeak data of the blood-pool of the heart (SUVbwmaxH and SUVbwpeakH) and those of the liver (SUVbwmaxL and SUVbwpeakL). A representative case is shown in Fig. 2.
SUV analysis of the same patient as in Fig. 1. A–D Images for analysis of the heart. E–H Images for analysis of the liver. A, C, E, G A selected VOI over the MIP images of SPECT. Results of SUVbwmaxH, SUVbwpeakH, SUVbwmaxL, and SUVbwpeakL were 11.56, 10.77, 12.85, and 12.35, respectively
SUVs of both the heart and liver corrected by lean body weight (lbw) and Japanese lean body weight (jlbw), and blood volume (bv) based on the following equations were used to calculate normalized SUV variations:
Lean body weight, Japanese lean body weight, and blood volume were estimated as follows [8,9,10]:
Statistical analysis
We calculated the correlation of SUVbwmax versus SUVbwpeak of the heart and liver Spearman’s correlation test. For evaluation of patient characteristics, we compared age, body weight, and height between females and males using the Mann–Whitney U test. For the evaluation of results of the 99 m-GSA examination, the SUVs, HH15, LHL15, and MELD scores were compared between SV and NSV groups using the Mann–Whitney U test. In all analyses, a probability (p) value < 0.05 was accepted as significant. Receiver-operating characteristic (ROC) analyses were performed in categories with significant differences. The Youden index was used to determine the optimal cutoff values. Comparisons of the areas under the curve (AUCs) between several results were performed using the DeLong method [11]. Statistical analyses were performed using EZR software (Saitama Medical Center, Jichi Medical University, Saitama, Japan), the graphical user interface for R [12].
Results
The clinical characteristics of patients are shown in Table 1. There were no significant differences in age between the female and male groups, whereas sex-based differences in body weight and height were significant. SUVbw and survival status from 99mTc GSA scintigraphy of each of the 24 cases are shown in Table 2.
Correlations between the SUVmax and SUVpeak values
There were significant and strong correlations between the SUVbwmax and SUVbwpeak values of both the heart and the liver. The correlation coefficients were SUVbwmaxH vs. SUVbwpeakH, 0.993 (p < 0.00001), and SUVbwmaxL vs. SUVbwpeakL, 0.999 (p < 0.00001).
Comparison of SUVs between the SV and NSV groups, and the ROC analysis
Regarding 7 day survival, the SV and NSV groups showed statistically significant differences for all kinds of SUVs and for HH15 while LHL15 and the MELD score showed no significant difference (Table 3). Results of ROC analyses are shown in Table 4 and Fig. 3. Although there was no statistically significant difference among AUCs of all SUVs and HH15 by the DeLong method, the AUCs of SUVbvmaxH and SUVbvpeakH were higher than those of other SUVs or HH15.
Receiver-operating characteristic curve for prediction of 7-day survival (A–H), 14-day survival (I, J), and 28-day survival (K). HH15, uptake ratio of the heart at 15 min to that at 3 min; MELD, model for end-stage liver disease; SUVbvMaxH, maximum SUV of the heart normalized by blood volume; SUVbwMaxH, maximum SUV of the heart normalized by body weight; SUVbwMaxL, maximum SUV of the liver normalized by body weight; SUVjlbwMaxH, maximum SUV of the heart normalized by Japanese lean body weight; SUVjlbwMaxL, maximum SUV of the liver normalized by Japanese lean body weight; SUVlbwMaxH, maximum SUV of the heart normalized by lean body weight; SUVlbwMaxL, maximum SUV of the liver normalized by lean body weight
Regarding 14 day survival, the SV and NSV groups showed statistically significant differences in SUVjlbwmaxH, SUVjlbwpeakH, SUVbvmaxH, and SUVbvpeakH but did not show differences in other SUVs, HH15, LHL15, or MELD scores (Table 3). Results of ROC analyses are described in Table 4 and Fig. 3. Although there were no statistically significant differences among SUVs by the DeLong method, the AUCs of SUVbvmaxH and SUVbvpeakH were higher than those of SUVjlbwmaxH or SUVjlbwpeakH. Additionally, we performed a subanalysis of a comparison of 3 patients consisted of the NSV group excluding 6 patients of NSV for 7-day vs. 15 patients consisted of the SV group, and results did not show a significant difference in SUVjlbwmaxH (p = 0.91), SUVjlbwpeakH (p = 0.91), SUVbvmaxH (p = 1.00), or SUVbvpeakH (p = 1.00).
