Abstract
Aim
To evaluate the effect of the 18F-FDG PET-CT respiratory gating (4D) study in the correct documentation of pulmonary lesions with faint uptake in standard PET-CT.
Methods
Forty-two pulmonary lesions with a low or no detectable uptake of FDG (SUVmax < 2.5) in 3D PET-CT were prospectively evaluated in 28 patients (19 males and 9 females), mean age 66.5 years (41–81). 22 patients had neoplastic background. A conventional PET-CT (3D) total body scan was performed approximately 60 min after iv injection of a mean dose of 370 MBq. Furthermore, a 4D PET-CT (synchronized with respiratory movement) thorax study was acquired. SUVmax was determined for each lesion in both studies. For the 4D studies, we selected the SUVmax in respiratory period with the highest uptake (“best bin”). We calculated the SUVmax percentage difference between 3D and 4D PET-CT (% difference = SUVmax 4D − SUVmax 3D/SUVmax 3D × 100) and the relation of this value with the size and locations of the lesions. In 4D study, any lesion with SUVmax ≥ 2.5 was classified as malignant. We assessed the changes of lesion classification (from benign to malignant) applying the 4D technique. The final diagnosis was obtained by histological assessment or clinical and radiological follow-up longer than 12 months.
Results
Forty out of 42 lesions showed an increase of SUVmax in the 4D study with respect to 3D. The mean SUVmax in the 3D and 4D PET-CT studies were 1.33 (±0.59) and 2.26 (±0.87), respectively. The SUVmax percentage difference mean between both techniques was 83.3% (±80.81).The smaller the lesion the greater was the SUVmax percentage difference (P < 0.05). No differences were observed depending on the location of the lesion. In 40% of cases, there was a change in the final classification of lesions from benign to malignant. In the final diagnosis, 24 lesions were malignant. 4D PET-CT diagnosed correctly the 52% of them.
Conclusions
The 4D PET-CT study permitted a better characterization of malignant lung lesions compared with the standard PET-CT, because of its higher sensitivity. 4D PET-CT is a recommendable technique in the early diagnosis of malignant lesions.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
The metabolic uptake grade of a pulmonary lesion is extremely important, since it will make possible to classify it as benign or malignant, and consequently, to determine the management of the patient (follow-up or biopsy, respectively). In the PET image of a pulmonary lesion, the respiratory motion not only causes a distortion in its morphology with worse shape definition but also a decrease in the FDG activity detected that possibly limiting the sensitivity in the lesion detection [1]. Thus, some authors have proposed investigating new threshold values due to the existence of a higher rate of “false classifications” in infracentimetric lesions [2, 3].
Although the global sensitivity and specificity of FDG-PET have very high values (96.8 and 77.8%, respectively) in the classification of solitary pulmonary nodules [4], the sensitivity decreases for lesions smaller than 2 cm (70%) [4–6]. The motion effect depends on the pulmonary region analyzed and the lesion size, causing greater detriment in the detection of a small nodule situated in the basal part of lungs than of a pulmonary mass [7] due to the addition to the partial volume effect [8]. Therefore, the respiratory movements may affect the diagnosis [9]. Although a SUV of >2.5 has been reported to indicate a higher probability for malignancy, some authors describe that a cutoff threshold should not be correlated with malignancy in lung lesions [10].
With regard to the application of the 4D system in the metabolic image, some previous studies show that respiratory gating, or 4D PET, may significantly improve the accuracy of tumor volume determination and of FDG quantification in the thorax [2, 11–17]; however, its clinical diagnostic impact has not been fully assessed yet.
According to that, the objective in the present work was to evaluate the impact of 4D in the correct documentation of pulmonary lesions classified as benign, attending to semiquantitative parameters (SUVmax < 2.5) in standard PET-CT. Furthermore, we assess the change in the previous diagnosis of lesions attending to semiquantitative parameters in order to define a possible indication of 4D PET-CT.
Materials and methods
Patients
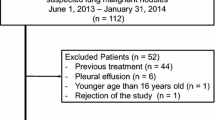
To establish the added value of PET scanning synchronized with respiratory movement with respect to conventional PET study, we studied prospectively 42 lung lesions suspicious for malignancy in 28 patients (19 men and 9 women).
The mean age of our patients was 66.5 years (41–81 years). 22 patients had neoplastic background, and in the remaining patients there was no known history of malignancy. Detailed data are reported in Table 1.
