Abstract
Objectives
To assess the efficacy and safety of 10-d sequential therapy compared to 5 to 14-d triple therapy for treating Helicobacter pylori infections in children according to the eradication rates.
Methods
The Cochrane Library, MEDLINE, EMBASE, China National Knowledge Infrastructure databases, and other sources were searched in November 2014 without language restrictions. Randomized controlled trials (RCTs) that compared sequential therapy with triple therapy for H. pylori eradication in children were included. Dichotomous data were pooled to obtain the relative risk (RR) of the eradication rate with a 95 % confidence interval (CI).
Results
Fourteen RCTs with 1698 participants (718 and 980 for sequential and triple therapy, respectively) were included. The intention-to-treat eradication rates were 73 % (95 % CI: 70–76) and 66 % (95 % CI: 64–70) for sequential and triple therapy, respectively. The pooled RR was 1.16 (95 % CI: 1.09–1.23), resulting in a number needed to treat of 16 (95 % CI: 10–48), favoring sequential therapy. Sequential therapy was superior to 7- and 10-d triple therapy. Sequential and triple therapy did not differ significantly in the overall risk of adverse effects.
Conclusions
In children, sequential therapy appears to be superior to triple therapy for H. pylori eradication, although the eradication rates remain lower than the expected goal with both treatments. Factors-associated with a higher risk of eradication failure, such as compliance and antimicrobial resistance, remain insufficiently investigated. Therefore, further high-quality RCTs are needed to compare these different eradication treatment approaches.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Helicobacter pylori is a highly prevalent chronic infectious pathogen in children, which can lead to chronic gastritis, atrophic gastritis, intestinal metaplasia, and a diverse spectrum of extra-gastric disorders [1, 2]. The successful eradication of H. pylori can dramatically reduce the rate of recurrence of peptic ulcers in children [3, 4]. Proton pump inhibitor (PPI)- based triple therapy has been recommended as a first-line eradication treatment in combination with an amoxicillin plus nitroimidazole regimen or an amoxicillin plus clarithromycin regimen for 7–14 d [5]. However, recently, the success of eradication using triple therapy has unexpectedly declined [1, 6]. Zullo et al. initially proposed a novel sequential treatment regimen for H. pylori infection, consisting of 5 d of treatment with a PPI and a single antibiotic (usually amoxicillin), followed by 5 d of treatment with a PPI and two different antibiotics (usually clarithromycin and nitroimidazole) [5, 7]. Two meta-analyses [8, 9] were performed to assess the efficacy of sequential therapy (ST) compared to triple therapy (TT) in children, and one of the two meta-analyses was later updated by their group [10].
The authors performed a review to compare the effect of a 10-d ST and TT on the H. pylori eradication rates in children; some new randomized controlled trials (RCTs) have been included to update and further consolidate previous findings.
Material and Methods
This meta-analysis followed the guidelines from the Cochrane Handbook for Systematic Reviews of Interventions [11] and the meta-analyses (PRISMA) statement [12].
Included studies had to meet the following criteria using the PICOS approach: (i) Participants: children aged below 18 y who had H. pylori infection, confirmed using generally accepted methods (i.e., bacterial culture, 13C-urea breath test [13C-UBT], histopathology, H. pylori stool antigen test, blood test, or rapid urease test); (ii) Intervention: ST; (iii) Comparison: TT; and (iv) Primary outcome: The H. pylori eradication rate, which was determined by a negative 13C-UBT or other generally accepted methods by at least 4 wk post-treatment; Secondary outcomes: The rate of side effects (e.g., abdominal pain, nausea, vomiting, diarrhea, taste disturbance, and constipation), compliance, and the need to discontinue H. pylori therapy; and (v) Study design: RCTs.
The authors performed an electronic search to identify relevant studies from the following databases in November 2014: The Cochrane Central Register of Controlled Trials, MEDLINE, EMBASE, and China National Knowledge Infrastructure database. There was no language restriction, and the principal search text word terms and medical subject headings used were as follows: (i) Helicobacter pylori OR H. pylori; (ii) sequential treatment OR sequential therapy; (iii) children OR adolescents. The sets of terms (i), (ii), and (iii) were combined with “AND” operator. The reference lists from the included studies and key review articles were reviewed to identify other published or unpublished data that could be included.
In a double-blinded separate manner, two investigators (YH and XZ) performed the search, selected the studies, and performed quality assessment and data extraction using a pre-defined and standardized collection form to increase uniformity and reduce reporting bias. From each report, reviewers extracted basic information, details of treatment, confirming method for H. pylori infection, and side effects. The corresponding authors of the included studies were contacted for any missing data points. Any disagreements were resolved by a consensus decision between the two reviewers.
