Abstract
Objective
The aim of this study was to estimate radiation exposure and evaluate the risks and benefits of 18F-fluorodeoxyglucose positron emission tomography (FDG-PET) in cancer screening.
Methods
A nationwide survey of FDG-PET cancer screening was conducted in 2006, and the results were analyzed with a common index, “extension/shortening of the average life expectancy.”
Results
The average estimated effective dose was 4.4 mSv (male 4.7 mSv; female 4.0 mSv) for dedicated PET and 13.5 mSv (male 14.2 mSv; female 12.8 mSv) for PET/computed tomography (CT). The risk–benefit break-even age from the viewpoint of radiation exposure was in the 40s for men and 30s for women for dedicated PET and in the 50s for men and 50s (variable injection dose) or 60s (constant injection dose) for women for PET/CT.
Conclusions
FDG-PET cancer screening is beneficial for examinees above the break-even ages. The risks and benefits should be explained to examinees because of the larger radiation used in cancer FDG-PET screening compared with other X-ray tests.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
In Japan, cancer screening that uses 18F-fluorodeoxyglucose (FDG) positron emission tomography [PET; including positron emission tomography and computed tomography (PET/CT)] is widespread. Cancer screening is performed for an asymptomatic population and is beneficial for undetected cancer patients. However, the detection rate is extremely low from an epidemiologic standpoint because a vast majority of screening subjects does not have cancer. The benefit of cancer screening may be extremely small for the healthy population relative to the risk of radiation exposure that accompanies the screening. Therefore, the benefits and risks should be quantitatively evaluated. To date, the results of some types of cancer screening have been analyzed to estimate the benefits and risks of radiation exposure using extension/shortening of the average life expectancy as an index [1–4]. However, no evaluation has been conducted based on the field research of FDG-PET cancer screening.
When dedicated PET is used, external radiation exposure attributable to FDG-PET cancer screening with a 68 Ge-Ga transmission source is very small, and most of the radiation exposure is internal exposure by FDG. However, when PET/CT is used, the exposure dose is larger than the other cancer screenings that use X-rays, such as CT lung cancer screening and mammography, because external exposure increases with the use of CT. Therefore, a risk–benefit evaluation of radiation exposure in FDG-PET cancer screening is essential to judge the effectiveness of this cancer-screening method.
The Japanese Society of Nuclear Medicine and Clinical PET Promoting Committee published the “Guidelines of FDG-PET Cancer Screening” [5] in 2004, with the aim of evaluating the effectiveness of FDG-PET cancer screening and maintaining test quality. This guideline requests that institutions with PET installed be field surveyed and that the results of FDG-PET cancer screening at each institution be reported every year. The cancer-screening methods, such as the CT scanning parameters, are included in this yearly investigation. The effectiveness of FDG-PET for cancer screening can be evaluated using a risk–benefit analysis of radiation exposure based on the field data obtained from these PET-installed institutions.
Therefore, the aims of this study were to demonstrate the actual status of radiation exposure in FDG-PET screening on the basis of the field survey data and further evaluate the risk of radiation exposure in FDG-PET cancer screening and the benefit of cancer detection using extension/shortening of the average life expectancy as an index.
Materials and methods
Subject for investigation
Questionnaires regarding the actual situations and results of FDG-PET cancer screening were sent to 156 PET-installed facilities that registered at the PET Summer Seminar Meeting in 2006. Questions regarding radiation exposure included the name of the PET or PET/CT scanner, FDG injection method (constant or variable by weight), FDG injection radioactivity (MBq or MBq/kg), and CT scanning parameters (kV, mAs as product of X-ray tube current and rotation time, pitch factor, CTDIvol, and scan range). The estimated radiation exposure doses were calculated on the basis of these data.