The lung lesions had a size from 0.5 to 2.8 cm. 23 lesions were in upper lobes (14 right and 9 left) and 19 in medium and lower lobes (10 right and 9 left).
All the lesions showed a low or no detectable uptake of FDG with SUVmax < 2.5 in conventional PET-CT.
All patients fasted for at least 4 h prior to PET/CT scans. Glucose levels were lower than 180 mg/dl in all cases.
Methodology
The PET-CT imaging was performed with a combined PET-CT scanner (Discovery STE 16, GE Healthcare). Prior to PET acquisition, helical CT was performed from the head to the proximal thigh according to a standardized protocol. No oral or intravenous contrast agents were used. Emission scans from the head to the proximal thigh were acquired at 60 min after injection of a mean dose of 370 MBq of FDG. Images were acquired in three-dimensional mode (3D), 3 min per table position. PET images were reconstructed using CT for attenuation correction with the ordered-subset expectation maximization iterative reconstruction algorithm.
Within 60 min after the conventional 3D PET/CT, a 4D PET-CT (synchronized with respiratory movement) located in thorax was acquired in one bed position. In this study, only the emission acquisition was gated for respiration (12 min/bed). The gating tool used was the Real-Time Position Management, RPM (Varian Medical Systems). The respiratory cycle was divided in 6 bins.
Because the transmission image used for attenuation correction was not gated, an attenuation map obtained from helical CT was used to perform this correction on each gate throughout the respiratory cycle.
Analysis of lesions
The SUVmax was determined for each lesion in both studies. For the gated studies, SUVmax was calculated in each bin. We selected the SUVmax in respiratory period (bin) with the highest uptake (“best bin”) for lesion classification. Later, we calculated the SUVmax percentage difference between 3D and 4D PET-CT (% difference = SUVmax 4D − SUVmax 3D/SUVmax 3D × 100) to compare both techniques. In Fig. 1 is showed an example.
A threshold value of 2.5 was selected establishing that any lesion with SUVmax ≥ 2.5 in the 4D should be classified as malignant. In addition, we determined the number of lesions that had changed their classification in the 4D study with respect to conventional PET.
Statistical analysis
The SUVmax mean values of 3D and 4D PET-CT were calculated for all lesions and mean SUVmax percentage difference. We correlated the change in the value of SUVmax with lesion size, location and final diagnosis. SUVmax percentage difference and the size of lesion were compared by the Spearman test.
Mann–Whitney and Kruskal–Wallis test were used to compare quantitative variables (P < 0.05 was considered statistically significant). Statistical diagnostic parameters were calculated for 3D and 4D PET-CT. A ROC-analysis (receiver-operating characteristics) was performed, and the best cut-off was calculated for the diagnostic test parameters.
Final diagnosis
Confirmation was made by histological assessment or clinical and radiological follow-up longer than 12 months.
Results
Twenty-three lesions were malignant. Confirmation was made by histological assessment in 11 lesions and by clinical and radiological follow-up in the rest of lesions. The distribution of the results is showed in Table 1.
Forty out of 42 lesions showed an increase of SUVmax in the 4D study with respect to 3D. 1 lesion was not detected in 3D and showed metabolism in 4D study. 2 lesions did not show change in semiquantitative parameters in both explorations. In 32/42 lesions, the greater increase in SUV was observed in expiratory phase.
The mean SUVmax in the 3D and 4D PET-CT studies were 1.33 (±0.59) and 2.26 (±0.87), respectively. The SUVmax percentage difference mean between both techniques was 83.3% (±80.81).
In 40% of cases, there was a change in the final classification of lesions from benign to malignant attending to 4D PET-CT, and the 52% of malignant lesions were diagnosed correctly. Statistical diagnostic parameters for 3D and 4D PET-CT are represented in Table 2.
After ROC analysis, a SUVmax value of 0.6 showed to be the best diagnostic parameter of sensitivity 92% for the 3D study but with a very low specificity (17%). In the 4D study, this value was of 1.2 (92% of sensitivity and 11% of specificity). On the contrary, the values of SUVmax with the higher specificity were 2 and 3 for 3D and 4D, respectively. The ROC analysis is presented in Fig. 2 and shows no statistical differences in global parameters between both techniques although there is a tendency towards an improvement of them in 4D.
In the correlation between the SUVmax percentage difference with other parameters, we observed a higher increase of SUVmax in the smaller lesions with respect to the bigger ones, and this value was statistically significant (P < 0.005). The lesions mean size was 1.2 cm (±0.56). The correlation is represented in Fig. 3.
