Abstract
Objective
When using perfusion only modified PIOPED II criteria for PE detection, generated non-diagnostic scans are found to be the main diagnostic restriction. The objective of current study is to identify the role of Wells criteria added to inconclusive readings with the intent of enhancing the lung scintigraphy diagnostic yield.
Methods
CTPA was performed in 34 suspected PE patients with inconclusive lung scintigraphy. They also were evaluated by Wells score and classified as low, intermediate and high probability. Overall prevalence and the rate of PE for each probability were calculated. Furthermore, NPV for scores < 2 and PPV for scores > 6 were computed.
Results
Having a mean age of 59.75 ± 17.38 years, 7 (20.6%), 23 (67.6%) and 4 (11.8%) of cases had total criteria point count < 2, 2–6 and > 6, respectively. Using CTPA, 5 patients (14.7%) were diagnosed with PE. None of the patients with scores < 2 had PE with an associated NVP of 100%. Patients with scores 2–6 had a PE rate of 4.3% and 100% of patients with scores > 6 were diagnosed with PE, implying that the PPV of scores > 6 was 100%.
Conclusion
Adding Wells score to non-diagnostic scans allowed identification of PE to be done reliably, and provided further insight into how lung scintigraphy in conjunction with clinical assessment is a practical strategy not only for the patients unfit for performing CTPA but also in all the patients referred for PE evaluation.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
The emphasis of reliable detection of pulmonary embolism as an established serious cause of mortality and morbidity is plainly visible [1]. A clinical assessment of the probability of PE using approved system such as wells score is a crucial step but it cannot definitely confirm a diagnosis of PE [2]. High accuracy, wide availability, and ability to exclude other pathologies have made computed tomography pulmonary angiography (CTPA) as the first-line imaging method in the daily clinical practice for suspected PE patients [3, 4]. However, as well as high cost of CTA and its usage limitation in patients with contraindications to iodinated contrast material, high radiation burden has been recently recognized as a major public health issue [3, 5, 6]. Yet, the trend is clearly toward safer approach in a way that CTPA would be performed just in selected patients. With the magnitude of lung scintigraphy having been truly understood [7,8,9]; the accuracy has been improved day after day by refining diagnostic criteria [11]. In perfusion only modified PIOPED II classification, this was achieved by reducing the number of non-diagnostic categories (potential conflict in the lung scintigraphic evaluations) to 20.6% [12]. Besides that, omitting ventilation scan has substantially decreased the amount of received radiation dose [9]. Finding trustworthy diagnostic pathways for reassessment of the subgroup with inconclusive results can develop the validity of scintigraphy [12]. Furthermore, introducing such a reliable approach by reducing the number of unnecessary CTPA is likely to make significant decrease in the cost and risk imposed to the suspected patients with PE [6]. The aim of the present investigation is to ascertain the significance of added Wells score as a robust clinical tool [13, 14] to non-diagnostic results derived from perfusion only modified PIOPED II criteria so as to eventually introduce more secure diagnostic approach in patients with suspected pulmonary embolism.