Calculation of radiation exposure
Values from the International Commission on Radiological Protection (ICRP), Publication 80 [6] (Table 1), were used to calculate the internal radiation exposure dose by FDG. A 68 Ge-Ga source used for transmission scan by a dedicated PET emits slight radiation equivalent to approximately 0.01 mSv of external exposure per scan. This radiation dose is extremely small compared with internal exposure to FDG; therefore, it was not taken into account in the present study. External exposure in a CT scan was calculated using ImPACT simulation software [7, 8]. Radiation exposure may vary depending on the physique of each subject because the radioactivity of FDG injected may vary by weight, and the CT tube current can be controlled using CT-auto exposure control (CT-AEC). Therefore, the radiation exposure dose was calculated similarly to the dose assessment model (men 170 cm, 70 kg; women 160 cm, 55 kg) prescribed in ICRP Publication 23 [9].
Risk–benefit analysis
A risk–benefit analysis was performed using radiation exposure dose data obtained from the questionnaires. The mean value of each index was used for evaluation because variations in radiation exposure dose differ by facility. The risk–benefit analysis of FDG-PET cancer screening followed the Murano method [4]. ICRP calculation software was used [10] for risk calculation. The shortened period Si(u 0) from the average life expectancy of a structure (organ/tissue) (i) due to exposure to the equivalent dose D H at age u 0 was calculated, and Si(u 0) values for all structures exposed to radiation were added to obtain the total shortened period S(u 0) of the average life expectancy. The formulas are shown below:
\( \left( {\frac{{{\text{d}}p}}{{{\text{d}}u}}} \right)_{{{\text{rad}},i}} \) is defined as the excess mortality from cancer in structure i due to radiation exposure per age group (per 100000 individuals). P(u) is the population size per age group (of 100000 individuals). W(u) is the survival rate at age u (per 100000 individuals). Bi(u) is cancer mortality in structure i at age u (per 100 thousand individuals). r mi (u) is the excess relative risk factor of annual cancer mortality per age group in structure i (per mSv). D H is the equivalent dose (mSv); d is the dose and dose rate effectiveness factor (=2); α is the latency period before the development of cancer due to radiation exposure (leukemia 2 years; solid cancer 10 years). T(u) is the average life expectancy at age u (years). Si(u 0) is the shortening of the average life expectancy due to cancer in structure i at age of exposure u 0 (years per 100000 individuals).
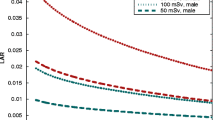
W(u) was obtained from the 20th complete life tables (2005) [11]. Bi(u) was obtained from Cancer Statistics [12], and r mi (u) was obtained from the report by Pierce et al. [13]. Figure 1 shows r mi (u) as reported by Pierce et al. [13]. According to this report, the latency period prior to the development of cancer because of radiation exposure is different between leukemias and solid cancers; leukemia is 2 years, and solid cancer is 10 years. Therefore, risk was calculated separately for leukemia and solid tumors, considering the latency periods, and the resulting risk values were added. Administered FDG spreads throughout the entire body, leading to internal exposure in all structures. Similarly, the CT exposure range is from the head to the pelvis, resulting in external exposure that covers most structures. Therefore, the risk of radiation exposure was evaluated for each structure in the entire body.
Excess relative risk factor of annual cancer mortality by radiation exposure (/mSv) per age group (graph based on the data by Pierce et al. [13])
The benefit of FDG-PET cancer screening is the prolonged life expectancy due to early detection and treatment of cancer by screening compared with the life expectancy of patients who do not undergo screening. Therefore, the difference in the 5-year survival rate (W s − W o) was defined as the benefit, and W s is the 5-year survival rate after cancer detection and treatment owing to FDG-PET cancer screening. W o is the 5-year survival rate after treatment following detection at a hospital visit for symptoms. The benefit was calculated using the following equations suggested by Iinuma [1–3]:
N′ is defined as the survival rate for each structure (per 100000 individuals). P is the population size per age group (of 100000 individuals). D is the morbidity of cancer per age group in each structure (per 100000 individuals). S is the sensitivity of FDG-PET cancer screening. W s is the 5-year survival rate in a screening group (per 100000 individuals). W o is the 5-year survival rate in a non-screening group (per 100000 individuals). N is the survival rate of all cancers (per 100000 individuals). NT is the surviving person-years (years per 100000 individuals). T is the average life expectancy (years).
