Abstract
The study examined the associations of anthropometric measures of obesity with high sensitivity C-reactive protein (hs-CRP) levels in Turkish immigrants with type 2 diabetes (T2D) living in the Netherlands. A total of 110 participants, physician-diagnosed with T2D, aged 30 years and older were recruited from multiple sources from The Hague, Netherlands. Serum hs-CRP levels were measured with immunoturbidimetric assay. Glycated hemoglobin (A1C) was determined by high-pressure liquid chromatography. Measures of obesity: body weight, body mass index (BMI), waist circumference (WC), hip circumference (HC), waist-to-hip ratio (WHR), and waist-to-height ratio (WHtR) were determined. Statistical analysis included descriptive statistics, Pearson’s correlations and multiple linear regressions (MLR) stratified by gender. Hs-CRP was log transformed to achieve normality. Subjects with hs-CRP levels >10 mg/L (n = 17) were excluded from the analysis. Females had a higher BMI (p = 0.007), HC (p < 0.001), and WHtR (p = 0.011) as compared to males. Conversely, males had a higher weight (p = 0.007), and WHR (p < 0.001) than females. MLR showed that after controlling for covariates, log hs-CRP was positively associated with BMI (B = 0.039, SE = 0.019, β = 0.287, p < 0.05), WC (B = 0.025, SE = 0.011, β = 0.332, p < 0.05) and WHtR (B = 4.015, SE = 1.464, β = 0.376, p < 0.01) in females only. Gender-specific associations between obesity measures and hs-CRP level need to be further investigated in the Turkish immigrant population. Hs-CRP assessment may be added as a standard of care for T2D treatment within this population.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Cardiovascular disease (CVD) is a significant cause of mortality and morbidity among individuals with type 2 diabetes (T2D) (Uitewaal et al. 2004a; Soinio et al. 2006). Recent literature suggests T2D to be a state of low-grade inflammation (Pickup 2004). Low-grade systemic inflammation is associated with an increased risk of CVD, where elevated serum C-reactive protein (CRP) levels are a reliable predictor of CVD and CVD risk factors (Soinio et al. 2006; Ujcic-Voortman et al. 2011; Onat et al. 2001; Onat et al. 2008). There are significant associations between obesity and increased circulating serum CRP levels in persons with obesity-related diseases (Onat et al. 2001; Huffman et al. 2009; Huffman et al. 2010). In the Netherlands, Turkish immigrants form the largest ethnic minority group with 388,967 inhabitants according to the 2011 census (CBS 2012). Several studies showed a higher prevalence of T2D, obesity, and elevated serum CRP levels among Turkish immigrants when compared to the indigenous Dutch (Uitewaal et al. (2004a); Ujcic-Voortman et al. 2011; Uitewaal et al. (2004b); Kriegsman et al. 2003; van Leest et al. 2002). Poor glycemic control combined with high prevalence of obesity in Turkish immigrants with T2D increases CVD risk. There is a higher prevalence of obesity among Turkish females as compared to their male counterparts (Uitewaal et al. (2004b); van Leest et al. 2002). A prospective cohort of the Turkish Adult Risk Factor (TARF) study, which included 1046 Turkish adults, found CRP levels to be greater for females than for males (Onat et al. 2001).