No statistically significant differences were observed depending on the location of the lesion, but the right lung showed higher values of SUVmax increase in 4D with respect to the left lung (mean of 101.30 ± 89.62 and 59.31 ± 61.76%; P = 0.208), and superior lobes showed a greater SUV increase than the lower lobes (mean of 90.74 ± 92.88 and 77.87 ± 64.11%, respectively; P = 0.947).
There were no statistically significant differences between the final diagnosis and SUVmax percentage difference of lesions with a mean SUVmax percentage difference of 85.81 ± 90.20 and 81.23 ± 74.18% for benign and malignant lesions, respectively.
Discussion
Respiratory motion causes, as a principal effect, a decrease in concentration per pixel within lung lesions that ranged from 21 to 45% and may sometimes exceed 50% of its maximum activity in phantom studies [14, 18]. This conditioning factor is connected to that derived from the limited resolution of the PET, and reduces the lesion/background index, decreasing the contrast. Thus, it is proposed that a threshold value of 2.5 should not be related with malignancy in small pulmonary lesions [2], and some authors have described that the simple visualization of metabolic activity, although it does not surpass the reference threshold value in a nodule whose size is approximately 1 cm or less, may mean malignancy. On the other hand, absence of metabolic detectability in a nodule, especially if it is subcentimetric, cannot rule out malignancy; therefore, radiological follow-up is recommended [12].
Other factors like lesion size and lack of spatial alignment between the emission and transmission images in the hybrid equipments determine if the motion itself has a greater or lesser effect. With regard to size, it has been demonstrated that lesions whose diameters are about 3 cm or greater are the least affected by the motion, while those with diameters that are similar or less than the shift range suffer variations in their activity of 20–30% compared to that obtained in the steady state [7, 15].
In relation with the spatial alignment, the combined synchronization technique has offered a more accurate quantification values compared with those obtained from the synchronization of each one separately. This means that there are more correct tumor images and intralesion SUV values, as has been demonstrated by Nehmeh et al. [12] and Hamill et al. [15] in their studies. These differences may reach 36% if the SUVs obtained in the 4D PET/CT scan are compared to SUVs calculated in 4D PET with helical CT [12]. In our work, the mean increment of SUV generated by 4D was quite high (83%) in spite of the absence of synchronization in CT. Perhaps this procedure is a limitation and could affect our results in some way although the combined procedure, in our opinion, may not add any advantage in small lesions, like most of them in this work (1.20 ± 0.56 cm).
Up to now, there has been scarce applicability of the 4D technique in the evaluation of pulmonary lesions, and although the results have been positive, increasing the metabolic activity, its added value in regards to the change of classification of the lesions has not been fully evaluated [19].
Some authors have found variations in the SUV of up to 159% and reductions in the lesion volume of up to 34%, only using synchronization in the PET image [2]. In regards to the 4D PET-CT scan, and although there are few works, all have obtained similar results in relation to the increase of the SUV and the decrease of the lesion volumes [12, 15].
In respiratory gating acquisition the greatest coincidence between the PET and CT scan images occurs in the expiratory phase, although this is never exact since there will always be an inherent mismatch between both due to the fact that the metabolic geometry of a lesion does not correspond with the structural one [8]. However, if we analyze how the respiratory cycle phase influences the quantitative parameters, the maximum concentration of the metabolic activity is generally in the expiratory phase because the motion is very low in this phase and it improves in the coregistry. In the present study, most of the lesions (32/42) showed the highest SUVmax values in the expiratory phase.
A high sensitivity and specificity of the PET in the characterization of pulmonary lesions, with mean values of 95 and 82%, is known [20]. However, if small-sized lesions (smaller than 2 cm) are evaluated, the sensitivity decreases to values around 70% [5, 6], and the percentage of errors in the diagnosis by PET of infracentimetric lesions may exceed 50%, at the expense of, above all, those of the false negatives (FN) [3]. To settle this matter, some procedures like normalization and delayed images have been developed.
It has not been shown that normalization or correction of the uptake values according to tumor size has any effect since as some authors have described the likelihood of malignancy in any metabolically visualizable lesion is 60% [6, 21].
The value of delayed or dual time point images has not yet been established. Delayed acquisition leads to an increase of the tumor/background ratio and a better qualitative evaluation of PET images, but has a disadvantage of reduced rate of true coincidences. Furthermore, the SUV values are calculated with a correction for radioactive decay, and a region with a similar SUV at 3 h actually has approximately half the true counts of the region at 1 h [22]. On the other hand, the results about the improvement in sensitivity are variable [23–25].
