Abstract
Objective
To compare long-term neurodevelopmental and growth (NDG) outcomes at 3 y corrected gestational age (GA) in premature infants with grade ≥ III intraventricular hemorrhage (IVH) and post-hemorrhagic hydrocephalus who were treated with ventriculo-peritoneal shunt with those who were not treated with shunt.
Methods
In a retrospective cohort study, NDG outcomes were compared between preterm infants of <29 wk GA with IVH treated with shunt (IVHS) and IVH with no shunt (IVHNS). This was a single centre study. The primary outcome was moderate to severe cerebral palsy (CP).
Results
Of 1762 preterm infants who survived to discharge, 90 had grade ≥ III IVH. Infants in IVHS group had more grade IV IVH than IVHNS (p < 0.05). Seventy percent of the patients in IVHNS groups had no hydrocephalus. IVHS group had increased CP (76% vs. 30%; p 0.003), and higher odds of CP after controlling for GA and IVH grade [odds ratio (OR); 4.23 (1.38 to 13.00)]. Growth delay was not different between groups.
Conclusions
Infants with IVHS are at increased risk of CP but not growth delay.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
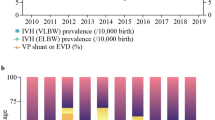
Advances in neonatal intensive care unit (NICU) have resulted in significant improvement in the survival of extremely preterm infants [1]. Intraventricular hemorrhage (IVH) of any severity is a major complication in preterm infants but severe IVH (grade III-IV) can lead to serious adverse neurological outcomes [2, 3]. The incidence of severe IVH in preterm infants weighing ≤1250 g at birth is 25% compared to 3% in infants weighing 1250–1500 g at birth [4].
Post-hemorrhagic hydrocephalus (PHH) occurs in 1/3rd of infants with severe IVH [5]. It is characterized by an enlargement of both head and ventricular system based on ultrasound scans [6]. Ventricular dilatation following severe IVH in preterm infants may lead to significant neurodevelopmental disability (NDD) at 12 mo and 18–24 mo corrected gestational age (CGA). Raised intracranial pressure with periventricular edema and distortion of the developing axonal pathways contributes to the development of NDD [2, 3]. Furthermore, 15–25% of infants with severe IVH and PHH eventually need a ventriculo-peritoneal shunt (VP shunt) because of continued progression in ventricular size [7–9].
To date, most of the long-term NDD data on infants with severe IVH and ventricular dilatation who required shunts are available either in small case-series from the 1980s and are restricted to 18–24 mo CGA [7–13]. There is paucity of data regarding longer-term neurodevelopmental outcomes of infants with IVH treated with VP shunts at 3 y CGA. The objective of present study was to compare the long-term neurodevelopmental and growth outcomes at 3 y CGA in preterm infants born at <29 wk gestational age (GA) with severe IVH (grade ≥ III) and PHH treated with VP shunt to those who did not.
Material and Methods
All surviving preterm infants (< 29 wk of GA at birth) born between January 1990 and December 2007, admitted to a regional tertiary care NICU at Foothills Medical Centre in Calgary, Alberta and followed-up at the neonatal follow-up clinic (NFC) were eligible for the study. Infants with congenital malformations and chromosomal anomalies were excluded from the study. The Conjoint Health Research Ethics Board of the University of Calgary approved this study.
All cranial ultrasound scans during the first 2 wk of life were reviewed by radiologists and the scan with the highest graded injuries were entered into the NFC database. NICU data were collected retrospectively but neurodevelopmental and growth outcome data were collected prospectively by trained data abstractors and entered into the NFC database on a weekly ongoing basis. Neonatal and follow-up data for all eligible infants were obtained from NFC and additional data about the progression and complications of IVH, timing and type of surgical intervention for PHH were collected from the patients’ charts and entered into a computerized database. Infants with severe IVH were identified and classified into two groups: IVH with VP shunting (IVHS) and IVH with no shunt (IVHNS). During the study period, there was no standard practice or consensus for interventions in cases of PHH. The diagnosis of PHH and intervention was usually based on progression of the hydrocephalus and neurological assessment, more specifically when ventricular size, measured at the level of the foramen of Monro reached 4 mm above the 97th centile for GA.