Regarding 28 day survival, the SV and NSV groups showed statistically significant differences in MELD scores, but not in any SUVs, HH15, or LHL15 (Table 3). Results of ROC analyses are shown in Table 4 and Fig. 3. Additionally, we performed subanalysis of a comparison of 6 patients consisted of the NSV group excluded of 6 patients of NSV for 7 day vs. 12 patients consisted of the SV group, and the results showed a significant difference (p = 0.02) in the MELD score.
Discussion
The results of this study revealed that our proposed method of analyzing the SUV of 99mTc-GSA is both simple and objective, requiring no specific imaging techniques or extensive experience in image interpretation; the analysis also showed sufficient value for the prediction of short-term survival in case of severe liver failure.
Estimating the prognosis of patients with severe liver failure is an important matter, and the MELD score is still the most widely used severity-of-liver disease scoring system; one benefit is that it can also be used in the field of intensive care [1, 13,14,15]. However, reports regarding the usefulness of the MELD score are limited, especially in intensive care medicine, and conditions with no possibility of recovery or prediction of short-term survival in case of severe liver failure needs further attention, given that intensive care for severely ill patient requires significant medical resources. Thus, we consider that our results of SUV analysis of 99mTc-GSA may become an important reference for appropriate use of medical resources with severe liver dysfunction [1]. Additionally, we recommend performing scintigraphy providing intensive care accompanying with an intensivist, because life-threatening event may occur during scintigraphy in the case of severe liver failure.
For evaluation of liver function, HH15 and LHL15 estimated from planar images of 99mTc-GSA scintigraphy have been widely employed in Japan, and many reports of their usefulness for preoperative evaluation for liver surgery, prognosis for liver failure, and evaluation of liver fibrosis severity have been published [1, 6, 7, 16,17,18,19,20]. But HH15 and LHL15 are considered less reproducible than other measures; the manner of setting the ROI of the heart and the liver for calculating HH15 and LHL15 differs among institutions, resulting in different absolute values [18, 19, 21]. On the other hand, SUV analysis of SPECT has come into wide use in clinical science worldwide and can provide higher inter- and intra-operator reproducibility [22, 23]. Thus, SUV analysis of SPECT images of 99mTc GSA scintigraphy has clear advantages over HH15 or LHL15 from planar images, and dynamic study of planar image may be omitted for reduction of the burden about intensive care during scintigraphy.
Especially in cases with severe liver failure, various factors can affect the measurement of HH15 and LHL15. Strong accumulation of the blood pool of the heart and less accumulation in the liver makes it difficult to set boundaries of the liver and the heart for placement of ROIs on a planar image, and the resulting ROIs counts are considered less reliable because of this overlap of heart and liver. On the other hand, SUV analysis using volumes of interest of the heart and liver on SPECT images with reference to the SPECT/CT image may be both easier and more reliable.
Moreover, we must pay attention to the mechanism of distribution of 99 m-Tc GSA especially in case of severe liver failure. Residual blood-pool accumulation in the vessels of the liver can prevent proper estimations of the physiological uptake of hepatocyte, and apparently stronger accumulation of the liver can be caused in cases with severe liver failure. Thus, we consider the SUV of residual blood-pool accumulation of the heart to be more reliable than the SUV of the liver; indeed, our results showed concordance with this hypothesis.
Several normalization methods for the SUV have been proposed, for example normalization by body weight, lean body weight, and body surface area [24, 25]. We developed a normalization of SUV by blood volume. We hypothesized that the SUV of the blood pool normalized by blood volume would be the best method for the evaluation of residual tracer in the blood pool theoretically. Although the results were not statistically significant in our small cohort, we were not surprised to find that the AUC of SUV analysis of the heart normalized by blood volume was higher than SUV analyses normalized by body weight, lean body weight, or Japanese lean body weight for prediction of 7 day survival and higher than that of Japanese lean body weight for 14 day survival.
As for the liver, we consider that the SUV of the liver should be normalized by liver volume or that total liver uptake would provide a more meaningful measure. However, in terms of applicability to intensive care settings, it is difficult to evaluate liver volume quickly in our SPECT/CT protocol; furthermore, evaluation of liver volume from SPECT images in the same manner as in the previous report is difficult in cases with severe liver failure due to strong accumulation of the blood pool around the liver [26,27,28]. Thus, we abandoned the search for an evaluation method for total liver uptake in the present work. Meanwhile, we are certain that the estimation of hepatic functional reserve using the Patlak plot method of 99mTc-GSA dynamic SPECT is more reliable [29, 30], and we consider that analysis of whole liver uptake of 99mTc-GSA including analysis of hepatic functional reserve is needed for evaluation of the liver.
Findings for 28 day survival were not significant for all SUVs, HH15, or LHL15, although our previous report showed significant differences for HH15 and LHL15 [1]. This discrepancy may be due to patient selection bias because we recruited fewer patients and those with more severe diseases in the present report than in the previous one. Further investigation with large-scale trials is needed, although recruitment of patients with severe liver failure may be difficult.