Obesity is a determinant of CRP levels (Onat et al. 2001). There is lack of agreement as to which indicator of obesity best predicts CVD risk (Connelly et al. 2003; Mojiminiyi et al. 2009; Can et al. 2009; de Koning et al. 2007; Schneider et al. 2010). Body mass index (BMI) was found to be an independent determinant of CRP level in females; whereas, waist circumference (WC) was an independent determinant of CRP level in males (Connelly et al. 2003). Other studies reported that waist-to-hip ratio (WHR) had a stronger correlation with CRP levels as opposed to BMI or WC (Snijder et al. 2003). However, Mojiminiyi et al. (2009) established WHR had the weakest correlations with CRP levels and that BMI was strongly associated with CRP levels in patients with T2D. Caan et al. (1994) suggested that both non-obese and obese individuals could exhibit the same WHR; and that it could remain constant for each individual during weight change. Conversely, several studies indicated that waist-to-height ratio (WHtR) was a better predictor of CVD than the more widely used BMI (Can et al. 2010; Schneider et al. 2010). Including either hip circumference (HC) or height into WC may provide additional information on CVD risk than WC alone (Can et al. 2009). Aside from the inconsistencies of obesity measurements and CRP levels, there is a scarcity of studies regarding the association of CVD risk factors with CRP levels in a Turkish population with T2D living in the Netherlands (Ujcic-Voortman et al. 2011). Therefore, the objective of this study was to examine the relationship between measures of obesity and CRP levels within this population. Examining these factors could provide important insights into the possible role of successful diabetes management and CVD prevention.
Methods and Procedures
Study Subjects
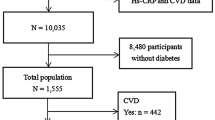
The study population consisted of 110 Turkish participants with T2D, aged 30 years and older. The investigation was a cross-sectional design that took place between March and May 2011. The participants were recruited from multiple sources in The Hague, Netherlands. Letters were sent to residents of The Hague who had Turkish surnames listed in the local telephone directory. During this 3-month period approximately 300 letters, written in Dutch and Turkish languages, outlining the study were mailed. The interested participants could respond to the invitation letter which included contact information. Due to unknown addresses, 1 % of the unopened letters were returned. Posters and flyers were also displayed at places where Turkish immigrants are known to visit and included a family physician’s office, a dietitian’s office, a health club center, mosques, hairdressers, grocery stores, a community center, and pharmacies. Eleven eligible participants were enrolled from the delivered mail, 60 participants were enrolled from the physician’s office, and 20 participants from other sources. A local community representative recruited 19 eligible participants. Twenty-two potential participants did not qualify for the study because they were either not Turkish (n = 3), or did not have T2D (n = 8), or did not provide blood samples within the 3-month study period (n = 11). Interested participants were initially interviewed on the phone, at which time the study purpose was explained, and the age and gender of the responders were recorded. To ascertain T2D status, each participant was asked for their age at diagnosis and initial treatment modalities. All participants were physician-diagnosed with T2D as having fasting serum glucose level of ≥ 6.1 mmol/L based on the classification recommended by the Dutch College of General Practitioners (NHG-standard 2006) (Bouma et al. 2006). This study was performed according to Dutch legislation regarding Ethics and Human Research and approved by The Central Committee on Research Involving Human Subjects (Centrale Commissie Mensgebonden Onderzoek). Florida International University Institutional Review Board (FIU-IRB) also approved the study protocol. Informed consent was obtained from all participants prior to the commencement of the study.
Anthropometric Measurements
All anthropometric measurements were obtained using standard techniques (Schneider et al. 2007) with the participant wearing light clothing without shoes. Height (rounded to the nearest 0.1 cm) was determined using a wall-mounted stadiometer, and weight (to the nearest 0.1 kg) was determined using a digital electronic clinical scale. BMI was calculated as weight (kg) divided by height (m2). WC was measured horizontally (to the nearest 0.1 cm) with a non-stretchable measuring tape placed midway between the lowest rib and the iliac crest with the participant standing and at the end of a slight expiration. Hip circumference (HC), the level of the widest diameter around the gluteal protuberance, was measured to the nearest 0.1 cm. WHR (WC in cm divided by HC in cm) and WHtR (WC in cm divided by height in cm) were calculated.