The maternal, perinatal and neonatal characteristics and outcomes were compared between the groups. Preterm infants were seen at 4, 8, 18 mo and 3 y CGA in the NFC. Neurodevelopmental assessments and growth measurements were carried out by a multidisciplinary team consisting of neonatologists or developmental pediatricians, psychologist, audiologist, physiotherapist and an ophthalmologist.
The primary outcome was the presence of moderate to severe cerebral palsy (CP) at 3 y CGA. NDD was considered present if a child had any of the following: moderate to severe CP, cognitive score > 2 SD below the mean, bilateral hearing loss requiring amplification or cochlear implants and bilateral blindness with corrected visual acuity <20/200 in the better eye diagnosed up to 3 y CGA. The secondary outcome included growth delay (head circumference, length and weight) less than 5th centile at 3 y CGA based on the Centre for Disease Control and Prevention (CDC 2000) growth curves (www.cdc.gov/growthcharts) [14].
The diagnosis of IVH and its severity was based on Papile’s criteria on cranial ultrasound (CUS) findings [15]. Respiratory distress syndrome (RDS) was defined as the presence of respiratory distress, chest X-ray findings consistent with RDS and/or requiring treatment with surfactant [16]. Bronchopulmonary dysplasia (BPD) was defined as need for supplemental oxygen or any form of assisted ventilation at 36 wk postmenstrual age [17]. Diagnosis of patent ductus arteriosus (PDA) was made clinically with or without echocardiography [16]. Sepsis was defined as blood or cerebrospinal fluid culture positive for a single organism during the hospital stay [16]. Small for gestational age (SGA) at birth was defined as birth weight < 10th percentile for gestational age [16].
Cerebral palsy refers to a non-progressive disability of movement and posture and was diagnosed on the basis of abnormal muscle tone and reflexes on the physical and neurological examination. Moderate to severe CP was defined as motor dysfunction treated with appliances or assistance with performance of daily activities and functions [18]. Cognitive delay was defined as cognitive score > 2 SD below the mean on the Wechsler Preschool and Primary Scale of Intelligence, Third Edition (WPPSI-III) or the Standford-Binet Intelligence Test, Fourth Edition (SB-IV). Blindness was defined as bilateral blindness with corrected visual acuity of <20/200 in the better eye. Deafness was defined as a bilateral sensorineural loss requiring amplification or cochlear implants.
The sample chosen was based on selecting the birth years with 3-y outcome data available in the NFC database. Based on a previous study [7], the rate of CP at 18–22 mo of age in infants with severe IVH without shunt is 28% and severe IVH with shunt is 70%. A sample size of 22 infants in each group would be required to find a difference in the proportion of CP of 42% between severe IVH with no shunt and severe IVH with shunt, at 80% power and alpha level of 0.05 [19]. The present study had 26 infants in the IVHS group and 50 infants in the IVHNS group, which is adequate to detect a difference of this size.
Baseline characteristics and outcomes were compared between the two groups using chi-square tests for categorical variables, and t-test for normally distributed continuous variables or Mann-Whitney U test for non-normally distributed continuous variables. Logistic regression was used to examine the effect of shunt (IVHS group) vs. no shunt (IVHNS group) on moderate to severe CP. The present sample size allowed to include a maximum of three variables at a time in the model. The authors included VP shunt and GA at birth in the model, then added other risk factors one at a time to determine whether the association between shunt and CP would be modified with these other potential confounders. The risk factors tested were: IVH grade, dexamethasone use in BPD, retinopathy of prematurity (ROP), sepsis and necrotizing enterocolitis (NEC), chosen based on clinical importance as risk factors for NDD. SAS 9.3 (SAS Institute, Cary, NC, USA) statistical software was used for the statistical analysis.
