Abstract
Background
Breast cancer (BC) prevalence steadily increases in older patients but their treatment is based on the geriatric evaluations of comorbidities and potential benefits proved in clinical trials with younger patients. The lack of better decision-making tools urges to promote the search for new prognostic markers. The association between inflammation, aging and cancer may be crucial for better treatment selection. We sought to analyze its impact on the survival of older BC patients, evaluating the interaction with age and comorbidities.
Methods
We evaluated the relationship between inflammatory biomarkers at BC diagnosis (circulating blood cell counts and inflammatory indexes) and BC-related and not related mortality rate, evaluating the influence of comorbidities and age through the competitive risks assessment.
Results
We analyzed 148 consecutive BC patients aged ≥ 70 years old, diagnosed with BC and regional lymph node metastases. After the median follow-up of 51.5 months, 59 patients died (28 due to breast cancer progression and 31 because of other causes). Increased levels of circulating monocytes, neutrophils and neutrophil-to-lymphocytes ratio and decreased level of eosinophils and eosinophil multiple by neutrophils-to-lymphocytes ratio were associated with higher probability of BC-related death but not with death related to other causes.
Conclusion
Our data suggest a role of inflammatory parameters as a possible prognostic tool in therapeutic decision-making process in older patients with BC, as increased level of inflammation was associated with cancer-specific mortality. Prospective studies may give the possibility of refining the geriatric evaluation for BC treatment in elderly.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Although the incidence of Breast Cancer (BC) increases with age and the tumor biology is not the same in the elderly, clinical trials usually exclude older population and the clinical guidelines are based mainly on the data from younger patients [1, 2]. The prescribed cancer treatment in older patients depends not only on the tumor subtype but also on the life expectancy, conditioned by their frailty and comorbidities. However, there are still many patients who do not achieve expected effects of anti-cancer therapy, because they experience more toxicity and fewer benefits than reported in clinical trials [1, 3].
Recently, we have witnessed a change in the paradigm of prognostic factors in cancer research, as more and more studies provide results about the prognostic and predictive role of systemic inflammation for survival outcomes in several malignancies.
However, most of geriatric evaluations, such as the Charlson comorbidity index (CCI), are based on patients’ comorbidities and do not include the individual inflammatory status, currently studied as a prognostic factor for different types of cancer [4]. For these reasons, new prognostic tools to refine the evaluation of older patients while choosing the treatment are required.
Nevertheless, unlike in younger population, the evidence on the relationship between inflammation and cancer in elderly is still scarce. This is probably due to the potential bias caused by the association of low-grade chronic inflammation with the aging process, known as the inflamm-aging [5, 6]. For these reasons, here we propose the evaluation of a cohort of patients diagnosed with BC at the age of 70 years or above to analyze the difference in the impact of inflammatory indicators on the mortality rate, both related and unrelated to BC, and to clarify the interaction of systemic inflammation with BC biology, patients’ age and comorbidities. We hypothesized that blood cell counts and inflammatory indexes may be useful for the estimation of systemic inflammatory status and prognostic of survival in elderly patients with BC.
Patients and methods
After the approval of the Institutional Review Board, the medical records of all patients diagnosed with BC and regional lymph node metastases treated at our institution between January 2012 and January 2017 were retrospectively reviewed. The study was conducted in accordance with the ethical standards following the Declaration of Helsinki.
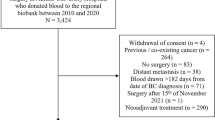
The clinical data of 148 consecutive patients diagnosed at the age of 70 years old or above with BC with regional lymph node metastases were analyzed. All patients had accessible blood test results done within 3 months prior to any treatment (surgery or neoadjuvant). Patients with chronic treatment with corticosteroids or immunosuppressive therapy were excluded (Fig. 1).