There are some study limitations to address. This was a retrospective analysis with a relatively small number of patients. Large prospective studies are needed to validate our results. Selection bias may have affected our results, as patients with different causes of liver failure were recruited in this report. Another selection bias is about severity. Patients of NSV for 7-day may have had a large impact on evaluation for 14 day and 28 day survival in this report.
In conclusion, the SUV analysis of 99mTc-GSA that we have described is of value for the prediction of short-term survival in patients with severe liver failure. Our results provide a foundation for the quantitative analysis of blood pool imaging using evaluation of SUV normalized by blood volume.
References
Tatsumi H, Masuda Y, Imaizumi H, Yoshida S, Goto K, Yama N, Mizuguchi T, Hirata K. Asialoglycoprotein receptor scintigraphy with 99mTc-galactosyl human serum albumin (99mTc-GSA) as an early predictor of survival in acute liver failure. Anaesth Intensive Care. 2013;41:523–8.
Wiesner R, Edwards E, Freeman R, Harper A, Kim R, Kamath P, Kremers W, Lake J, Howard T, Merion RM, Wolfe RA, Krom R. United network for organ sharing liver disease severity score committee. model for end-stage liver disease (MELD) and allocation of donor livers. Gastroenterology. 2003;124:91–6.
Kamath PS, Wiesner RH, Malinchoc M, Kremers W, Therneau TM, Kosberg CL, D’Amico G, Dickson ER, Kim WR. A model to predict survival in patients with end-stage liver disease. Hepatology. 2001;33:464–70.
Wiesner RH, McDiarmid SV, Kamath PS, Edwards EB, Malinchoc M, Kremers WK, Krom RA, Kim WR. MELD and PELD: application of survival models to liver allocation. Liver Transpl. 2001;7:567–80.
Malinchoc M, Kamath PS, Gordon FD, Peine CJ, Rank J, Ter Borg PC. A model to predict poor survival in patients undergoing transjugular intrahepatic portosystemic shunts. Hepatology. 2000;31:864–71.
Kwon AH, Ha-Kawa SK, Uetsuji S, Kamiyama Y, Tanaka Y. Use of technetium 99m diethylenetriamine-pentaacetic acid-galactosyl-human serum albumin liver scintigraphy in the evaluation of preoperative and postoperative hepatic functional reserve for hepatectomy. Surgery. 1995;117:429–34.
Shiomi S, Kuroki T, Kuriyama M, Takeda T, Nishiguchi S, Nakajima S, Tanaka T, Ochi H. Evaluation of fulminant hepatic failure by scintigraphy with technetium-99m-GSA. J Nucl Med. 1997;38:79–82.
Ito H, Ohshima A, Ohto N, Ogasawara M, Tsuzuki M, Takao K, Hijii C, Tanaka H, Nishioka K. Relation between body composition and age in healthy Japanese subjects. Eur J Clin Nutr. 2001;55:462–70.
James WPT. Research on obesity: a report of the DHSS/MRC group, department of health and social security / medical research council. London: HMSO; 1976.
Nadler SB, Hidalgo JH, Bloch T. Prediction of blood volume in normal human adults. Surgery. 1962;51:224–32.
DeLong ER, DeLong DM, Clarke-Pearson DL. Comparing the areas under two or more correlated receiver operating characteristic curves: a nonparametric approach. Biometrics. 1988;44:837–45.
Kanda Y. Investigation of the freely available easy-to-use software ‘EZR’ for medical statistics. Bone Marrow Transplant. 2013;48:452–8.
Lindvig KP, Teisner AS, Kjeldsen J, Strøm T, Toft P, Furhmann V, Krag A. Allocation of patients with liver cirrhosis and organ failure to intensive care: systematic review and a proposal for clinical practice. World J Gastroenterol. 2015;21:8964–73.
Levesque E, Hoti E, Azoulay D, Ichaï P, Habouchi H, Castaing D, Samuel D, Saliba F. Prospective evaluation of the prognostic scores for cirrhotic patients admitted to an intensive care unit. Levesque E J Hepatol. 2012;56:95–102.
Singh N, Gayowski T, Wagener MM, Marino IR. Outcome of patients with cirrhosis requiring intensive care unit support: prospective assessment of predictors of mortality. J Gastroenterol. 1998;33:73–9.
Shiomi S, Kuroki T, Enomoto M, Ueda T, Masaki K, Ikeoka N, Takeda T, Kobayashi K, Ochi H. Fulminant hepatic failure monitored by technetium-99m-DTPA-galactosyl-human serum albumin scintigraphy. J Nucl Med. 1996;37:641–3.