Laboratory Examination
Venous blood (20 mL) was collected, after an 8–12 hour overnight fast, by a certified phlebotomist who used standard laboratory techniques. Immediately after collection, blood samples were centrifuged; serum/plasma was separated, frozen and stored at −80 °C for analysis. All measurements were performed in a hospital laboratory at Medisch Centrum Haaglanden. The Roche Tina-quant® Cardiac C - reactive protein (Latex) High Sensitive (CRPHS) immunoturbidimetric assay was used for the in vitro quantitative determination of hs-CRP levels in the range from 0.1–20 mg/L. This assay is proven to be a suitable method for screening large populations (Lolekha et al. 2005). A1C was determined by high-pressure liquid chromatography (HPLC) using the Bio-Rad VARIANT™ II TURBO Hemoglobin A1C Program. This method is certified by the National Glycohemoglobin Standardization Program (NGSP) and standardized by the International Federation of Clinical Chemistry and Laboratory Medicine (IFCC) (Consensus Committee 2007).
Measurements of Risk Variables
A trained physician assistant (PA) fluent in both Dutch and Turkish languages, interviewed all participants. The PA assisted and completed questionnaires on age, smoking status, prescription medication(s) use including nonsteroidal anti-inflammatory drugs (NSAIDs), lipid-lowering drugs (LLD), hypertension medications, and diabetes medications. The investigators reviewed the questionnaires and the participants were contacted to inquire about any missing information. Current smokers were defined as having smoked at least 100 cigarettes per lifetime and reported smoking every day or some days (CDC 2002).
Statistical Analyses
Participants who had hs-CRP levels >10 mg/L (n = 17) were assumed to have acute phase infection, thus were excluded from the analysis, leaving a study sample of 93 participants (42 males and 51 females). Hs-CRP was log transformed to achieve normality. Differences between males and females were assessed using the independent samples t-test for numerical values and chi-square test for categorical variables. Pearson’s correlations were used to determine the relationship of measures of obesity with hs-CRP and other covariates stratified by gender. The impact of hs-CRP for males and females were assessed via separate multiple linear regression analysis (MLR) for each separate dependent variable including weight, BMI, WC, HC, WHR, and WHtR. All models were adjusted for age, A1C, smoking, NSAIDs, LLD, hypertension medications, and diabetes medications. Statistical analyses were conducted using the Statistical Package for the Social Sciences, SPSS, version 19.0 (SPSS Inc., Chicago, IL, USA). The level of statistical significance was set at p < 0.05.
Results
Participants
The general characteristics of the study participants are presented in Table 1. Females had higher mean BMI (p = 0.007), HC (p < 0.001) and WHtR (p = 0.011) as compared to males. Conversely, males had higher mean weight and WHR than females (p = 0.007, p < 0.001 respectively).
Age
Age of the study participants are presented in Table 2. Over two-thirds of the participants were aged 50 or older. Compared to those below the age of 50, the older participants had higher mean BMI (p = 0.016), WC (p = 0.008), HC (p = 0.042), WHtR (p = 0.002), and had a greater percent of hypertension medication use (p = 0.015).
Hs-CRP with Independent Determinants
Pearson’s correlations indicated that hs-CRP level was positively correlated with A1C (r = 0.281, p = 0.006) and WHtR (r = 0.211, p = 0.043) for the entire study sample (Table 3). When stratified by gender, hs-CRP level was positively correlated with A1C (r = 0.360, p = 0.010) in females only.