The Cochrane Collaboration’s tool for assessing the risk of bias was used, which includes the following specific domains: Adequacy of sequence generation, allocation concealment and blinding of participants, personnel and outcome assessors, and incomplete outcome data. “Yes” indicates a low risk of bias, and “No” indicates a high risk of bias [13]. In addition, the authors assessed the presence of publication bias by visually inspecting funnel plot asymmetry and by applying Egger’s test [14] for asymmetry.
The primary outcome was the relative risk (RR) of successful eradication of H. pylori based on intention-to-treat (ITT) when comparing ST to TT. Preplanned subgroup analyses were performed based on the duration of TT (5, 7, 10, or 14 d). The authors also performed subgroup analyses to compare the findings of RCTs available as full-text publications with those reported in abstract form only. The secondary outcome measures were the RR of side effects.
Heterogeneity was assessed by the I 2 statistic, which can be interpreted as the percentage of the observed variation between included studies that is attributable to heterogeneity rather than to chance. Values of 25, 50, and 75 % were used as outer limits for low, moderate and high heterogeneity, respectively [15]. If the I 2 value was >50 %, heterogeneity was considered to be significant. When there was a statistically significant heterogeneity of the primary outcome between studies, sensitivity analyses were performed to evaluate the differences in the quality of trials, resistance to clarithromycin, adherence, etc.
All the RRs were pooled using the fixed effects model (Mantel-Haenszel method), and a two-sided P value ≤0.05 was regarded as significant. Where significant heterogeneity was detected, a random effect model was additionally assessed, if appropriate. The data were analyzed using Review Manager (version 5.2; The Nordic Cochrane Center, The Cochrane Collaboration, 2011, Copenhagen, Denmark). The number needed to treat (NNT), with a 95 % confidence interval (CI) and the Egger’s test, were calculated using the StatsDirect statistical software (version 2.7.9; StatsDirect, Altrincham, UK).
Results
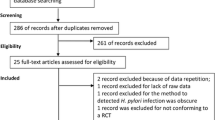
A flow diagram illustrating the study retrieval method is shown in Fig. 1. Of the 104 potentially relevant studies, 14 RCTs were included in this meta-analysis [16–29]. Ten of 14 were full-text publications [16, 19, 21, 23–29], and four were published in abstract form [17, 18, 20, 22]. All the trials were published in English, except for three publications in Chinese [19, 24, 25]. The characteristics of the included studies are summarized in Table 1.
The selected trials included 1,698 randomized participants aged below 18 y. The sample sizes ranged 30–360 participants. The studies were performed in European countries (Belgium, France, Italy, Poland, Romania, and Turkey), Asia (China), and Africa (Kenya). Except for two multicenter trials [21, 26], all the studies were single-center trials.
The TT consisted of a PPI (Omeprazole or lansoprazole) and two antibiotics, except in two trials that included three antibiotics [18, 22]. One of the 14 RCTs [21] had a tailored triple therapy regimen, which selected either clarithromycin or metronidazole according to the antimicrobial susceptibility testing. In one of the 14 RCTs [24], the two antibiotics used in TT had two regimens. In seven of the 14 RCTs, the duration of triple therapy was 7 d. In the remaining studies, the duration of triple therapy was 5 d [22], 10 d [19, 24–27, 29], or 14 d [18, 20, 25, 28]. In two of the RCTs [18, 26], the comparison groups had two arms. The participants were randomly assigned to one of three groups: an intervention group that received ST, a 7-d TT group and a 10-d TT group, or a 7-d TT group and a 14-d TT group. The objective of the index review was to compare ST with TT; thus, the TT arms were combined into a single TT group. However, in the subgroup analysis based on the duration of TT, ST was compared with the two different TTs. Another RCT compared ST with three TTs, differing only in the duration of the TT group (7, 10, and 14 d) [25]. The three TTs arms were combined into a single TT group, but in the subgroup analysis based on the duration of TT, ST was compared with the three different TT groups. The ST consisted of a PPI (Omeprazole or lansoprazole) and amoxicillin administered for the first 5 d, followed by a PPI and two antibiotics administered for another 5 d. Details of the ST and TT are presented in Table 2.