According to dual time point images, Nuñez et al. [23] studied 83 pulmonary lesions and obtained a raise of sensitivity from 74 to 85%. Kim et al. [24] studied 30 lesions with characteristics similar to ours, SUVmax < 2.5 in standard PET-CT, and found that delayed images increased the sensitivity from 8 to 23%. In our case, respiratory-gated PET obtained a sensitivity of 52%, attending to a semi-quantitative approach. We are aware that this value is not enough for diagnostic purposes, but improved the detection of malignant lesions with respect to the standard procedure.
Other procedure, deep-inspiration breath-hold (DIBH) PET/CT, has been developed as an alternative to 4D PET/CT [26, 27]. This procedure uses the RPM system in its amplitude-gating mode to monitor the patient respiratory motion and acquires CT and PET frames for a total of 3 min in hold condition.
Nehmeh et al. [26, 27] showed an increase in lesion SUV as much as 83% and an improved spatial matching between PET and CT as much as 50% using DIBH PET/CT versus nonrespiratory motion-corrected PET/CT. Furthermore, this technique improved the detection visualizing additional nodules, allowed a more precise localization and characterization of pulmonary lesions than non-DIBH CT and reduced respiratory motion-related mis-registration between PET and CT [28, 29]. In addition, the same authors have reported significant advantages of DIBH acquisition over 4D protocols as the former does not require the patient to follow verbal instructions for the duration of the breathing cycle, allows a better image quality than gated acquisitions due to the increased statistics, and offers the possibility of discard suboptimal data acquired in irregular breath.
In our department, we do not give instructions to the patients during 4D, only some recommendations before the acquisition in cases of irregular breath. In our opinion, to maintain a regular breathing motion is important for both procedures. Furthermore, in DIBH acquisition the patient has to be instructed to breathe deeply and to hold the breath up to 20 s until all the necessary frames have been obtained. In relation to this limitation Kawano et al. [30] developed a shorter DIBH protocol and observed a percentage difference mean of uptake increase with respect to a standard protocol of 26.6 ± 37.2, lower than ours results.
Unfortunately, both 4D and DIBH techniques have been mostly performed in malignant lung lesions with high FDG uptake in standard PET [2, 11–15, 17, 30, 31]. Therefore, the added value that the increase of the activity detected in a lesion may have is still unknown. So, in order to clarify the diagnostic impact of any procedure, it is important to include doubtful lesions.
In our casuistic all lesions showed low metabolic activity values (lower than the threshold value of 2.5). However, in 17 of them, this value reached pathological levels after performing the 4D technique. We do not know of any other work that has determined this fact. Thus, this study offers an analysis of how the 4D technique permits an evaluation of the metabolic activity more in agreement with the reality and possibly more effective as it increases the sensitivity in the detection of a lesion.
In our case, the 4D technique made possible to reduce the FN rate by 50% (from 23 to 11), compared to the 3D technique. Considering the results of the 4D technique, 12 lesions would have been correctly classified as malignant and 5 would have been erroneously classified (false positives). Therefore, although attending to global diagnostic parameters, no statistical differences were observed between 3D and 4D in ROC analysis; the improvement in the detection allowed a more correct characterization of lesions, so as accuracy increased from 45 to 62%, respectively.
Our study had some limitations. The delay of acquisition of 4D could contribute to the SUV parameters, but in our opinion this effect was not the principal cause of the observed SUV increase taking into account the shorter time of acquisition in each bin (2 min) of the 4D acquisitions with respect to the 3D (3 min/bed). The diagnostic impact of both techniques in the same group of patients would clear these doubts and determine and compare the diagnostic impact of the two available solutions to improve lesion detection. Other limitations were the small number of patients and absence of histological confirmation in all the lesions. Due to ethical reasons, we perform only 4D in cases of doubtful lesions in standard 3D PET/CT acquisition. On the other hand, it is difficult to obtain histological specimens in all the cases due to the small size of some lesions and patient conditions.
Other authors have reported that the evaluation of small pulmonary lesions, attending to clinical interpretation of PET scans in order to determine the benign of malignant nature of them, independent of the used visual or semiquantitative criteria, has the limitation of the partial volume effect [32]. We completely agree with this assertion and although, attending to our results, smaller lesions had the bigger increase in SUVmax after 4D PET-CT. This technique was not good enough to detect all the malignant lesions using the 2.5 threshold, and other thresholds did not show a significative improvement of the diagnostic accuracy. So, due to the inherent limitation of lesion size, all our efforts should be focused in the development of strategies for the early detection of malignant pulmonary lesions.