Measures of Obesity with Independent Determinants
Pearson’s correlations indicated that WC (r = 0.249, p = 0.016) and WHtR (r = 0.327, p = 0.001) were positively correlated with age for the entire study sample (Table 4). For males, WHR (r = 0.444, p = 0.003) and WHtR (r = 0.335, p = 0.030) were positively correlated with age. For females only, WHtR (r = 0.283, p = 0.045) was positively correlated with age. WHR (r = 0.313, p = 0.044) was positively correlated with A1C in males only. For the combined sample (males and females) HC (r = `−0.215, p = 0.038) and WHtR (r = −0.243, p = 0.019) were negatively correlated with smoking and WHR (r = 0.215, p = 0.038) was positively correlated with NSAIDs. When stratified by gender, WHR (r = 0.319, p = 0.022) was positively correlated with NSAIDs in females only. BMI (r = 0.238, p = 0.021) and WHtR (r = 0.243, p = 0.019) were positively correlated with LLD for the entire study sample. When stratified by gender, WHtR (r = 0.333, p = 0.031) was positively correlated with LLD in males only. Weight (r = 0.259, p = 0.012), BMI (r = 0.300, p = 0.004), WC (r = 0.341, p = 0.001), HC (r = 0.225, p = 0.031), and WHtR (r = 0.340, p = 0.001) were positively correlated with hypertension medications for the entire study sample. For males, BMI (r = 0.378, p = 0.014), WC (r = 0.393, p = 0.010), WHR (r = 0.450, p = 0.003), and WHtR (r = 0.457, p = 0.002) were positively correlated with hypertension medications. For females, weight (r = 0.295, p = 0.036), BMI (r = 0.301, p = 0.032), WC (r = 0.308, p = 0.028), HC (r = 0.328, p = 0.019), and WHtR (r = 0.301, p = 0.032) were positively correlated with hypertension medications.
Hs-CRP with Measures of Obesity
The results of MLR are presented in Table 5. After adjusting for covariates, hs-CRP explained 4.6 % of the variation in weight (β = 0.233, p = 0.026), 3.8 % of the variation in BMI (β = 0.217, p = 0.043), 7.8 % of the variation in WC (β = 0.313, p = 0.003), 3.8 % of the variation in HC (β = 0.223, p = 0.043), 3.8 % of the variation in WHR (β = 0.275, p = 0.042), and 6.1 % of the variation in WHtR (β = 0.287, p = 0.009) for the entire study sample. When stratified by gender, hs-CRP explained 7.1 % of the variation in BMI (β = 0.287, p = 0.042), 8.7 % of the variation in WC (β = 0.332, p = 0.023), and 11.3 % of the variation in WHtR (β = 0.376, p = 0.009) in females only.
Discussion
The main findings of our study were that hs-CRP associations were stronger with anthropometric indices in females than in males. These findings may be related to body fat differences between males and females. Females tend to have a higher percentage of body fat than males, regardless of equivalent amounts of liver and intra-abdominal fat (Westerbacka et al. 2004). In the TARF study, CRP levels were much higher in females as compared to males (Onat et al. 2011). Our results indicate that WHtR was a better measure than BMI, WC, WHR, weight, or HC for the association of hs-CRP levels in Turkish females with T2D. This finding confirms the findings of other cross-sectional studies (Can et al. 2009; Schneider et al. 2010). Results from the Turkish Heart Study suggest that WHtR is a better predictor of CVD risk as compared to BMI, WC, and WHR (Can et al. 2009). Schneider et al. (2010) observed similar findings, where WHtR was the strongest predictor of CVD risk and mortality and discouraged the use of BMI. Our study shows no significant difference in WHR in males or females with respect to hs-CRP levels. These findings are in accordance with other studies where WHR showed the weakest correlation with hs-CRP level in patients with T2D (Mojiminiyi et al. 2009). Connelly et al. (2003) found measures of total body fat (WC and BMI) were more strongly correlated with hs-CRP levels than measures of fat distribution including the WHR. Mojiminiyi et al. (2009) found gender-dependent differences in the pattern of fat distribution. Although some studies found BMI correlated with hs-CRP levels in patients with T2D more strongly as compared to other anthropometric measures (Mojiminiyi et al. 2009), our results revealed that BMI and WC have a weaker correlation with hs-CRP levels as compared to WHtR. The WHtR may be a more effective screening tool than WC, supporting the public health message ‘keep your waist circumference to less than half your height’ (Browning et al. 2010). WC and HC measure different patterns of body fat distribution, with independent effects on CVD, which could be poorly reflected in the WHR (Mojiminiyi et al. 2009). Research indicates that anthropometric measures of abdominal obesity are better indicators of CVD than BMI (de Koning et al. 2007; Schneider et al. 2010). The use of WHtR rather than WHR is recommended to assess CVD risk in Turkish adults (Can et al. 2009).