Only three of the 10 RCTs published as full-text publications were judged to have a low risk of bias [16, 23, 27]. The trials published in abstract form had a number of methodological limitations or lacked adequate information to assess the overall risk of bias (Table 3). The funnel plot of the RR from the 14 RCTs showed clear asymmetry favoring ST, as evidenced by the absence of trials in the lower right-hand portion of the triangle (Fig. 2). The result of the Egger’s test (bias = −1.067905 [95 % CI: −2.804128 to 0.668318], P 0.205) provided no statistical evidence for publication bias. However, the sensitivity of the Egger’s test was generally low in meta-analyses based on <20 trials [30]; thus, caution is necessary in interpreting the result.
There were 1698 participants (718 for ST and 980 for TT) enrolled in the included studies (Fig. 3). The eradication rate was 73 % (524/718) for ST (95 % CI: 70–76) and 66 % (651/980) for TT (95 % CI: 64–70). The pooled RR from 14 RCTs using the fixed model was 1.16 (95 % CI: 1.09–1.23), yielding a NNT of 16 (95 % CI: 10–48) favoring ST. However, the I 2 showed a moderate degree of heterogeneity (30 %).
The pooled RRs from the trials published as full-text papers and abstracts using the fixed model were 1.19 (95 % CI: 1.11–1.27) and 1.00 (95 % CI: 0.89–1.13), respectively (Fig. 3). No evidence of heterogeneity was found in either comparison. Only the trials published as full-text publications found that ST had a statistically significant advantage.
The results of the trials based on the duration of TT are shown in Fig. 4. There was only a higher eradication rate when comparing the 7-d or 10-d STT (seven RCTs, n = 830, RR: 1.22, 95 % CI: 1.13–1.32 and six RCTs, n = 779, RR: 1.20, 95 % CI: 1.09–1.32). No such effect was found when compared to 14-d TT. No evidence of high heterogeneity was found in the three comparisons. Only one RCT analyzed a 5-d STT, and since it was underpowered, no firm conclusion could be drawn.
Data regarding therapy-related adverse effects were available from eight of the included trials [16, 19–21, 23, 25, 26, 28] (Fig. 5). No significant differences between the study groups with respect to the overall risk of adverse effects were found (Eight RCTs, n = 1131, RR: 1.05, 95 % CI: 0.85–1.30). No evidence of high heterogeneity was found. In addition, no significant differences between the study groups with respect to abdominal pain were found (Four RCTs, n = 388, RR: 1.23, 95 % CI: 0.74–2.03).
The need to discontinue the eradication treatment was reported in five trials [16, 20, 21, 23, 24] (Seven patients; one in the ST group [20] and six in the TT group [20, 21, 24]).
Compliance was assessed in six RCTs [16, 20–23, 29], and in all of these studies, compliance was claimed to be excellent, with no significant differences between the study groups.
Discussion
This meta-analysis shows that the ITT eradication rates of H. pylori were 73 % for ST and 66 % for TT in the pediatric population. However, ST did not obviously improve the eradication rates; the NNT for one additional child to be eradicated was 16. In addition, the absolute pooled eradication rate of ST did not reach the expected level (80 % in the intention-to-treat analysis and 90 % in the per-protocol analysis) [31], and the anti-microbial susceptibility may account for this. A recent review summarized the resistance rates for commonly used antimicrobial agents in different parts of the world and showed that clarithromycin-resistance is a major problem in most developed counties, with a few notable exceptions, such as in Scandinavia [32]. This has not been systematically assessed in the present review. However, only two RCTs [21, 29] provided related data on the eradication rate according to pre-treatment antimicrobial susceptibility testing. Since the response to eradication therapy is significantly related to the prevalence of primary resistance in the population, the choice of treatment regimen should be based on the knowledge of the underlying prevalence of resistant strains in the community, which need to be closely monitored.
Two previous meta-analyses [8, 9] have assessed the efficacy of ST compared to TT in children successively. However, the present meta-analysis further consolidates and adds to the evidence reported in previous meta-analyses conducted in children. First, the authors carefully analyzed the meta-analysis performed by Gatta et al. [8] who concluded that ST is superior to triple therapy for H. pylori eradication. However, this finding was only obvious in the adult population (10 RCTs, n = 3006, RR: 2.99, 95 % CI: 2.47–3.62). In the pediatric population, ST showed no statistically significant advantage in H. pylori eradication (Three RCTs, n = 260, RR: 1.98, 95 % CI: 0.96–4.07). The eradication of H. pylori observed in adults was obviously higher compared to that in children studied in the present review. Second, the other meta-analysis performed by Horvath et al. [9], which was later updated by their group [10] and excluded data from one RCT for ethical reasons, found a significant difference between the ST and TT group with respect to the H. pylori eradication rates in the pediatric population (9 RCTs, n = 813, RR: 1.11, 95 % CI: 1.03–1.20). Although the evidence was limited, the findings of the trials based on the duration of TT showed that ST was only superior to 7-d TT, which differs from the conclusion of the present analysis that ST is superior to 7- and 10-d TT. Neither the index analysis nor the two relevant aforementioned meta-analyses found significant differences in the rate of adverse effects between the ST and TT groups.