Conclusion
The acquisition of the 18F-FDG PET-CT scan in 4D shows metabolic activity values more in accordance with the reality, increasing the sensitivity of lesion detection from the metabolic point of view.
Attending to our results, 4D PET-CT is a good option to improve the detection of malignant pulmonary nodules with faint FDG uptake in standard PET-CT acquisition, especially the smaller ones but bigger than the double of the spatial resolution of the PET-CT system.
References
Osman MM, Cohade C, Nakamoto Y, Wahl RL. Respiratory motion artifacts on PET emission images obtained using CT attenuation correction on PET-CT. Eur J Nucl Med Mol Imaging. 2003;30:603–6.
Nehmeh SA, Erdi Y, Ling CC, Rosenzweig E, Shoder H, Larson SM, et al. Effect of respiratory gating on quantifying PET images of lung cancer. J Nucl Med. 2002;43:876–81.
Bryant AS, Cerfolio RJ. The maximum standardized uptake values on integrated FDG-PET/CT is useful in differentiating benign from malignant pulmonary nodules. Ann Thorac Surg. 2006;82:1016–20.
Gould MK, Maclean CC, Kuschner WG, Rydzak CE, Owens DK. Accuracy of positron emission tomography for diagnosis of pulmonary nodules and mass lesions: a meta-analysis. JAMA. 2001;285:914–24.
Degirmenci B, Wilson D, Laymon CM, Becker C, Mason NS, Bencherif B, et al. Standarized uptake value-based evaluations of solitary pulmonary nodules using F-18 fluorodeoxyglucose-PET/computed tomography. Nucl Med Commun. 2008;29:614–22.
Kim SC, Machac J, Krynyckyi BR, Knesaurek K, Krellenstein D, Schultz B, et al. FDG PET for evaluation of indeterminate lung nodules: assigning a probability of malignancy may be preferable to binary readings. Ann Nucl Med. 2008;22:165–70.
Pevsner A, Nehmeh SA, Humm JL, Mageras GS, Erdi YE. Effect of motion on tracer activity determination in CT attenuation corrected PET images: a lung phantom study. Med Phys. 2005;32:2358–62.
Goerres GW, Kamel E, Seifert B, Burger C, Buck A, Hany TF, et al. Accuracy of image coregistration of pulmonary lesions in patients with non-small cell lung cancer using an integrated PET/CT system. J Nucl Med. 2002;43:1469–75.
Beyer T, Antoch G, Blodgett T, Freudenberg LF, Akhurst T, Mueller S. Dual-modality PET/CT imaging: the effect of respiratory motion on combined image quality in clinical oncology. Eur J Nucl Med Mol Imaging. 2003;30:588–96.
Lowe VJ, Fletcher JW, Gobar L, Lawson M, Kirchner P, Valk P, et al. Prospective investigation of positron emission tomography in lung nodules. J Clin Oncol. 1998;16:1075–84.
Erdi Y, Nehmeh SA, Pan T, Pevsner A, Rosenzweig KE, Mageras G, et al. The CT motion quantitation of lung lesions and its impact on PET-measured SUVs. J Nucl Med. 2004;45:1287–92.
Nehmeh SA, Erdi YE, Ling CC, Pevsner A, Rosenzweig KE, Yorke E, et al. Four dimensional (4D) PET/CT imaging in the thorax. Med Phys. 2004;31:3179–86.
Larson SM, Nehmeh SA, Erdi Y, Humm JL. PET-CT in non-small-cell lung cancer: value of respiratory-gated PET. Chang Gung Med J. 2005;28:306–14.
Pan T, Mawlawi O, Nehmeh SA, Erdi YE, Luo D, Liu HH, et al. Attenuation correction of PET images with respiration-averaged CT images in PET/CT. J Nucl Med. 2005;46:1481–7.
Hamill JJ, Bosmans G, Dekker A. Respiratory-gated CT as a tool for the simulation of breathing artifacts in PET and PET-CT. Med Phys. 2008;35:576–85.
Cheng N-M, Yu C-T, Ho K-C, Wu YC, Liu YC, Wang CW, et al. Respiration-averaged CT for attenuation correction in non-small-cell lung cancer. Eur J Nucl Med Mol Imaging. 2009;36:607–15.