Various mechanisms have been suggested for the association between obesity and hs-CRP levels. Hs-CRP is synthesized by both the liver and adipose tissue in response to proinflammatory cytokines such as interleukin-6 (IL-6) (Anty et al. 2006). Consequently, both tissues may contribute to the elevated serum CRP levels found in obesity (Ujcic-Voortman et al. 2011; Anty et al. 2006). Elevated hs-CRP levels in females with T2D could be due to higher BMI and percentage of body fat (Flores-Alfaro et al. 2008; Al-Daghri et al. 2010). For persons with T2D, higher inflammatory stress in females than in males could contribute to females’ higher CVD risk (Saltevo et al. 2009). In the KORA study (Cooperative Research in the Region of Augsburg) a large proportion of the variation in hs-CRP levels was explained by body fatness and the association was particularly strong for females (Thorand et al. 2006).
Obesity accounts for only a portion of the variance of hs-CRP (Connelly et al. 2003). There are a number of other factors that have been found to affect hs-CRP levels including age, smoking, A1C, medications, alcohol and ethnicity (Ujcic-Voortman et al. 2011; Onat et al. 2008; Pai et al. 2006). Some of these factors may account for gender differences in obesity and hs-CRP. Turkish males have a higher prevalence of smoking as compared to Dutch males (Uitewaal et al. (2004b)). The TARF Study found smoking status to be a major determinant of elevated hs-CRP level in Turkish males independent of WC (Onat et al. 2008). Higher insulin resistance in relation to obesity may play a role in poor A1C status and can largely explain elevated hs-CRP level in patients with T2D (Onat et al. 2007). Previous studies have shown that certain medications including NSAIDs, LLD, angiotensin-converting enzyme (ACE) inhibitors, and diabetes medications, affect serum hs-CRP levels (Prasad 2006). Additionally, moderate alcohol consumption has shown an inverse association with hs-CRP levels (Pai et al. 2006). Due to the low prevalence of alcohol consumption in our study population, we did not include this as a covariate in our analysis. The TARF Study suggested that the association between hs-CRP levels and CVD might be even stronger for the Turkish population as compared to most Western populations (Onat et al. 2001).
Our study has several strengths. Participants included were all of Turkish origin, a single origin, in which research concerning hs-CRP level and measures of obesity is scarce. We used a standardized protocol, including uniform anthropometric and biochemical measurements in a clinical setting. Serum hs-CRP is a more sensitive assay for the prediction of CVD compared to traditional assays for circulating CRP levels (Pearson et al. 2003). Hs-CRP levels >10 mg/L reflect acute inflammation and were excluded from the analysis (Chou et al. 2010). NSAIDs, LLD, hypertension medications, diabetes medications, smoking and A1C, which might have influenced the association of hs-CRP levels, were controlled for in the analysis (Onat et al. 2008; Prasad 2006).
There were a number of limitations for this study. First, because of the study’s cross-sectional nature, our results do not establish causality. Second, these results cannot be generalized for other populations, since measures of obesity are known to be ethnic-specific. Third, given the small sample size (n = 93), these study findings need to be repeated in a larger sample to confirm our results.
Conclusion
The present study confirmed that gender differences exist in the association of anthropometric indices of obesity and hs-CRP levels for a Turkish sample with T2D. Among the measures examined, WHtR, WC, and BMI were independent determinants of serum hs-CRP level in females for a cohort with T2D. This relationship was not statistically significant for males. The association between hs-CRP level and WHtR in females is stronger than that of hs-CRP level with WC, BMI, weight or HC. Further studies are needed to confirm our results and to examine the factors of obesity that affect serum hs-CRP levels in Turkish immigrants with T2D. Prospective studies should be conducted to determine if changes in obesity results in differences in hs-CRP for populations with T2D. Research findings can contribute to the management of risk factors for CVD in Turkish patients with T2D. Adding hs-CRP testing to the protocol of standard diabetes care may prove beneficial for determining potential risk for CVD and may direct treatment in the primary prevention of CVD.