D was obtained from Cancer Statistics [12]. Although FDG-PET cancer screening has the benefit that all structures in the body are screened for cancer at the same time, its efficacy has never been confirmed scientifically. Minamimoto et al. [14] reported in an investigation based on a national survey that the thyroid, colon, lung, prostate, breast, stomach, lymph, kidney, uterus, liver, pancreas, ovary, and cervix were the structures for which screening is effective. Therefore, we selected these structures to calculate the benefit. The NTs for all screened structures were added because the parameters varied by structure. The sensitivity of FDG-PET cancer screening (S) was the probability of the correct detection of cancer and was calculated as reported by Minamimoto et al. [14]. The PET and PET/CT results were evaluated separately because the sensitivity of cancer screening was different between the two modalities. W o was obtained from the Cancer Statistics [12]. W s (the 5-year survival rate of the FDG-PET cancer-screening group) was not determined. However, the report by Minamimoto et al. [14] showed that cancers up to stage 2 are often detected. Therefore, in this study, the 5-year survival rates in the screening group (W s) were assumed to be equivalent to those of stage 2 cancers [15, 16]. For the structures for which the 5-year survival rates by stage were not determined, the average 5-year survival rate of stage 2 cancer for all structures was used. Table 2 shows the sensitivity of FDG-PET cancer screening (S) and the relative 5-year survival rates of the screening and non-screening (all) groups. The average life expectancy of each age was obtained from the 20th complete life table (2005) [11].
The benefit/risk ratio (ω) was calculated using the following equation, in which the surviving person-year NT (benefit) is divided by the shortened period S(u) of the average life expectancy (risk):
A benefit/risk ratio ω < 1 indicates that the risk exceeds the benefit, indicating that the screening technique is not effective. Meanwhile, ω ≥ 1 indicates that the benefit exceeds the risk, indicating that the screening technique is effective. In this study, the effectiveness of screening was determined by evaluating ω.
Statistical analysis
All of the data were stored in a database (Microsoft Excel 2003). The standard deviation (SD) for the data is reported as needed. The Wilcoxon-Signed-Rank Test was used to compare the benefit/risk ratio between PET and PET/CT. A p value <0.05 was considered statistically significant.
Results
Ninety-eight institutions responded to the questionnaires out of the 156 PET-installed facilities that registered at the PET Summer Seminar Meeting in 2006. Sixty-seven facilities among 98 performed FDG-PET cancer screening and provided information regarding their screening situation.
Of the 67 facilities that performed FDG-PET cancer screening, 22 owned dedicated PET systems, and 51 owned PET/CT systems. The total number of dedicated PET systems in 22 facilities was 25. The total number of PET/CT systems in 51 facilities was 63. The details are shown in Table 3.
Most facilities covered the scan range from the top of the head to the thigh. Some facilities scanned from the head to the pelvis. The detailed scan range data are shown in Table 4.
The results of the FDG injection method and radioactivity were analyzed separately for the PET and PET/CT facilities. The mean injection radioactivity was first obtained for each institution. The mean values were then averaged for all of the corresponding facilities. Of the 22 PET facilities, the FDG injection radioactivity was constant in 6 facilities and varied by subject weight in 16 facilities. Of the six facilities with a constant injection radioactivity, five synthesized FDG with cyclotron, and one facility procured FDG from a pharmaceutical company. The mean injection radioactivity was 216.8 MBq (range 111–370 MBq). The 16 facilities that injected FDG in a radioactivity that varied by weight synthesized FDG with a cyclotron. The mean injection radioactivity was 3.7 MBq/kg (range 2.65–5 MBq/kg). This radioactivity was equivalent to 261 MBq (range 182–390 MBq) for the reference man model. For the reference woman model, the mean radioactivity was 205 MBq (range 143–275 MBq).