Results
A total of 2108 preterm infants were admitted to NICU, of which 1762 (83.5%) infants survived to discharge. A flow diagram of the study population is shown in Fig. 1. Among the infants who survived to discharge, 90 had severe IVH. Of these, 5 subjects were excluded; 4 with major congenital anomaly (Trisomy 21, Goldenhaur syndrome, Dandy -Walker syndrome and multiple congenital anomalies) and one died after discharge.
Eighteen (69.2%) children in IVHS group received temporising surgical measures (ventricular access device and/or ventriculosubgaleal shunts) before permanent VP shunting. The mean age of VP shunting was 143 d (earliest at 29 d and as late as 3 y). Fifteen infants in IVHNS group had arrested hydrocephalus but did not require shunt surgery. In IVHNS group, 35 infants did not have any evidence of hydrocephalus. The maternal and neonatal characteristics were similar in the two groups of this study (Table 1). Neonatal outcomes are shown in Table 2. A higher proportion of infants in the IVHS group had grade IV IVH than infants in the IVHNS group (p < 0.05) (Table 2).
Three children (11.5%) in the IVHS group had a single episode of meningitis before any surgical intervention (Escherichia coli, n = 2, Haemophilus influenzae, n = 1) and they did not develop meningitis post shunting. The present study did not find any difference in the incidence of sepsis between the two groups. In terms of complications, seven children with VP shunt (27%) had meningitis (culture positive cerebro-spinal fluid). Of these 3/7 (43%) had two episodes while 4/7 (57%) had ≥3 episodes of meningitis prior to follow-up visit at 3 y CGA. The common organisms identified in cerebrospinal fluid were Coagulase-negative staphylococci (n = 5), Staphylococcus aureus (n = 2), Rothia mucilaginosa (n = 1), Enterococcus (n = 1), N. meningitidis (n = 1), E. coli (n = 2), H. influenzae (n = 1) and Propionibacterium acnes (n = 5). All children in IVHS group required revision of shunt at least once. Eight children required revision of shunts >2 times.
The neurodevelopmental and growth outcomes are shown in Table 3. Forty-four (58%) children with severe IVH had at least one of the severe disabilities at 3 y CGA. Thirty-two (42%) had moderate to severe CP (76% in IVHS vs. 30% in IVHNS groups; p 0.004), 9 (12%) had blindness and deafness was diagnosed in 2 (2.6%). All seven children with shunt infection were diagnosed with moderate to severe CP. Of three children who had meningitis before surgery, one had severe NDD, 1 had moderate NDD and 1 had normal outcomes at 3 y CGA. After excluding cases of shunt infection, children with shunt and no shunt infection did not show a statistically significant higher rate of CP than those without shunt (53% IVHS vs. 30% IVHNS, p 0.081). The results of the logistic regression models exploring the association between IVHS/IVHNS and moderate to severe CP are shown in Table 4. After controlling for IVH grade and gestational age, the IVHS group had higher odds of moderate to severe CP as compared to the IVHNS group (OR: 4.23; 95% CI: 1.38 to 13.00). The present study did not find any difference in the postnatal growth between the groups (Table 3).
Discussion
The present study showed that preterm infants with severe IVH and PHH treated with a VP shunt were at higher risk of developing CP at 3 y CGA compared to the infants in IVHNS group.
Preterm children who required surgery for PHH had adverse neurodevelopmental outcomes mainly CP possibly due to pressure effects of hydrocephalus and parenchymal hemorrhagic injury [2, 6]. This finding is similar to present findings. Boynton et al. reported neurodevelopmental outcomes in 50 preterm infants with VP shunting at 2 y age [8]. Severe motor handicap was observed in almost half of the infants and CP in 70% infants [8]. A recent study, published by Srinivasakumar et al. showed that posthemorrhagic ventricular dilatation has significant adverse impact on motor and cognitive outcomes in preterm infants born ≤ 34 wk GA at 18 to 24 mo [11]. Brouwer et al., in a case-control study did not observe any difference in the risk of neurodevelopmental impairment or CP in 23 infants with severe IVH at the age of five and 8 y who required VP shunting for PHH and those who did not [20]. In PHH, enlarging ventricles have an impact on corticospinal tracts, cortico-cortical and cortico-fugal connectivity in the white matter [21, 22] and poor inter-hemispheric connection resulting from damage to the corpus callosum; [22] both of which are postulated to be important in the cause of cognitive impairment [22]. Other possible mechanisms for cerebral white matter injury include increasing cerebral vascular resistance, decreasing cerebral perfusion and compression of brain parenchyma causing damage to the periventricular white matter leading to hypoxic ischemic injury [6, 23].