References
Al-Daghri, N. M., Al-Attas, O. S., Alokail, M. S., Alkharfy, K. M., Shaik, N. A., Draz, H. M., et al. (2010). Gender-specific associations between insulin resistance, hypertension, and markers of inflammation among adult Saudis with and without diabetes mellitus type 2. Advances in Medical Sciences, 55(2), 179–185.
Anty, R., Bekri, S., Luciani, N., Saint-Paul, M. C., Dahman, M., Iannelli, A., et al. (2006). The inflammatory C-reactive protein is increased in both liver and adipose tissue in severely obese patients independently from metabolic syndrome, Type 2 diabetes, and NASH. American Journal of Gastroenterology, 101(8), 1824–1833.
Bouma, M., Rutten, G. E., de Grauw, W. J., Wiersma, T., & Goudswaard, A. N. (2006). Nederlands Huisartsen Genootschap. Summary of the practice guideline ‘Diabetes mellitus type 2’ (second revision) from the Dutch College of General Practitioners. [Article in Dutch]. Nederlands Tijdschrift voor Geneeskunde, 150(41), 2251–2256.
Browning, L. M., Hsieh, S. D., & Ashwell, M. (2010). A systematic review of waist-to-height ratio as a screening tool for the prediction of cardiovascular disease and diabetes: 0·5 could be a suitable global boundary value. Nutrition Research Reviews, 23(2), 247–269.
Caan, B., Armstrong, M. A., Selby, J. V., Sadler, M., Folsom, A. R., Jacobs, D., et al. (1994). Changes in measurements of body fat distribution accompanying weight change. International Journal of Obesity and Related Metabolic Disorders, 18(6), 397–404.
Can, A. S., Bersot, T. P., Gönen, M., Pekcan, G., Rakıcıoğlu, N., Samur, G., et al. (2009). Anthropometric indices and their relationship with cardiometabolic risk factors in a sample of Turkish adults. Public Health Nutrition, 12(4), 538–546.
Can, A. S., Yildiz, E. A., Samur, G., Rakicioğlu, N., Pekcan, G., Ozbayrakçi, S., et al. (2010). Optimal waist: height ratio cut-off point for cardiometabolic risk factors in Turkish adults. Public Health Nutrition, 13(4), 488–495.
Centersfor Disease Control and Prevention. (2002). Cigarette smoking among adults—United States, 2000. Morbidity and Mortality Weekly Report, 51, 642–645.
Centraal Bureau voor de Statistiek. Turkse ingezetenen in Nederland 2011. (2012) Retrieved from: http://statline.cbs.nl/StatWeb/publication/?VW=T&DM=SLNL&PA=37325&D1=0&D2=a&D3=0&D4=0&D5=2-4,11,38,46,95-96,137,152,173,177,194,215,232&D6=0,4,8,12,l&HD=100209-1037&HDR=T,G2,G3,G5&STB=G1,G4.
Chou, H. H., Hsu, L. A., Liu, C. J., Teng, M. S., Wu, S., & Ko, Y. L. (2010). Insulin resistance is associated with C-reactive protein independent of abdominal obesity in nondiabetic Taiwanese. Metabolism, 59(6), 824–830.
Connelly, P. W., Hanley, A. J., Harris, S. B., Hegele, R. A., & Zinman, B. (2003). Relation of waist circumference and glycemic status to C-reactive protein in the Sandy Lake Oji-Cree. International Journal of Obesity and Related Metabolic Disorders, 27(3), 347–354.