Of the 52 facilities that owned PET/CT machines, the FDG injection radioactivity was constant in 12 facilities and varied by weight in 40 facilities. Of the 12 facilities with constant injection radioactivity, FDG was synthesized with a cyclotron in 2 facilities; 10 facilities procured FDG from a pharmaceutical company. The injection radioactivity was 185 MBq in 12 facilities. Of the 40 facilities that used a variable-by-weight injection radioactivity, 38 synthesized FDG with a cyclotron, and 2 procured FDG from a pharmaceutical company. The mean injection radioactivity was 3.6 MBq/kg (range 2.6–4.5 MBq/kg). This radioactivity is equivalent to 252 MBq (range 182–315 MBq) for the reference man model. For the reference woman model, the mean radioactivity was 198 MBq (range 143–248 MBq). Table 5 shows the injection radioactivity in detail.
Regarding the CT parameters, the number of machines with each parameter was counted because some facilities owned plural systems, and the parameters varied by system. Twenty-five systems had a tube current of 120 kV, six had a tube current of 130 kV; twenty-four had a tube current of 140 kV, and eight had an unknown tube current. Fourteen systems had a fixed tube current, 43 varied, and six were unknown. The mean fixed tube current was 85.2 mAs (range 20–220 mAs). The mean pitch factor was 1.11 (range 0.75–1.75), with the exception of 11 systems with unknown parameters. Table 6 shows the collected CT parameters.
Radiation exposure calculation
The mean radiation exposure dose for dedicated PET cancer screening that was calculated on the basis of the collected questionnaire data was 4.7 mSv in men (range 2.1–7.0 mSv) and 4.0 mSv in women (range 2.1–7.0 mSv). The mean internal exposure dose for PET/CT cancer screening was 4.5 mSv in men (range 3.1–6.0 mSv) and 3.7 mSv in women (range 2.7–4.7 mSv). The mean external exposure dose of a CT scan integrated in PET/CT scanners was 10.1 mSv in men (range 2.1–28.0 mSv) and 9.7 mSv in women (range 2.1–27.0 mSv). The mean total radiation exposure dose in PET/CT cancer screening was 14.2 mSv in men (range 5.7–32.9 mSv) and 12.8 mSv in women (range 5.6–30.6 mSv). Table 7 shows the calculated effective dose of PET, and Table 8 shows the calculated effective dose for PET/CT.
Risk–benefit analysis
The risk–benefit analysis using the mean value of radiation exposure dose in FDG-PET cancer screening demonstrated a benefit/risk ratio (ω) > 1 in men aged between 40 and 49 years and women aged between 30 and 39 years for dedicated PET, in men aged between 50 and 59 years regardless of the FDG injection method, and in women aged between 60 and 69 years with a constant-dose injection and between 50 and 59 years with a varied-dose injection for PET/CT. Tables 9, 10, 11, and 12 show the calculated ω with regard to the PET system and FDG injection method.
Discussion
In the present investigation, PET/CT systems accounted for approximately 70% of the overall systems used for FDG-PET cancer screening. The dominance of PET/CT is explained by the higher diagnostic ability of PET/CT compared with dedicated PET because PET/CT allows reference to CT images and fusion images to reach a correct diagnosis. Therefore, newly established facilities preferably purchase PET/CT, and facilities with dedicated PET machines introduce PET/CT machines when they update their equipment.
In terms of the scanning ranges, most facilities scanned from the top of the head to the thigh, including the main structures. However, some facilities shorten the scan time by omitting the scan of the brain where physiological uptake is important.