Suzuki Y, Kakisaka K, Sato T, Mikami R, Abe H, Sasaki T, Takikawa Y. Tc-99m GSA scintigraphy within the first 3 days after admission as an early predictor of outcome in severe acute liver injury. Sci Rep. 2021;11:12518.
Ogasawara G, Inoue Y, Itoh Y, Tagami S, Matsunaga K, Miki K. Improved reproducibility of simple quantitative indices from 99mTc-GSA liver functional imaging. Ann Nucl Med. 2013;27:487–91.
Nakajima K, Kinuya K, Mizutani Y, Hwang EH, Michigishi T, Tonami N, Kobayashi K. Simple scintigraphic parameters with Tc-99m galactosyl human serum albumin for clinical staging of chronic hepatocellular dysfunction. Ann Nucl Med. 1999;13:5–11.
Itano S, Sata M, Kumashiro R, Hirai K, Tanikawa K. Usefulness of technetium-99m-galactosyl human serum albumin liver scintigraphy for assessment of severity of alcoholic hepatitis. Alcohol Clin Exp Res. 1996;20(1 Suppl):86A-90A.
Koizumi M, Yamada Y, Nomura E, Takiguchi T, Kokudo N. An easy and reproducible semi-automatic method for the evaluation of 99mTc-galactosyl human serum albumin. Ann Nucl Med. 1997;11:345–8.
Ren C, Ren J, Tian Z, Du Y, Hao Z, Zhang Z, Fang W, Li F, Zhang S, Hsu B, Huo L. Assessment of cardiac amyloidosis with (99m)Tc-pyrophosphate (PYP) quantitative SPECT. EJNMMI Phys. 2021;8:3.
Dorbala S, Park MA, Cuddy S, Singh V, Sullivan K, Kim S, Falk RH, Taqueti VR, Skali H, Blankstein R, Bay C, Kijewski MF, Di Carli MF. Absolute quantitation of cardiac (99m)Tc-pyrophosphate using cadmium-zinc-telluride-based SPECT/CT. J Nucl Med. 2021;62:716–22.
Sarikaya I, Sarikaya A. Assessing PET parameters in oncologic (18) F-FDG studies. J Nucl Med Technol. 2020;48:278–82.
Kim CK, Gupta NC, Chandramouli B, Alavi A. Standardized uptake values of FDG: body surface area correction is preferable to body weight correction. J Nucl Med. 1994;35:164–7.
Tokorodani R, Sumiyoshi T, Okabayashi T, Hata Y, Noda Y, Morita S, Daisaki H, Okada Y, Yasuda E. Liver fibrosis assessment using 99mTc-GSA SPECT/CT fusion imaging. Jpn J Radiol. 2019;37:315–20.
Tokorodani R, Kume T, Daisaki H, Hayashi N, Iwasa H, Yamagami T. Combining 99mTc-GSA single-photon emission-computed tomography and Gd-EOB-DTPA-enhanced magnetic resonance imaging for staging liver fibrosis. Medicine (Baltimore). 2023;102: e32975.
Taniguchi M, Okizaki A, Watanabe K, Imai K, Uchida K, Einama T, Shuke N, Miyokawa N, Furukawa Hiroyuki. Hepatic clearance measured with (99m) Tc-GSA single-photon emission computed tomography to estimate liver fibrosis. World J Gastroenterol. 2014;20:16714–20.
Li XF, Taki J, Kinuya S, Higuchi T, Konishi S, Hwang EH, Shuke N, Nakajima K, Tonami N. Asialoglycoprotein receptor concentration in tumor-bearing livers and its fate early after their sectorial resection. Ann Nucl Med. 2003;17:489–93.
Hwang EH, Taki J, Shuke N, Nakajima K, Kinuya S, Konishi S, Michigishi T, Aburano T, Tonami N. Preoperative assessment of residual hepatic functional reserve using 99mTc-DTPA-galactosyl-human serum albumin dynamic SPECT. J Nucl Med. 1999;40:1644–51.
Funding
This research was supported by a research grant from Sapporo Medical University.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
Hiroomi Tatsumi received lecture fee from Otsuka Pharmaceutical Factory, Inc. The other authors have no potential conflicts of interest to report.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Yama, N., Tatsumi, H., Akatsuka, M. et al. Blood-pool SUV analysis of 99mTc-galactosyl human serum albumin (99mTc-GSA) normalized by blood volume for prediction of short-term survival in severe liver failure: preliminary report. Ann Nucl Med (2024). https://doi.org/10.1007/s12149-024-01975-9
Received:
Accepted:
Published:
DOI: https://doi.org/10.1007/s12149-024-01975-9