Lupi A, Zaroccolo M, Salgarello M, Malfatti V, Zanco P. The effect of 18F-FDG-PET/CT respiratory gating on detected metabolic activity in lung lesions. Ann Nucl Med. 2009;23:191–6.
Boucher L, Rodriguez S, Lecomte R, Bénard F. Respiratory gating for 3-dimensional PET of the thorax: feasibility and initial results. J Nucl Med. 2004;45:214–9.
García Vicente AM, Soriano Castrejón A, Talavera Rubio MP, Poblete García VM, Palomar Muñoz A, Cepedello Boiso I, et al. 18F-FDG PET/CT and respiratory synchronization: effect in the detection and classification of pulmonary lesions. Rev Esp Med Nucl. 2009;28(4):181–7.
Cronin P, Dwamena BA, Kelly AM, Carlos RC. Solitary pulmonary nodules: meta-analytic comparison of cross-sectional imaging modalities for diagnosis of malignancy. Radiology. 2008;246:772–82.
Hashimoto Y, Tsujikawa T, Kondo C, Maki M, Momose M, Nagai A. et al. Accuracy of PET for diagnosis of solid pulmonary lesions with 18F-FDG uptake below the standardized uptake value of 2.5. J Nucl Med. 2006;47:426–31.
Chin BB, Green ED, Turkington TG, Hawk TC, Coleman RE. Increasing uptake time in FDG-PET: standardized uptake values in normal tissues at 1 versus 3 h. Mol Imaging Biol. 2009;11:118–22.
Nuñez R, Kalapparambath A, Varela J. Improvement in sensitivity with delayed imaging of pulmonary lesions with FDG-PET. Rev Esp Med Nucl. 2007;26:196–207.
Kim IJ, Kim SJ, Kim YS, Lee TH, Jeong YJ. Characterization of pulmonary lesions with low F18-FDG uptake using double phase F-18 FDG-PET: comparing of visual and quantitative analyses. Neoplasma. 2009;56:33–9.
Cloran FJ, Banks KP, Song, Kim Y, Bradley WC. Limitations of dual time point PET in the assessment of lung nodules with low FDG avidity. Lung Cancer. 2009. doi:10.1016/j.lungcan.2009.05.013.
Nehmeh SA, Erdi YE, Rosenzweig KE, Schoder H, Larson SM, Squire OD, et al. Reduction of respiratory motion artifacts in pet imaging of lung cancer by respiratory correlated dynamic PET: methodology and comparison with respiratory gated PET. J Nucl Med. 2003;44:1644–8.
Nehmeh SA, Erdi YE, Meirelles GSP, Squire O, Larson SM, Humm JL, et al. Deep-inspiration breathhold PET/CT of the thorax. J Nucl Med. 2007;48:22–6.
Nagel CCA, Bosmans G, Dekker ALAJ, Ollers MC, De Ruysscher DK, Lambin P, et al. Phased attenuation correction in respiration correlated computed tomography/positron emitted tomography. Med Phys. 2006;33:1840–7.
Meirelles GSP, Erdi YE, Nehmeh SA, Squire OD, Larson SM, Humm JL, et al. Deep-inspiration breathhold PET/CT: clinical findings with a new technique for detection and characterization of thoracic lesions. J Nucl Med. 2006;48:712–9.
Kawano T, Ohtake E, Inoue T. Deep-inspiration breath-hold PET/CT of lung cancer: maximum standardized uptake value analysis of 108 patients. J Nucl Med. 2008;49:1223–31.
Torizuka T, Tanizaki Y, Kanno T, Futatsubashi M, Yoshikawa E, Okada H, et al. Single 20-second acquisition of deep-inspiration breath-hold PET/CT: clinical feasibility for lung cancer. J Nucl Med. 2009;50:1579–84.
Hamberg LM, Hunter GL, Alpert NM, Choi NC, Babich JW, Fischman AJ. The dose uptake ratio as an index of flucose metabolism: useful parameter or oversimplification? J Nucl Med. 1994;35:1308–12.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
García Vicente, A.M., Soriano Castrejón, A.M., Talavera Rubio, M.P. et al. 18F-FDG PET-CT respiratory gating in characterization of pulmonary lesions: approximation towards clinical indications. Ann Nucl Med 24, 207–214 (2010). https://doi.org/10.1007/s12149-010-0345-2
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12149-010-0345-2