Inflammatory indicators
The absolute white blood cells (WBC) count was analyzed separately for circulating neutrophils (absolute neutrophils count—ANC), lymphocytes (ALC), monocytes (AMC) and eosinophils (AEC) in pre-treatment blood tests. Additionally, the following preoperative inflammatory indicators were examined: neutrophil-to-lymphocyte ratio (NLR: neutrophil count divided by the lymphocyte count), monocyte-to-lymphocyte ratio (MLR: monocyte count divided by the lymphocyte count), eosinophil-to-lymphocyte ratio (ELR: eosinophil count divided by the lymphocyte count) and Eosinophils*Neutrophil-to-Lymphocytes Ratio (ENLR: eosinophil count multiplied by neutrophils count and divided by the lymphocyte count). The most appropriate cut-off value for each indicator was chosen, according to the optimal decision threshold from the receiver operating characteristics (ROC) curve using the Youden index.
Statistics
The primary endpoint consisted of evaluation of the prognostic value of WBC absolute count and systemic inflammation biomarkers on the cumulative incidence of BC-related and non-BC-related deaths in the studied population of elderly patients with BC.
Descriptive statistics were summarized using mean, median, standard deviation (SD), and range. The comparisons between quantitative variables were estimated by t-paired or chi-squared tests.
All statistical analyses were performed using the statistical software R (www.r-project.com). Analysis items with p value < 0.05 were considered statistically significant. Survival outcomes were calculated from the date of diagnostic biopsy to the event occurrence, which was breast cancer-related death or death due to other cause.
The estimation of the prognostic value of the WBC and inflammatory indicators was based on the competitive risks methodology. For the analysis of competing risk of death, cumulative incidences (CI) for BC-related and non-BC-related deaths were calculated and compared using the modified chi-squared statistic [7]. Sub-distribution hazard ratio (SDHR) was calculated for quantifying predictive relationships between variables and CI [8].
Results
Patients’ characteristics and treatment
A total of 148 patients with a median age of 76 years (range 70–91 years) were included in the study. Almost 30% of patients were ≥ 80 years old and 42.6% had ≥ 2 comorbidities. The severity of comorbidities was high, since in 54% of patients the CCI was > 6.
An 85.8% of the patients had luminal BC subtype, distinction between luminal tumors (A or B) was not possible because Ki-67 index was available only in 17 patients. Triple-negative tumors (TTN) were the least frequent (6.8%). At diagnosis, 74.4% of the patients were clinically diagnosed with stage II or III of disease, while 25.6% presented stage Ib with N micro-metastases. Only 17 patients (11.5%) received some neoadjuvant treatment: 12 patients were treated with chemotherapy, 4 patients with endocrine therapy and 1 patient with radiotherapy. Among these, 4 patients (2.7%) did not finally receive surgical treatment. Characteristics of all patients are summarized in Table 1.
Systemic inflammation markers: cut-off value
The most appropriate cut-off value for each indicator was as follows: 2351.5 for ALC with an area under curve (AUC) of 0.46, specificity (Sp) of 0.49 and a sensitivity (Se) of 0.47; 641 for AMC (AUC 0.61, Sp 0.53, Se 0.58); 4489 for ANC (AUC 0.62, Sp 0.53, Se 0.59); 105 for AEC (AUC 0.58, Sp 0.48, Se 0.59); 10.5 for LMR (AUC 0.36, Sp 0.54, Se 0.38); 3.5 for NLR (AUC 0.60, Sp 0.76, Se 0.33); 0.035 for ELR (AUC 0.47, Sp 0.63, Se 0.35) and 65.5 for ELNR (AUC 0.64, Sp 0.49, Se 0.65).
Outcomes
Median follow-up (FU) for the entire cohort was 51.5 months (P25 39.3–P75 71). During this time, 59 patients (39.8%) died: in 28 patients (18.9%) the underlying cause of death was BC, 11 patients (7.4%) died from other cancer, 4 patients (2.7%) due to diseases associated with cardiovascular risk factors and 16 patients (10.8%) due to other diseases. At the end of the study, 89 patients (60.2%) remained alive.