The injection radioactivity tended to be larger with PET than with PET/CT. Facilities with a dedicated PET scanner may try to improve image quality by increasing the injection radioactivity and raising the count rate to compensate for the lack of information that could be obtained from CT images. However, most facilities that vary the dose by weight are likely to refer to the recommendation of a 3.7 MBq/kg injection dose by the Guideline of FDG-PET Cancer Screening [5] to set their dose standards.
With regard to the method used to obtain FDG, the facilities that used a constant injection radioactivity procure FDG from a pharmaceutical company. Most facilities that vary the injection dose by weight synthesize FDG with a cyclotron within the facility. The facilities that procure FDG from the outside face difficulties in varying the injection radioactivity by weight because procured FDG is prepackaged in syringes at 185 MBq.
The internal exposure dose of FDG was 3.7–4.5 mSv in both men and women. The internal exposure can be reduced if the injected FDG dose is reduced. However, an extended acquisition time is required to ensure image quality because otherwise the count rate during scanning would be smaller, compromising image quality [17].
In terms of the CT parameters, numerous facilities used CT-AEC to vary the tube current. CT-AEC is a technique that successively alters the tube current in a helical scan because the radiation dose required for image acquisition differs depending on the body region. The reduction in radiation exposure dose is expected in this technique by using a low tube current in body regions where a high tube current is unnecessary. Additionally, CT-AEC can be adjusted to achieve image quality that is optimal for diagnosis. When a reference CT scan is performed using CT-AEC with a setting for typical PET/CT cancer screening, the highest tube current is approximately 100 mAs. Even the facilities that use a fixed tube current are probably trying to reduce the exposure by setting the tube current to less than 100 mAs.
The Guidelines of FDG-PET Cancer Screening [5] classify the CT radiation exposure dose into three levels: (1) the radiation exposure dose is less than 2 mSv, and CT is used only for attenuation correction (extremely low dose), (2) the radiation exposure dose is 2–12 mSv, and CT is used for reference and fusion images (low dose to middle dose), and (3) the radiation exposure dose is greater than 12 mSv, and clinical CT is used for diagnosis (high dose). In the present investigation, 31 facilities could be classified as level 2, and 14 facilities could be classified as level 3. This result suggests that all facilities used a combination of CT and PET images for diagnosis. From the viewpoint of radiation exposure, the Guidelines of FDG-PET Cancer Screening [5] recommend level 1 or 2. Level 3 may have a greater risk of high radiation exposure relative to the benefit that may not always keep pace.
The mean total radiation exposure dose of PET/CT cancer screening was 14.2 mSv in men and 12.8 mSv in women. PET/CT cancer screening has a higher radiation exposure dose than other X-ray examinations; therefore, it should be performed only after the subjects understand the risks and benefits of FDG-PET cancer screening. Because the target of cancer screening is an asymptomatic population, the facilities should follow guidance on the adequate radiation exposure dose to avoid using an injection radioactivity of FDG that is too high or a CT tube current that is too large.
In the risk–benefit analysis of FDG-PET cancer screening, ω exceeded 1 in a lower age group of dedicated PET than PET-CT. This suggests that dedicated PET screening is more effective for a lower age group than PET/CT. In terms of ω, dedicated PET obtained significantly larger values than PET/CT regardless of the injection method of FDG (p < 0.05). From the viewpoint of radiation exposure risk, PET cancer screening is recommended for people in their 40s or older, and PET/CT cancer screening is recommended for people in their 50s or older. According to Minamimoto et al. [14], most people who undergo FDG-PET cancer screening in their 50s or older (70.8%) may potentially enjoy the benefits of such screening. In PET without CT, physicians cannot refer to fusion or CT images for diagnosis. Therefore, dedicated PET detectability of cancer is inferior to that of PET/CT, and the benefit decreases. In this study, ω was used to evaluate the risk–benefit by considering the difference in detectability between dedicated PET and PET/CT. Dedicated PET, in which radiation is derived only from internal exposure and thus is lower, showed a more important risk decrease than benefit decrease and thus proved more pertinent for a lower age group than PET/CT.