Consensus Committee. (2007). Consensus statement on the worldwide standardization of the hemoglobin A1C measurement: the American Diabetes Association, European Association for the Study of Diabetes, International Federation of Clinical Chemistry and Laboratory Medicine, and the International Diabetes Federation. Diabetes Care, 30(9), 2399–2400.
de Koning, L., Merchant, A. T., Pogue, J., & Anand, S. S. (2007). Waist circumference and waist-to-hip ratio as predictors of cardiovascular events: meta-regression analysis of prospective studies. European Heart Journal, 28(7), 850–856.
Flores-Alfaro, E., Parra-Rojas, I., Salgado-Bernabé, A. B., Chávez-Maldonado, J. P., & Salazar-Martinez, E. (2008). Cardiovascular risk evaluated by C-reactive protein levels in diabetic and obese Mexican subjects. Circulation Journal, 72(7), 1170–1174.
Huffman, F. G., Gomez, G. P., & Zarini, G. G. (2009). Metabolic syndrome and high-sensitivity C-reactive protein in Cubans. Ethnicity & Disease, 19(2), 115–120.
Huffman, F. G., Whisner, S., Zarini, G. G., & Nath, S. (2010). Waist circumference and BMI in relation to serum high sensitivity C-reactive protein (hs-CRP) in Cuban Americans with and without type 2 diabetes. International Journal of Environmental Research and Public Health, 7(3), 842–852.
Kriegsman, D., van Langen, J., Valk, G., Stalman, W., & Boeke, J. (2003). Hoge prevalentie van diabetes mellitus type 2 bij Turken and Marokkanen. Huisarts & Wetenschap, 46(7), 363–368.
Lolekha, P. H., Chittamma, A., Roberts, W. L., Sritara, P., Cheepudomwit, S., & Suriyawongpaisal, P. (2005). Comparative study of two automated high-sensitivity C-reactive protein methods in a large population. Clinical Biochemistry, 38(1), 31–35.
Mojiminiyi, O. A., Al Mulla, F., & Abdella, N. A. (2009). Which obesity index best explains the link between adipokines, coronary heart disease risk and metabolic abnormalities in type 2 diabetes mellitus? Medical Principles and Practice, 18(2), 123–129.
Onat, A., Sansoy, V., Yildirim, B., Keleş, I., Uysal, O., & Hergenç, G. (2001). C-reactive protein and coronary heart disease in western Turkey. The American Journal of Cardiology, 88(6), 601–607.
Onat, A., Uyarel, H., Hergenç, G., Karabulut, A., Albayrak, S., & Can, G. (2007). Determinants and definition of abdominal obesity as related to risk of diabetes, metabolic syndrome and coronary disease in Turkish men: a prospective cohort study. Atherosclerosis, 191(1), 182–190.
Onat, A., Can, G., & Hergenç, G. (2008). Serum C-reactive protein is an independent risk factor predicting cardiometabolic risk. Metabolism, 57(2), 207–214.
Onat, A., Can, G., Hergenç, G., Uğur, M., & Yüksel, H. (2011). Coronary disease risk prediction algorithm warranting incorporation of C-reactive protein in Turkish adults, manifesting sex difference. Nutrition, Metabolism, and Cardiovascular Diseases. doi:10.1016/j.numecd.2010.10.010.
Pai, J. K., Hankinson, S. E., Thadhani, R., Rifai, N., Pischon, T., & Rimm, E. B. (2006). Moderate alcohol consumption and lower levels of inflammatory markers in US men and women. Atherosclerosis, 186(1), 113–120.
Pearson, T. A., Mensah, G. A., Alexander, R. W., Anderson, J. L., Cannon, R. O., III, Criqui, M., et al. (2003). Markers of inflammation and cardiovascular disease: application to clinical and public health practice: a statement for healthcare professionals from the Centers for Disease Control and Prevention and the American Heart Association. Circulation, 107(3), 499–511.
Pickup, J. C. (2004). Inflammation and activated innate immunity in the pathogenesis of type 2 diabetes. Diabetes Care, 27(3), 813–823.
Prasad, K. (2006). C-reactive protein (CRP)-lowering agents. Cardiovascular Drug Reviews, 24(1), 33–50.