Materials and Methods
This study was carefully conducted in the nuclear medicine and radiology departments of Farshchian heart center between 2018 and 2019 on the patients with suspected PE. The study was approved by the university ethics committee. The age, sex and referral cause of each patient referred to nuclear department of Farshchian hospital in this time interval for PE evaluation were recorded. This was followed by a clinical assessment to complete the Wells score which was done prospectively for all the patients by the nuclear physicist just before the scintigraphy. Components of the Wells score [15] are shown in Box 1. The findings of CXR, taken at the same day, were documented as well. Every patient, then, underwent lung perfusion scintigraphy immediately after intravenous injection of 3 mCi of Tc-99m macroaggregated albumin. Planar static images of perfusion of the lung were acquired in six identical projections using a rotating, dual head gamma camera (Symbia T2, Siemens Healthcare) equipped with a low-energy high-resolution parallel whole collimator. Lung perfusion scans in conjunction with CXR findings were thereafter read by an experienced nuclear physician, who had performed the clinical assessment of the included patients. The scan was reported as PE present, PE absent and non-diagnostic reading according to the perfusion only modified PIOPED II criteria [9] shown in box 2. Finally, the patients with non-diagnostic reading and without contraindications to iodinated contrast material (having a history of allergy to contrast media and/or renal dysfunction: estimated Glomerular Filtration Rate, GFR < 30 ml/min/1.73 m2) were included in the study and referred to radiology department for further evaluation with CTPA. CT scanning was performed using a 128-slice CT device (Definition AS, Siemens Medical Solutions, and Forchheim, Germany) and thorax CT angiography protocol after injection of contrast material at the speed of 3 ml/s. MSCT parameters were 300 ms rotation time, 128 × 0.6 mm collimation and 1 mm slice width, and pitch value was 1.0–1.2. The CTPA studies were reported by an expert radiologist as positive or negative PE based on diagnostic criteria. The numerical variables are presented as mean ± standard deviation. They were also shown as median, minimum and maximum values if necessary, and the categorical variables were summarized by raw frequencies and percentages. The rate of PE in this study was determined according to the different Wels score intervals (< 2, 2–6 and > 6). The negative predictive value (NPV) for scores < 2 and positive predictive value (PPV) for scores > 6 were calculated. Fisher's exact test was also used to compare the distribution of computed tomography findings between patients diagnosed and not diagnosed with PE. For the statistical analyses, the statistical software SPSS version 16.0 for Windows (SPSS Inc, Chicago, IL) was applied. All of the P values were 2-tailed, with statistical significance defined by P value ≤ 0.05.
Results
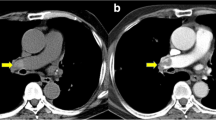
During the period of the study, 153 patients with suspected PE were referred to nuclear medicine department of Farshchian hospital. The prevalence of PE in the sample was 22 of 153 (14.37%) using the perfusion only modified PIOPED II, whereas 38 patients were reported as non-diagnostic scintigraphic reading. Having contraindication to CTPA, 4 patients could not be investigated by CTPA and were excluded from the study. Finally, 34 patients perfuming CTPA were credited for the analysis tests. The patients had a mean age of 59.75 ± 17.38 years ranging from 29 to 91 years with a male-to-female ratio of 22: 12. The number of patients referred as inpatients, outpatients and from the emergency department were 14 (41%), 8 (24%) and 12 (35%), respectively. The most common clinical presentations were shortness of breath (SOB) in 33 (97.1%), chest pain in 20 (58.8%), cough in 6 (17.6%), leg pain or swelling in 5 patients (14.7%), and hemoptysis in 3 patients (8.8%). Demographic and clinical characteristics of the study population are represented in Table 1. Recent immobilization in 11 patients (32 0.5%) and previous deep venous thrombosis (DVT) in 5 ones (14.7%) were noted. None of the patients had a history of malignancy (0%). While normal CXR was observed in 12 patients, the most frequently described findings in abnormal reported CXR were consolidation (31. 8%), atelectasis (22.72%), and pleural effusion (18.1%). In the study population, 7 (20.6%), 23 (67.6%) and 4 (11.8%) of cases had total criteria point count < 2, 2–6 and > 6, in the order given. The total criteria point count categorized for the study population as well as patients with positive CTPA result for PE have been shown in Table 2. Means calculated wells score was 3.75 with minimum and maximum values equal to 0 and 9, respectively. The CTPA ruled out the diagnosis of PE in 29 (85.3%) and confirmed pulmonary embolism in 5 patients (14.7%), all with sub-segmental branches involved. None of the patients with scores < 2 had pulmonary embolism with an associated NVP of 100%. Patients with scores 2–6 had a PE rate of 4.3% and 100% of patients with scores > 6 were diagnosed with PE, implying that the PPV of scores > 6 was 100% ( Fig. 1). The most common computed tomography findings in the cases not diagnosed with PE were pulmonary artery dilation (24.13%) and consolidation (20.6%). The distribution of CT findings of cases diagnosed and not diagnosed with PE has been introduced in Table 3. In patients with Wells score above 6, the male-to-female number ratio was 4:1; however, overall, the significant relationship between sex and Wells score was not found. When it comes to diameter measurement of main pulmonary artery—although all the patients with proved pulmonary embolism on CTPA had a PA diameter of 29 mm or more—there was no significant correlation between increased PA diameter and diagnosis of acute pulmonary embolism.