All WBC and inflammatory markers were independent of age, tumor subtype and clinical stage. ANC and AEC were associated with the number of comorbidities (0–1 versus > 2) (p = 0.02 and p = 0.04, respectively), while ANC and NLR were associated with CCI (p = 0.00 and p = 0.01, respectively) (Table 2).
A greater risk of BC-related mortality was found in patients with higher circulating neutrophils (ANC ≥ 4489) and monocytes (AMC ≥ 641), and lower eosinophils (AEC < 105), as well as in patients with NLR ≥ 3.5 or with ENLR < 65.5, while no statistically significative differences were observed in patients with high level of circulating lymphocytes (ALC ≥ 2351.5), LMR ≥ 10.5 or ELR ≥ 0.035 (Fig. 2).
When SDHR was calculated and its effect on CI for BC was analyzed, univariate analysis has shown that AMC ≥ 641, ANC ≥ 4489, AEC < 105, NLR ≥ 3.5 and ELNR < 65.5 indicated a higher risk of BC compared to their respective counterparts (Table 3). Interestingly, the BC-related mortality was not associated with any of expected patients and tumor characteristics, such as patient’s age, number of comorbidities, CCI, cancer clinical stage and molecular subtype (Table 4).
However, in the multivariate analysis, neither WBC nor inflammatory markers demonstrated to be independent prognosticators for both BC-related and non-related mortality.
Discussion
Although BC is biologically different in elderly, the patients diagnosed at the age of 70 years old or above are under-represented in the clinical trials [1, 3, 9]. As a consequence, the clinical guidelines are based on the benefits proved in younger patients [10]. Moreover, the geriatric scales, such as the CCI, rely mainly on the evaluation of co-morbidities and do not include any immunological characteristics, which may determine patient’s response to the tumor and, as a consequence, their survival [11].
In many older women, the supposed benefit of the oncological treatments is based on the survival prediction, which fails due to the lack of better tools to assess the patients’ availability to receive highly toxic treatment and urges to promote the search for new predictive markers. Avoiding overtreatment and under-treatment should be a central objective in older patients treated for BC due to its direct impact on patient mortality [1, 2, 6].
Probably for this reason, many older patients are still frequently under- or over-treated, as the analysis of the risk–benefit ratio of anti-cancer therapy for this population does not address the individual capacity of the inflammatory response to the tumor development [12]. This situation is reflected both in geriatric scales and new decision-making algorithms for older BC patients, such as a new nomogram proposed to estimate the risk of death within 90 days after BC surgery in older patients, based on seven variables (age, gender, comorbidity score, facility type, facility location, clinical stage, and surgery type) [13].
Besides, this immunological response may be different in older patients, as aging is associated with a chronic inflammation and immune deregulation process known as inflamm-aging [5]. This process is based on sustained high levels of pro-inflammatory substances produced without the influence of specific triggers, where the ability for articulating an effective inflammatory response is also reduced [14, 15].
On the one hand, inflamm-aging has been proposed as a strong candidate to be the link between aging and cancer as chronic inflammatory status has influence in the microenvironment of several types of tumors, this include BC [16].
On the other hand, inflamm-aging is associated to cellular and tissue damage, and this contributes to the development of patients’ frailty [6, 14, 15]. Several studies have found a relationship between frailty and high leucocyte, neutrophil and monocyte counts [17, 18].
Many studies found the relation of inflammatory markers at cancer diagnosis and patient’s survival [19, 20]. Although BC has not classically been associated with an obvious chronic inflammatory process in the tumor microenvironment, available evidence shows that higher levels of pro-inflammatory markers slow down the process of the age-related atrophy of the mammary lobes and consequently may produce an increased risk of developing BC [21].
To date, the influence of WBC and inflammatory markers on the younger BC patients’ survival was described by many authors [22, 23]. However, the results in geriatric patients have scarcely been reported [12].