This meta-analysis has several potential limitations. First, determining the antimicrobial susceptibility is useful for choosing the best treatment option and/or for managing treatment failure, particularly with clarithromycin [1, 5]. However, only two RCTs [21, 29] provided the related data. Unfortunately, antimicrobial susceptibility testing is still not widely available in the United States and other countries; therefore, the availability of new kits that can perform susceptibility testing (e.g., by using real-time polymerase chain reaction in stool) will likely make matters easier in the future [32]. Second, there was no available RCT data from North America or other regions, which may limit the generalizability. Third, not all studies conformed to the diagnosis standard of H. pylori infection that was recommended and based on a positive histopathology plus a positive rapid urease test, or a positive culture [5]. Fourth, adherence to the treatment regimen is difficult to measure, and incomplete data are provided in the studies on compliance. Lastly, the strength of the present conclusions may be reduced by the varied methodological quality of the included RCTs.
Conclusions
This meta-analysis provides evidence that 10-d ST is superior to either 7- or 10-d TT. However, the improvement was only moderate, and the absolute pooled eradication rate of ST did not reach the expected level. Factors-associated with a higher risk of eradication failure, such as compliance and antimicrobial resistance, remain insufficiently investigated. Therefore, further high-quality RCTs are needed to compare these different eradication treatment approaches.
References
Seo JH, Woo HO, Youn HS, Rhee KH. Antibiotics resistance of Helicobacter pylori and treatment modalities in children with infection. Korean J Pediatr. 2014;57:67–71.
Pacifico L, Osborn JF, Tromba V, Romaggioli S, Bascetta S, Chiesa C. Helicobacter pylori infection and extragastric disorders in children: a critical update. World J Gastroenterol. 2014;20:1379–401.
Huang FC, Chang MH, Hsu HY, Lee PI, Shun CT. Long-term follow-up of duodenal ulcer in children before and after eradication of Helicobacter pylori. J Pediatr Gastroenterol Nutr. 1999;28:76–80.
Tam YH, Lee KH, To KF, Lee PI, Shun CT. Helicobacter pylori-positive versus Helicobacter pylori-negative idiopathic peptic ulcers in children with their long-term outcomes. J Pediatr Gastroenterol Nutr. 2009;48:299–305.
Koletzko S, Jones NL, Goodman KJ, et al; H pylori working groups of ESPGHAN and NASPGHAN. Evidence-based guidelines from ESPGHAN and NASPGHAN for Helicobacter pylori infection in children. J Pediatr Gastroenterol Nutr. 2011;53:230–43.
Oderda G, Shcherbakov P, Bontems P, et al; European Pediatric Task Force on Helicobacter pylori. Results from the Pediatric European Register for Treatment of Helicobacter pylori (PERTH). Helicobacter. 2007;12:150–6.
Zullo A, Rinaldi V, Winn S, et al. A new highly effective short-term therapy schedule for Helicobacter pylori eradication. Aliment Pharmacol Ther. 2000;14:715–8.
Gatta L, Vakil N, Leandro G, Di Mario F, Vaira D. Sequential therapy or triple therapy for Helicobacter pylori infection: systematic review and meta-analysis of randomized controlled trials in adults and children. Am J Gastroenterol. 2009;12:3069–79.
Horvath A, Dziechciarz P, Szajewska H. Meta-analysis: sequential therapy for Helicobacter pylori eradication in children. Aliment Pharmacol Ther. 2012;36:534–41.
Horvath A, Dziechciarz P, Szajewska H. Letter: sequential therapy for Helicobacter pylori eradication in children’ updated meta-analysis of randomized controlled trials. Aliment Pharmacol Ther. 2013;37:835–6.
Higgins JPT, Green S. Cochrane handbook for systematic reviews of interventions version 5.0.1 [updated March 2011]. The Cochrane Collaboration, 2011. Available at: http://www.cochrane-handbook.org.
Liberati A, Altman DG, Tetzlaff J, et al. The PRISMA statement for reporting systematic reviews and meta-analyses of studies that evaluate healthcare interventions: explanation and elaboration. BMJ. 2009;339:b2700.