Discussion
Thanks to amazing technological advancements occurred in the field of pulmonary computed tomography angiography (CTPA), this practice is brought up as the modality of choice in suspected acute PE [3,4,5]. However, CTA is an expensive practice and may result in complications in patients who have reduced renal function or iodine allergy [5, 6]. Furthermore, based on recently suggested diagnostic pathways, when CTA result is inconclusive or discordant with the clinical risk assessment, further imaging tests such as scintigraphy may be required [12, 15]. Eventually, the rapidly increasing frequency of CTA usage has raised concern about the radiation exposure of the population, particularly radiation of the female breast [16, 17]. CTPA delivers a minimum radiation dose of 20 mGy to each breast in an average-sized woman, 50–80 mSv depending on coronary CTA protocol, and as many as 190 mGy with CTA in a woman with large breasts. Owing to the risk of cancer after such an exposure to radiation, another imaging test with lower doses may be indicated, especially in younger women. Breast irradiation with V/Q scintigraphy is found to be less than 5% of the radiation dose to the breast resulting from CTA, approximately 0.28–0.9 mGy [12]. It is more relevant if follow-up studies require evaluating recovery of pulmonary perfusion over time, or in patients likely to have recurrent clinical episodes of Pulmonary Emboli. Indeed, it is hypothesized that this risk is further increased in pregnancy due to increased radio sensitivity of the proliferating breast tissue [19]. To the best of our knowledge, this survey is the first to evaluate the utility of applying the wells score to inconclusive only perfusion modified PIOPED II results so as to improve the diagnostic yield of lung scintigraphy as a more secure test in the diagnosis of acute PE. Lung scintigraphic interoperation criteria have been redefined over time so as to enhance its diagnostic yield in the field of pulmonary embolism detection [9,10,11, 20]. Comparing with previous algorithms for V/Q scan reporting, modified PIOPED II criteria has been found to truly define most patients to PE present and PE absent with high sensitivity and specificity [11, 12]. When using this algorithm, further imaging test is warranted in just small number of patients with non-diagnostic results (20.6%) [12]. Our investigation revealed that adding Wells score < 2 to non-diagnostic readings in perfusion only modified PIOPED II interpretation system can rule out PE with NPV to 100% and consequently, patients who without any need to additional evaluation are reliably identified. On the other hand, 100% of inconclusive readings along with Wells score above 6 were diagnosed as pulmonary embolism by CTPA. Only one patient with wells score between 2 and 6 (4.3%) was diagnosed as Pulmonary Embolism on CTPA. The only patient with intermediate score (4.5) and pulmonary embolism was a 78- year-old man hospitalized because of heart failure and lower—extremity edema. The patient had the documented history of pulmonary embolism dating back to 5 years ago. After the patient being evaluated by CTPA, signs of acute and chronic pulmonary embolism were appeared simultaneously. Previously, Sostman et al. found substantial agreement between CTPA results and perfusion only modified PIOPED II interpretations for detection of PE; in their study, the sensitivity of a “PE present” perfusion scan was 84.9% and the specificity of "PE absent "was 92.7%, excluding "nondiagnostic" results [12]. Accordingly, with inconclusive results being excepted, perfusion scintigraphy combined with chest radiography could provide diagnostic accuracy similar to both CTA and ventilation–perfusion scintigraphy, at lower cost and with lower radiation dose [20].Our findings is momentous in terms of management of patients with inconclusive lung scintigraphic result who have contraindication for further radiological evaluation. Therefore, by this approach, later appropriate therapeutic strategies could be selected safely. Our findings add confirmation to the strong nature of Wells score in identifying the patients with high probability of pulmonary embolism. The strength of Wells score in management of suspected PE patients had been previously understood [14]so that wells score < 2 with a high NPV (> 95%) can reliably rule out PE but in Wells score above 2, other diagnostic imaging tests are obligatory, therefore, just 67% of patients with wells score above 6 revealed PE in their CTPA examination. Such a beneficial role of combination of clinical assessment system with other diagnostic test has been truly understood [2, 22]. Our study suffers a small sample size, may be due to referral of most suspected PE patients to the Department of Radiology for going under CTPA procedure as the first-line imaging modality. With respect to our findings, exerting Wells score to non-diagnostic reading, which occurs just in 20.6% modified PIOPED II criteria [12], can solve the main problem of declining usage of lung perfusion scan appearing in recent years. If other studies with larger sample size confirm these findings, this algorithm may replace the routine use of CTPA as a first line in PE detection (Tables 4, 5).