In the index study, when patients with a history of cerebrospinal fluid (CSF) culture positive shunt infection were removed, no difference in the rate of CP in shunted children was identified as compared with those without shunt. The present finding is consistent with Brouwer et al.’s study [20]. A high proportion of index patients had insertion of a temporizing ventricular reservoir prior to definitive shunt insertion that may have played a role in the development of subsequent CSF infection. Meningitis in preterm infants has a detrimental effect on long-term neurodevelopmental outcomes [24]. VP shunts are associated with many complications including infection, which occurs in 10% of patients [25]. It is recognised that shunt infection remains as an additional potential risk factor for adverse outcomes. This needs further study to explore the risk of NDD in children with VP shunting in PHH and meningitis.
The index study did not observe any difference in cognitive delay, blindness and deafness at 3 y CGA. The present finding is consistent with Brouwer et al. study [20]. In contrast to present results, Adams-Chapman et al. study reported significant cognitive delay and blindness in the shunted group but no difference in deafness at 18–22 mo CGA [7]. However, the predictive value of neurodevelopmental outcomes at an early age has been debated in the literature; outcomes may change over a period of time as children grow; low general cognitive index scores may show improvement, some minor sequelae may manifest at later age or some remain unchanged [26]. Fazzi et al. also noted many of the minor sequelae becoming more evident at 5 to 7 y of age, thus stressing the need for long-term follow-up and cautioning against predicting an outcome on the basis of low general cognitive index score in early infancy [26]. As the present single-centre cohort was smaller compared to the study by Adams-Chapman et al. [7], it may not have been possible for the present study to detect small differences in less common outcome like blindness.
The present study did not find any significant difference in growth impairment between the two groups. In contrast to present study results, children with CP are at increased risk of poor growth and lower Z-score [7, 27] due to immature oral-motor organization, sucking and swallowing problems, regurgitation, coughing and choking during feeding and oral motor dysfunction [28]. Despite disproportionately increased number of CP in the shunted group, growth impairment was comparable between the two groups.
Cranial ultrasound was done on all infants involved in the study. CUS is the primary imaging modality for the screening and diagnosis of IVH and PHH [29]. The advantages of cranial ultrasound scanning include: safely done at the bedside even if the infant is critically ill, no adverse effects like radiations, less expensive, does not need transportation and no risk of hypothermia [30]. It is evident that ultrasound provides a convenient, non-invasive, safe and reliable method of measuring ventricular size [30]. In the present study, mostly infants in the surgical group had advanced neuroimaging like CT (computed tomography) scanning and MRI (magnetic resonance imaging) as a supplementary tool to diagnose other neurological conditions before and or after surgery. Presently, MRI is a commonly used advanced neuroimaging modality as a supplementary tool in the stable premature infants with PHH after cranial ultrasound scanning between corrected age of term gestation to 3 y of corrected age [29].
The strengths of index study include long term follow-up at 3 y CA based on prospectively collected follow-up data with a high follow-up rate (89%). As a single centre cohort at a regional NICU, the risk of variability in the management of PHH is likely to be less compared to multi-centre studies. The present study has some limitations including a small cohort of preterm infants who required surgery for PHH. The authors’ database did not have detailed information about CT/MRI scans on the infants who had surgical interventions. All assessors in the authors’ neonatal follow-up clinic were not blinded at the time of assessment and the retrospective nature of the study may introduce some bias. Important radiological features in PHH; including laterality, the size of severe IVH and related ventricular size were not routinely documented or collected for this study. During the study period, the Gross Motor Function Classification System (GMFCS) was not used in the follow-up clinic to classify severity of CP.