In our study, ANC ≥ 4489, AMC ≥ 641, AEC < 105, NLR ≥ 3.5 and ELNR < 65.5 were associated with an increased risk of BC-related death, but not with non-BC-related mortality. In geriatric patients, the presence of comorbidities and subsequent chronic inflammation may determine the higher levels of circulation WBC. Nevertheless, in our analysis, the altered WBC levels did not influence the non-BC mortality but conditioned the BC-related deaths, probably as a part of the antitumor response of the adaptive immune system [24].
Moreover, the increased number of circulating monocytes determines an increase in reactive oxygen species (ROS) production, thereby inducing a state of suppression of the antitumor activity of T lymphocytes and NK cells [25]. The role of monocytes in BC development was examined in the recently published article of Wang et al., who suggested that the proportion of BC progression depends on two essential components of the tumor microenvironment: monocytes and inflammatory cytokine CLCX7 [26].
Additionally, once in tumor tissue, monocytes can differentiate into tumor-associated macrophages and promote the tumor invasion and metastasis by preparing a favorable tumoral microenvironment [27].
Our results, that included all BC subtypes, are consistent with these findings, although up till now, many studies were focused only on the more aggressive molecular subtypes, such as TNT [28]. A meta-analysis that included more than 5500 patients reported that a low lymphocyte-to-monocyte ratio (LMR) was associated with a poor overall survival (OS), particularly in TNT, due to stronger immune response from NK cells than tumors expressing estrogen receptors and higher presence of regulatory T lymphocytes with immunosuppressive activity in tumor tissue of TNT [29]. Our results did not show the prognostic value of LMR, possibly due to high proportion of luminal tumors in our sample.
Regarding AEC, ELR and ENLR, none of these indices has been previously studied in older patients with BC. The difference that we observed between ELR and ENLR results suggests that the relationship between eosinophils and lymphocytes in ELR was affected by neutrophils in ELNR. Lower lever of AEC and ENLR was associated with higher BC-related mortality and this finding is attractive regarding the role of eosinophils in tumorigenesis, as some authors suggested that a greater amount of eosinophils infiltrated into the tumor led to a decrease in its peripheral blood count [30].
The prevalence of chronic diseases in our study is higher compared to that reported by other studies in BC [30]. Even so, our results are in agreement with the previously cited investigations as we confirmed the higher inflammation status associated with comorbidities: we found a significantly higher ANC, NLR and AEC values in patients with ≥ 2 comorbidities and CCI ≥ 6 (Table 2).
The aging process is related to the presence of comorbidities and sustained chronic inflammation, but we hypothesize that the tumor development may change this stable chronic inflammation. Our results suggested that hematological indices of chronic inflammation could be useful and easily available prognosis tool in older BC patients.
Strengths and weaknesses of our study
Our study aimed to differentiate the impact of age-related inflammation and tumor-related inflammation on the survival of BC diagnosed in older patients. The main strength of this work is the analysis of the influence of inflammatory markers separately on the BC-related and non-related mortality. According to our results, patients with altered immunological response were at higher risk of dying from BC, as the changes in immunological system during the tumor were different to the age-related inflammation. To our best knowledge, our approach is a pioneer to investigate how the immune response in the older patients increases the risk of tumor-related death, without losing sight of age-related immune changes.
Moreover, none of our patients was exposed to anti-inflammatory treatment (Fig. 2) and the cut-off values of inflammatory markers were established for population ≥ 70 years old. Of note, another recent study, which specifically addressed the role of WBC and inflammatory markers, was conducted in older BC population, only 52.2% of included patients were 65–70 years old and only one index (platelet-to-lymphocyte ratio, PLR) was associated with OS and disease-free survival (DFS) [12]. Besides, in this study, the cut-off values for each inflammatory marker were not based on geriatric population, in fact they were based on a previous study, addressing patients with a median age around 46 years old [22]. Additionally, patients treated with systemic steroids were not excluded [14].