Conclusion
The summery of current study concluded that applying wells score to inconclusive only perfusion modified PIOPED II readings could appropriately reclassify the patients; as a result, PE was excluded in patients with Wells score below 2 and confirmed in Wells score above 6. According to these valuable findings, using Wells score in combination with only perfusion modified PIOPED II interpretation system seems to be reliable diagnostic strategy both for the patients inappropriate for performing CTPA and in all the patients needing PE evaluation and it is likely to replace the routine use of CTPA in PE detection.
References
Dalen JE. Pulmonary embolism: what have we learned since Virchow? Natural history, pathophysiology, and diagnosis. Chest. 2002;122(4):1440–566.
Wells PS, Ginsberg JS, Anderson DR, Kearon C, Gent M, Turpie AG, et al. Use of a clinical model for safe management of patients with suspected pulmonary embolism. Ann Intern Med. 1998;129(12):997–1005.
Escalon JG, Green DB, Bang TJ, Vargas D. Imaging pulmonary embolic disease. Curr Pulmonol Rep. 2019;8(3):104–11.
Konstantinides SV, Torbicki A, Agnelli G, Danchin N, Fitzmaurice D, Galiè N, et al. 2014 ESC guidelines on the diagnosis and management of acute pulmonary embolism. Eur Heart J. 2014;35(43):3033–69.
Albrecht MH, Bickford MW, Nance JW Jr, Zhang L, De Cecco CN, Wichmann JL, et al. State-of-the-art pulmonary CT angiography for acute pulmonary embolism. AJR Am J Roentgenol. 2017;208(3):495–504.
Mamlouk MD, vanSonnenberg E, Gosalia R, Drachman D, Gridley D, Zamora JG, et al. Pulmonary embolism at CT angiography: implications for appropriateness, cost, and radiation exposure in 2003 patients. Radiology. 2010;256(2):625–32.
Da Silva R, Shah M, Freeman LM. Ventilation-perfusion (V/Q) lung scintigraphy: a long journey to a renewed position of prominence in diagnosing pulmonary embolism. Clin Transl Imaging. 2014;2(5):369–78.
Poulose KP, Reba RC, Gilday DL, Deland FH, Wagner HN. Diagnosis of pulmonary embolism. A correlative study of the clinical, scan, and angiographic findings. Br Med J. 1970;3(5714):67–71.
Parker JA, Coleman RE, Grady E, Royal HD, Siegel BA, Stabin MG, et al. SNM practice guideline for lung scintigraphy 40. J Nucl Med Technol. 2012;40(1):57–655.
Freitas JE, Sarosi MG, Nagle CC, Yeomans ME, Freitas AE, Juni JE. Modified PIOPED criteria used in clinical practice. J Nucl Med. 1995;36(9):1573–8.
Stein PD, Woodard PK, Weg JG, Wakefield TW, Tapson VF, Sostman HD, et al. Diagnostic pathways in acute pulmonary embolism: recommendations of the PIOPED II investigators. Am J Med. 2006;119(12):1048–55.