Saltevo, J., Kautiainen, H., & Vanhala, M. (2009). Gender differences in adiponectin and low-grade inflammation among individuals with normal glucose tolerance, prediabetes, and type 2 diabetes. Gender Medicine, 6(3), 463–470.
Schneider, H. J., Glaesmer, H., Klotsche, J., Böhler, S., Lehnert, H., Zeiher, A. M., et al. (2007). Accuracy of anthropometric indicators of obesity to predict cardiovascular risk. Journal of Clinical Endocrinology and Metabolism, 92(2), 589–594.
Schneider, H. J., Friedrich, N., Klotsche, J., Pieper, L., Nauck, M., John, U., et al. (2010). The predictive value of different measures of obesity for incident cardiovascular events and mortality. Journal of Clinical Endocrinology and Metabolism, 95(4), 1777–1785.
Snijder, M. B., Dekker, J. M., Visser, M., Stehouwer, C. D., Yudkin, J. S., Bouter, L. M., et al. (2003). Prospective relation of C-reactive protein with type 2 diabetes: response to Han et al. Diabetes Care, 26(5), 1656–1657. author reply 1657–1658.
Soinio, M., Marniemi, J., Laakso, M., Lehto, S., & Rönnemaa, T. (2006). High-sensitivity C-reactive protein and coronary heart disease mortality in patients with type 2 diabetes: a 7-year follow-up study. Diabetes Care, 29(2), 329–333.
Thorand, B., Baumert, J., Döring, A., Schneider, A., Chambless, L., Löwel, H., et al. (2006). Association of cardiovascular risk factors with markers of endothelial dysfunction in middle-aged men and women. Results from the MONICA/KORA Augsburg Study. Journal of Thrombosis and Haemostasis, 95(1), 134–141.
Uitewaal, P. J., Goudswaard, A. N., Ubink-Veltmaat, L. J., Bruijnzeels, M. A., Hoes, A. W., & Thomas, S. (2004). Cardiovascular risk factors in Turkish immigrants with type 2 diabetes mellitus: comparison with Dutch patients. European Journal of Epidemiology, 19(10), 923–929.
Uitewaal, P. J., Manna, D. R., Bruijnzeels, M. A., Hoes, A. W., & Thomas, S. (2004). Prevalence of type 2 diabetes mellitus, other cardiovascular risk factors, and cardiovascular disease in Turkish and Moroccan immigrants in North West Europe: a systematic review. Preventive Medicine, 39(6), 1068–1076.
Ujcic-Voortman, J. K., Baan, C. A., Verhoeff, A. P., Krol, A., & Seidell, J. C. (2011). Ethnic differences in systemic inflammation: an investigation of C-reactive protein levels among Moroccan, Turkish and Dutch groups in the Netherlands. Atherosclerosis, 218(2), 511–516.
van Leest, L. A. T. M., van Dis, S. J. & Verschuren, W. M. M. (2002). Hart- en vaatziekten bij allochtonen in Nederland. Een cijfermatige verkenning naar leefstijl- en risicofactoren, ziekte en sterfte. RIVM Rapport Bilthoven (The Dutch National Institute for Public Health and the Environment).
Westerbacka, J., Cornér, A., Tiikkainen, M., Tamminen, M., Vehkavaara, S., Häkkinen, A. M., et al. (2004). Women and men have similar amounts of liver and intra-abdominal fat, despite more subcutaneous fat in women: implications for sex differences in markers of cardiovascular risk. Diabetologia, 47(8), 1360–1369.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Sukhram, S.D., Zarini, G.G., Shaban, L.H. et al. Obesity and Serum High Sensitivity C-Reactive Protein Levels Among Elderly Turkish Immigrants in the Netherlands with Type 2 Diabetes. Ageing Int 39, 68–80 (2014). https://doi.org/10.1007/s12126-012-9149-0
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12126-012-9149-0