In conclusion, PHH needing shunt surgery is associated with an increased risk of moderate to severe CP in preterm infants born at <29 wk gestational age. The present study emphasizes the significance of long-term follow-up of infants with PHH needing VP shunt surgery with or without meningitis and assists clinicians while counseling parents of preterm infants with severe IVH and PHH. In the absence of randomised control trials to assess the effectiveness of various surgical interventions in PHH and long-term outcomes in premature infants, the authors recommend that there is a need for multicentre prospective data collection to acquire adequate numbers in order to determine best practices and longer-term neurodevelopmental follow-up information at school age in infants with IVH and PHH.
References
Guillen U, Weiss EM, Munson D, et al. Guidelines for the management of extremely premature deliveries: a systematic review. Pediatrics. 2015;136:343–50.
Volpe JJ. Intracranial hemorrhage: subdural, primary subarachnoid, cerebellar, intraventricular (term infant), and miscellaneous. In: Volpe JJ, editor. Neurology of the newborn. 5th ed. Philadelphia, PA: Saunders Elsevier; 2008. p. 483–516.
Bolisetty S, Dhawan A, Abdel-Latif M, et al. Intraventricular hemorrhage and neurodevelopmental outcomes in extreme preterm infants. Pediatrics. 2014;133:55–62.
Lemons JA, Bauer CR, Oh W, et al. Very low birth weight outcomes of the National Institute of child health and human development neonatal research network, January 1995 through December 1996. NICHD Neonatal Research Network. Pediatrics. 2001;107:E1.
Wellons JC, Shannon CN, Kulkarni AV, et al. A multicenter retrospective comparison of conversion from temporary to permanent cerebrospinal fluid diversion in very low birth weight infants with posthemorrhagic hydrocephalus. J Neurosurg Pediatr. 2009;4:50–5.
Whitelaw A, Cherian S, Thoresen M, Pople I. Posthaemorrhagic ventricular dilatation: new mechanisms and new treatment. Acta Paediatr Suppl. 2004;93:11–4.
Adams-Chapman I, Hansen NI, Stoll BJ, Higgins R, Network NR. Neurodevelopmental outcome of extremely low birth weight infants with posthemorrhagic hydrocephalus requiring shunt insertion. Pediatrics. 2008;121:e1167–77.
Boynton BR, Boynton CA, Merritt TA, Vaucher YE, James HE, Bejar RF. Ventriculoperitoneal shunts in low birth weight infants with intracranial hemorrhage: neurodevelopmental outcome. Neurosurgery. 1986;18:141–5.
Goldstein RF, Cotten CM. Shankaran S, Gantz MG, Poole WK; Eunice Kennedy Shriver National Institute of Child Health and Human Development Neonatal Research Network. Influence of gestational age on death and neurodevelopmental outcome in premature infants with severe intracranial hemorrhage. J Perinatol. 2013;33:25–32.
O'Shea TM, Allred EN, Kuban KC, et al. Intraventricular hemorrhage and developmental outcomes at 24 months of age in extremely preterm infants. J Child Neurol. 2012;27:22–9.
Srinivasakumar P, Limbrick D, Munro R, et al. Posthemorrhagic ventricular dilatation-impact on early neurodevelopmental outcome. Am J Perinatol. 2013;30:207–14.
Tsai AJ, Lasky RE, John SD, Evans PW, Kennedy KA. Predictors of neurodevelopmental outcomes in preterm infants with intraparenchymal hemorrhage. J Perinatol. 2014;34:399–404.
van Zanten SA, de Haan TR, Ursum J, van Sonderen L. Neurodevelopmental outcome of post-hemorrhagic ventricular dilatation at 12 and 24 months corrected age with high-threshold therapy. Eur J Paediatr Neurol. 2011;15:487–92.
Kuczmarski R, Ogden C, Grummer-Strawn L, et al. CDC growth charts: United States. Advance data from vital and health statistics, no.314. Hyattsville, Maryland: National Center for Health Statistics; 2000.