Sostman HD, Miniati M, Gottschalk A, Matta F, Stein PD, Pistolesi M. Sensitivity and specificity of perfusion scintigraphy combined with chest radiography for acute pulmonary embolism in PIOPED II. J Nucl Med. 2008;49(11):1741–8.
Yap KS, Kalff V, Turlakow A, Kelly MJ. A prospective reassessment of the utility of the Wells score in identifying pulmonary embolism. Med J Aust. 2007;187(6):333–6.
Sherk WM, Stojanovska J. Role of clinical decision tools in the diagnosis of pulmonary embolism. AJR Am J Roentgenol. 2017;208(3):W60–W70.
Wells PS, Anderson DR, Rodger M, Ginsberg JS, Kearon C, Gent M, et al. Derivation of a simple clinical model to categorize patients probability of pulmonary embolism: increasing the models utility with the SimpliRED D-dimer. Thromb Haemost. 2000;83(3):416–20.
Parker MS, Hui FK, Camacho MA, Chung JK, Broga DW, Sethi NN. Female breast radiation exposure during CT pulmonary angiography. AJR Am J Roentgenol. 2005;185(5):1228–333.
Niemann T, Nicolas G, Roser HW, Müller-Brand J, Bongartz G. Imaging for suspected pulmonary embolism in pregnancy-what about the fetal dose? A comprehensive review of the literature. Insights Imaging. 2010;1(5–6):361–72.
Harris BS, Bishop KC, Kuller JA. Radiologic aspects of the diagnosis of pulmonary embolism in pregnancy. Clin Obstet Gynecol. 2018;61(2):219–27.
Easther S, Langdana F, Beasley R, Maharaj D, Entwisle J, Abels P. The diagnostic role of ventilation/perfusion scans versus computed tomography pulmonary angiography in obstetric patients investigated for pulmonary embolism at Wellington Hospital from 2010 to 2012. N Z Med J. 2016;129(1433):62–8.
Cronin P, Dwamena BA. A clinically meaningful interpretation of the prospective investigation of pulmonary embolism diagnosis (PIOPED) scintigraphic data. Acad Radiol. 2017;24(5):550–62.
Waxman AD, Bajc M, Brown M, Fahey FH, Freeman LM, Haramati LB, et al. Appropriate use criteria for ventilation-perfusion imaging in pulmonary embolism: summary and excerpts. J Nucl Med. 2017;58(5):13–5.
Malek MM, Adimi P, Seyedi SR, Sharif-Kashani B. Assessment of wells criteria in patients with pulmonary embolism. Tanaffos. 2008;7(2):50–3.
Gruettner J, Walter T, Lang S, Meyer M, Apfaltrer P, Henzler T, et al. Importance of wells score and Geneva score for the evaluation of patients suspected of pulmonary embolism. Vivo. 2015;29(2):269–72.
Slattengren AH, Prasad S, Bury C, Dickman M, Bennett N, Smith A, et al. PURL: a better approach to the diagnosis of PE. J Fam Pract. 2019;68(5):286–95.
Turan O, Turgut D, Gunay T, Yilmaz E, Turan A, Akkoclu A. The contribution of clinical assessments to the diagnostic algorithm of pulmonary embolism. Adv Clin Exp Med. 2017;26(2):303–9.
Wolf SJ, McCubbin TR, Feldhaus KM, Faragher JP, Adcock DM. Prospective validation of wells criteria the evaluation of patients with suspected pulmonary embolism. Ann Emerg Med. 2004;44(5):503–10.
Acknowledgements
We would like to thank Afshin Rezapour for careful editing the manuscript.
Author information
Authors and Affiliations
Corresponding author
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Hadei, S.K., Alvandi, M., Ramezani, M. et al. Applying Wells score to inconclusive perfusion only modified PIOPED II (Prospective Investigation of Pulmonary Embolism Diagnosis II) readings in order to optimize the lung scintigraphy diagnostic yield in acute pulmonary embolism detection. Ann Nucl Med 34, 521–526 (2020). https://doi.org/10.1007/s12149-020-01478-3
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12149-020-01478-3