However, the relatively short FU and limited number of patients in the current study could have influenced our multivariate analysis results. For these reasons, there is an urgent need to confirm our hypothesis in larger prospective studies that should be based on the evaluation of the immune system changes during cancer development and how to differentiate them from the physiological age-related inflammation, as a part of the next major advance in BC treatment.
Our research outlines the clinical importance of host-derived factors regulating the Systemic inflammatory response in BC patients and suggests the implementation of this information for developing new risk stratification criteria and follow-up recommendations. We believe that our study provides new evidence about the role of systemic inflammation in BC outcomes in elderly and may generate more questions about the mechanism of WBC interaction and its influence on tumor progression.
This is the first report that describes and analyses the pre-treatment inflammatory ratios as prognostic indicators in older BC patients, suggesting that they might provide additional prognostic value beyond the standard clinical–pathological parameters and should be a subject of more extensive studies to define better their clinical application.
Conclusion
The treatment of BC diagnosed in older patients is challenging, as the new guidelines dedicated to older population are mainly based on the results of trials extrapolated from younger patients. The inclusion of inflammatory index in the geriatric evolution would help to improve prediction of the life expectancy in patients with cancer and to better adjust the personalized treatment. Addressing the relationship between BC and chronic inflammation in older patients with BC could provide relevant data to guide therapeutic decisions and might be helpful for planning intervention strategies in this population.
References
Hurria A, Wong FL, Villaluna D, et al. Role of age and health in treatment recommendations for older adults with breast cancer: the perspective of oncologists and primary care providers. J Clin Oncol. 2008;26(33):5386–92. https://doi.org/10.1200/JCO.2008.17.6891.
Magnuson A, Sedrak MS, Gross CP, et al. Development and validation of a risk tool for predicting severe toxicity in older adults receiving chemotherapy for early-stage breast cancer. J Clin Oncol. 2021. https://doi.org/10.1200/JCO.20.02063.
Bastiaannet E, Portielje JE, van de Velde CJ, et al. Lack of survival gain for elderly women with breast cancer. Oncologist. 2011;16(4):415–23. https://doi.org/10.1634/theoncologist.2010-0234.
Truffi M, Piccotti F, Albasini S, Tibollo V, Morasso CF, Sottotetti F, Corsi F. Preoperative systemic inflammatory biomarkers are independent predictors of disease recurrence in ER+ HER2-early breast cancer. Front Oncol. 2021;11: 773078. https://doi.org/10.3389/fonc.2021.773078.
Franceschi C, Bonafè M, Valensin S, et al. Inflamm-aging. An evolutionary perspective on immunosenescence. Ann N Y Acad Sci. 2000;908:244–54. https://doi.org/10.1111/j.1749-6632.2000.tb06651.x.
Jenny NS. Inflammation in aging: cause, effect, or both? Discov Med. 2012;13(73):451–60.
Fine JP, Gray RJ. A proportional hazards model for the subdistribution of a competing risk. J Am Stat Assoc. 1999;94(446):496–509. https://doi.org/10.2307/2670170.
Noordzij M, Leffondré K, van Stralen KJ, Zoccali C, Dekker FW, Jager KJ. When do we need competing risks methods for survival analysis in nephrology? Nephrol Dial Transplant. 2013;28(11):2670–7. https://doi.org/10.1093/ndt/gft355.
Cappellani A, Di Vita M, Zanghì A, Cavallaro A, Piccolo G, Majorana M, Barbera G, Berretta M. Prognostic factors in elderly patients with breast cancer. BMC Surg. 2013;13(Suppl 2):S2. https://doi.org/10.1186/1471-2482-13-S2-S2.