This study has the following drawbacks. First, FDG-PET cancer screening is usually combined with other cancer-screening tests [5]. The FDG-PET cancer-screening sensitivity used in the benefit calculations in this study was obtained by combining the sensitivity of FDG-PET (PET/CT) examination and the sensitivity of other cancer-screening methods. FDG-PET cancer-screening sensitivity varied depending on the facility because the other cancer-screening methods and their accuracy are substantially different between facilities [5, 18, 19]. This study used the mean sensitivity for FDG-PET cancer screening in all of the relevant facilities for evaluation; thus, the study design has a general nature. The data should be reanalyzed to evaluate individual facilities. Presently, many facilities combine various X-ray examinations, such as lung cancer CT and mammography, with FDG-PET cancer screening. Radiation from these combined examinations should also be considered in risk–benefit analyses. A more broad view may also be required to evaluate the effectiveness of an examination, considering not only the radiation viewpoint but also adverse effects and other risks that possibly arise from the test. For example, compared with endoscopy, which is considered to be invasive because of the risk of perforating the gastrointestinal tract, FDG-PET cancer screening is less invasive because only FDG is administered intravenously to the subject.
Second, in this study, a risk–benefit analysis was performed by assuming that the subjects underwent FDG-PET cancer screening only once. No evaluation was made regarding the subjects who underwent FDG-PET cancer screening twice or more often during the past years. When subjects undergo repeated FDG-PET cancer screenings, a risk–benefit analysis should be performed using different parameters (e.g., sensitivity of screening, 5-year survival rate of the screening group) other than those used for first-time screening. Moreover, when subjects undergo repeated FDG-PET cancer screening, the radiation exposure dose is cumulative. The method of evaluation of oncologic risk due to repeated radiation exposure is currently under investigation.
The FDG-PET cancer-screening situation in Japan was revealed from the investigation of radiation exposure requested by the guidelines. By encouraging the facilities to refer to the results to review their screening protocols, a reduction in radiation exposure is expected, and the screening is expected to be further standardized from the viewpoint of radiation exposure.
Conclusions
The actual situation of radiation exposure of FDG-PET cancer screening was studied, and a risk–benefit analysis was conducted on the basis of the field investigation. The average estimated effective dose was 4.4 mSv (male 4.7 mSv; female 4.0 mSv) for dedicated PET and 13.5 mSv (male 14.2 mSv; female 12.8 mSv) for PET/CT. As a result, the risk/benefit break-even age from the viewpoint of radiation exposure was in the 40s for men and 30s for women for dedicated PET and in the 50s for men (regardless of the injection method) and 50s (for variable dose) or 60s (for constant dose) for women for PET/CT. FDG-PET cancer screening is beneficial for examinees, but this benefit depends on age, gender, and type of examination (PET or PET/CT). The benefit/risk ratio can be improved if the radiation exposure dose is reduced and the subsequent risk is also reduced.
References
Iinuma T, Tateno Y, Hashizume T, Umegaki Y, Kitabatake T. Benefit-risk analysis for mass screening of stomach cancer in Japan. 1. Life-saving vs. loss of life. Nippon Igaku Houshasen Gakkai Zasshi. 1977;37:1109–21.
Iinuma T, Tateno Y. Risk–benefit analysis for mass screening of breast cancer utilizing mammography as a screening test. Nippon Igaku Houshasen Gakkai Zasshi. 1989;49:1091–5.
Iinuma T, Tateno Y. Benefit-risk analysis of mass screening for lung cancer. Nippon Igaku Houshasen Gakkai Zasshi. 1990;50:101–6.
Murano T, Iinuma T, Tateno Y, Daisaki H, Tateishi U, Terauchi T, et al. Risk–benefit analysis of 18FDG-PET cancer screening. Nippon Houshasen Gijutsu Gakkai Zasshi. 2008;64:1151–6.