Papile LA, Burstein J, Burstein R, Koffler H. Incidence and evolution of subependymal and intraventricular hemorrhage: a study of infants with birth weights less than 1,500 gm. J Pediatr. 1978;92:529–34.
Lodha A, Zhu Q, Lee SK. Shah PS; Canadian Neonatal Network. Neonatal outcomes of preterm infants in breech presentation according to mode of birth in Canadian NICUs. Postgrad Med J. 2011;87:175–9.
Shennan AT, Dunn MS, Ohlsson A, Lennox K, Hoskins EM. Abnormal pulmonary outcomes in premature infants: prediction from oxygen requirement in the neonatal period. Pediatrics. 1988;82:527–32.
Russman BS, Gage JR. Cerebral palsy. Curr Probl Pediatr. 1989;19:65–111.
Lenth R. Java Applets for Power and Sample Size (Computer software) 2006–9. Available at: http://www.stat.uiowa.edu/~rlenth/Power. Accessed on 15th June 2012.
Brouwer AJ, van Stam C, Uniken Venema M, Koopman C, Groenendaal F, de Vries LS. Cognitive and neurological outcome at the age of 5-8 years of preterm infants with post-hemorrhagic ventricular dilatation requiring neurosurgical intervention. Neonatology. 2012;101:210–6.
Ment LR, Vohr B, Allan W, et al. The etiology and outcome of cerebral ventriculomegaly at term in very low birth weight preterm infants. Pediatrics. 1999;104:243–8.
Stewart A, Kirkbride V. Very preterm infants at fourteen years: relationship with neonatal ultrasound brain scans and neurodevelopmental status at one year. Acta Paediatr Suppl. 1996;416:44–7.
Cherian S, Whitelaw A, Thoresen M, Love S. The pathogenesis of neonatal post-hemorrhagic hydrocephalus. Brain Pathol. 2004;14:305–11.
Doctor BA, Newman N, Minich NM, Taylor HG, Fanaroff AA, Hack M. Clinical outcomes of neonatal meningitis in very-low birth-weight infants. Clin Pediatr (Phila). 2001;40:473–80.
Mantovani JF, Pasternak JF, Mathew OP, et al. Failure of daily lumbar punctures to prevent the development of hydrocephalus following intraventricular hemorrhage. J Pediatr. 1980;97:278–81.
Fazzi E, Orcesi S, Telesca C, Ometto A, Rondini G, Lanzi G. Neurodevelopmental outcome in very low birth weight infants at 24 months and 5 to 7 years of age: changing diagnosis. Pediatr Neurol. 1997;17:240–8.
Dahl M, Gebre-Medhin M. Feeding and nutritional problems in children with cerebral palsy and myelomeningocoele. Acta Paediatr. 1993;82:816–20.
Gangil A, Patwari AK, Aneja S, Ahuja B, Anand VK. Feeding problems in children with cerebral palsy. Indian Pediatr. 2001;38:839–46.
Blankenberg FG, Norbash AM, Lane B, Stevenson DK, Bracci PM, Enzmann DR. Neonatal intracranial ischemia and hemorrhage: diagnosis with US, CT, and MR imaging. Radiology. 1996;199:253–9.
Robinson S. Neonatal posthemorrhagic hydrocephalus from prematurity: pathophysiology and current treatment concepts. J Neurosurg Pediatr. 2012;9:242–58.
Acknowledgements
The authors thank Ms. Michelle Mathews for abstraction of data and entry into the database. The authors also thank Swasti Lodha and Ajay Sahai for their editorial comments.
Contributions
All authors contributed to study design, data acquisition and writing the manuscript. AL will act as guarantor for the paper.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of Interest
None.
Source of Funding
None.
Rights and permissions
About this article
Cite this article
Diwakar, K., Hader, W.J., Soraisham, A. et al. Long-Term Neurodevelopmental and Growth Outcomes of Premature Infants Born at <29 week Gestational Age with Post-Hemorrhagic Hydrocephalus Treated with Ventriculo-Peritoneal Shunt. Indian J Pediatr 84, 662–669 (2017). https://doi.org/10.1007/s12098-017-2319-z
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12098-017-2319-z