Higgins JPT, Altman DG; On behalf of the Cochrane Statistical Methods Group and the Cochrane Bias Methods Group. Assessing risk of bias in included studies. In: Higgins JPT, Green S, editors. Cochrane Handbook for Systematic Reviews of Interventions. Chichester, UK: Wiley-Blackwell; 2008. p. 187–241.
Egger M, Davey Smith G, Schneider M, Minder C. Bias in meta-analysis detected by a simple, graphical test. BMJ. 1997;315:629–34.
Higgins JP, Thompson SG, Deeks JJ, Altman DG. Measuring inconsistency in meta-analyses. BMJ. 2003;327:557–60.
Francavilla R, Lionetti E, Castellaneta SP, et al. Improved efficacy of 10-day sequential treatment for Helicobacter pylori eradication in children: a randomized trial. Gastroenterology. 2005;129:1414–9.
Lerro P, Kuvidi M, Baldi M, Calvo PL, Barbera C. A 10-day sequential therapy: new option for Helicobacter pylori eradication in children. Dig Liver Dis. 2006;38:A104–5.
Hurduc V, Dragomir D, Leseanu G, et al. Comparison of sequential and triple therapies in the eradication of H. pylori infection in symptomatic children. Gut. 2007;56:A243.
Lu JH, Xu MY, Sheng Y, Yang WX. Comparison of the efficacy of 10-day sequential therapy and conventional triple therapy for Helicobacter pylori eradication in children. Zhongguo Dang Dai Er Ke Za Zhi. 2010;12:988–90.
Baysoy G, Saltik Temizel I, Uslu N, et al. Sequential therapy is not effective for the treatment of Helicobacter pylori infection in children. J Pediatr Gastroenterol Nutr. 2010;50:E131.
Bontems P, Kalach N, Oderda G, et al. Sequential therapy versus tailored triple therapies for Helicobacter pylori infection in children. J Pediatr Gastroenterol Nutr. 2011;53:646–50.
Anania C, Di Nardo G, Olivero G, Ferraro F, Olivero E, Pacifico L. Sequential versus concomitant therapy for Helicobacter pylori infection in children: a pilot study. J Pediatr Gastroenterol Nutr. 2011;52:E170–1.
Albrecht P, Kotowska M, Szajewska H. Sequential therapy compared with standard triple therapy for Helicobacter pylori eradication in children: a double-blind, randomized, controlled trial. J Pediatr. 2011;159:45–9.
Liu LF, Zhen LN, Zhao Y, et al. The efficacy of sequential therapy and standard triple therapy for eradication of Helicobacter pylori infection in children. J Clin Pediatr. 2011;29:925–8.
Huang J, Gong ST, Qu WJ, et al. A 10 day sequential therapy for eradication of Helicobacter pylori infection in children. Zhongghua Er Ke Za Zhi. 2012;50:563–7.
Huang J, Zhou L, Geng L, et al. Randomised controlled trial: sequential vs. standard triple therapy for Helicobacter pylori infection in Chinese children-a multicentre, open-labelled study. Aliment Pharmacol Ther. 2013;38:1230–5.
Laving A, Kamenwa R, Sayed S, Kimang’a AN, Revathi G. Effectiveness of sequential v. standard triple therapy for the treatment of Helicobacter pylori infection in children in Nairobi, Kenya. S Afr Med J. 2013;103:921–4.
Baysoy G, Saltik Temizel IN, Uslu N, et al. Ornidazole-based sequential therapy is not effective in Helicobacter pylori eradication in children. Turk J Gastroenterol. 2013;24:382–6.
Kutluk G, Tutar E, Bayrak A, et al. Sequential therapy versus standard triple therapy for Helicobacter pylori eradication in children: any advantage in clarithromycin-resistant strains? Eur J Gastroenterol Hepatol. 2014;26:1202–8.
Sterne JA, Egger M, Smith GD. Systematic reviews in health care: investigating and dealing with publication and other biases in meta-analysis. BMJ. 2001;323:101–5.
Graham DY, Lu H, Yamaoka Y. A report card to grade Helicobacter pylori therapy. Helicobacter. 2007;12:275–8.
Vakil N, Megraud F. Eradication treament for Helicobacter pylori. Gastroenterology. 2007;133:985–1001.
Conflict of Interest
None.
Source of Funding
None.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Huang, Y., Zhan, X. Sequential Therapy is Superior to Triple Therapy for Helicobacter pylori Infection in Children: A Meta-Analysis. Indian J Pediatr 83, 307–315 (2016). https://doi.org/10.1007/s12098-015-1878-0
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12098-015-1878-0