Japanese Society of Nuclear Medicine. The guideline of FDG-PET cancer screening. Kaku Igaku. 2007;44:1–28.
International Commission on Radiological Protection. Radiation dose to patients from radiopharmaceuticals, ICRP Publication 80, Addendum to ICRP 53, J Valentine. Oxford: Pergamon Press; 1998.
Jones D, Shrimpton P. NRPB-SR250: Normalised organ doses for x-ray computed tomography calculated using monte carlo techniques. National Radiological Protection Board; 1993.
ImPACT. CT patient dosimetry Excel spreadsheet (version 0.99v, 17 June 2004). http://www.impactscan.org/.
International Commission on Radiological Protection. Referenceman: anatomical physiological and metabolic characteristics. ICRP Publication 23, J Valentine. Oxford: Pergamon Press; 1975.
1990 Recommendation of the International Commission on Radiological Protection (ICRP Publication 60). Ann Icrp, vol 21. Oxford: Pergamon; 1991. p. 1–201.
The 20th Life Tables For Japan 2005. Statistics and Information Department Minister’s Secretariat Ministry of Health, 2007.
Cancer Statistics in Japan 2007. The Editorial of the Cancer Statistics in Japan; 2007.
Pierce D, Shimizu Y, Preston D, Vaeth M, Mabuchi K. Studies of the mortality of atomic bomb survivors. Report 12, Part 1. Cancer. 1950–1990. Radiat Res. 1996;146:1–27.
Minamimoto R, Senda M, Uno K, Jinnouchi S, Iinuma T, Ito K, et al. Performance profile of FDG-PET and PET/CT for cancer screening on the basis of a Japanese Nationwide Survey. Ann Nucl Med. 2007;21:481–98.
Okamoto N, Saruki N, Mikami H, Yamashita K, Maruyama Y, Yano T, et al. 5-year survival rates for primary cancer sites at cancer-treatment-oriented hospitals in Japan. Asian Pacif J Cancer Prev. 2006;7:46–50.
Saruki N. 16-2 Chiiki gan-senmon-shinryou-shisetsu no sofuto-men no seibi-kakusyuu ni kansuru kenkyuu. A 2006 report of Grant-in-Aid for Cancer Research from the Ministry of Health, Labor, and Welfare, Japan. 2006; p. 21–34.http://www.gunma-cc.jp/sarukihan/seizonritu/index.html/.
Daisaki H, Suzuki K, Fukukita H, Fukushima H, Satou T, Shinohara H. Influence of count rate on image quality in three-dimensional PET acquisition. Nippon Houshasen Gijutsu Gakkai Zasshi. 2008;64(4):407–16.
Terauchi T, Murano T, Daisaki H, Kanou D, Shoda H, Kakinuma R, et al. Evaluation of whole-body cancer screening using 18F-2-deoxy-fluoro-d-glucose positron emission tomography: a preliminary report. Ann Nucl Med. 2008;22(5):379–85.
Ide M. Cancer screening with FDG-PET. Q J Nucl Med Mol Imaging. 2006;50(1):23–7.
Acknowledgments
This research was supported by a Grant-in-Aid for Cancer Research from the Ministry of Health, Labor, and Welfare, Japan. The authors thank Sachiko Yanagida and Yoshihide Nakamura of the Japan Radioisotope Association for their cooperation in the field investigation.
Author information
Authors and Affiliations
Corresponding author
Additional information
This article was previously published in Kakuigaku in Japanese (48[1]:1–13.2011). We obtained permission from the editorial office to republish this article in English.
Rights and permissions
About this article
Cite this article
Murano, T., Minamimoto, R., Senda, M. et al. Radiation exposure and risk–benefit analysis in cancer screening using FDG-PET: results of a Japanese nationwide survey. Ann Nucl Med 25, 657–666 (2011). https://doi.org/10.1007/s12149-011-0511-1
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12149-011-0511-1