Biganzoli L, Battisti NML, Wildiers H, et al. Updated recommendations regarding the management of older patients with breast cancer: a joint paper from the European Society of Breast Cancer Specialists (EUSOMA) and the International Society of Geriatric Oncology (SIOG). Lancet Oncol. 2021;22(7):e327–40. https://doi.org/10.1016/S1470-2045(20)30741-5.
August DA, Rea T, Sondak VK. Age-related differences in breast cancer treatment. Ann Surg Oncol. 1994;1(1):45–52. https://doi.org/10.1007/BF02303540.
Losada B, Guerra JA, Malón D, Jara C, Rodriguez L, Del Barco S. Pretreatment neutrophil/lymphocyte, platelet/lymphocyte, lymphocyte/monocyte, and neutrophil/monocyte ratios and outcome in elderly breast cancer patients. Clin Transl Oncol. 2019;21(7):855–63. https://doi.org/10.1007/s12094-018-1999-9.
Dillon J, Thomas SM, Rosenberger LH, DiLalla G, Fayanju OM, Menendez CS, Hwang ES, Plichta JK. Mortality in older patients with breast cancer undergoing breast surgery: how low is “Low Risk”? Ann Surg Oncol. 2021;28(10):5758–67. https://doi.org/10.1245/s10434-021-10502-3.
López-Otín C, Blasco MA, Partridge L, Serrano M, Kroemer G. The hallmarks of aging. Cell. 2013;153(6):1194–217. https://doi.org/10.1016/j.cell.2013.05.039.
Fulop T, McElhaney J, Pawelec G, et al. Frailty, inflammation and immunosenescence. Interdiscip Top Gerontol Geriatr. 2015;41:26–40. https://doi.org/10.1159/000381134.
Colotta F, Allavena P, Sica A, Garlanda C, Mantovani A. Cancer-related inflammation, the seventh hallmark of cancer: links to genetic instability. Carcinogenesis. 2009;30(7):1073–81. https://doi.org/10.1093/carcin/bgp127.
Leng SX, Xue QL, Tian J, et al. Associations of neutrophil and monocyte counts with frailty in community-dwelling disabled older women: results from the Women’s Health and Aging Studies I. Exp Gerontol. 2009;44(8):511–6. https://doi.org/10.1016/j.exger.2009.05.005.
Samson LD, Boots AMH, Verschuren WMM, et al. Frailty is associated with elevated CRP trajectories and higher numbers of neutrophils and monocytes. Exp Gerontol. 2019;125: 110674. https://doi.org/10.1016/j.exger.2019.110674.
Szor DJ, Dias AR, Pereira MA, Ramos MFKP, Zilberstein B, Cecconello I, Ribeiro-Júnior U. Prognostic role of neutrophil/lymphocyte ratio in resected gastric cancer: a systematic review and meta-analysis. Clinics (Sao Paulo). 2018;73: e360. https://doi.org/10.6061/clinics/2018/e360.
Shen J, Zhu Y, Wu W, Zhang L, Ju H, Fan Y, Zhu Y, Luo J, Liu P, Zhou N, Lu K, Zhang N, Li D, Liu L. Prognostic role of neutrophil-to-lymphocyte ratio in locally advanced rectal cancer treated with neoadjuvant chemoradiotherapy. Med Sci Monit. 2017;23:315–24. https://doi.org/10.12659/msm.902752.
Hanna M, Dumas I, Orain M, Jacob S, Têtu B, Sanschagrin F, Bureau A, Poirier B, Diorio C. Association between local inflammation and breast tissue age-related lobular involution among premenopausal and postmenopausal breast cancer patients. PLoS One. 2017;12(8): e0183579. https://doi.org/10.1371/journal.pone.0183579.
Marín Hernández C, Piñero Madrona A, Gil Vázquez PJ, Galindo Fernández PJ, Ruiz Merino G, Alonso Romero JL, Parrilla PP. Usefulness of lymphocyte-to-monocyte, neutrophil-to-monocyte and neutrophil-to-lymphocyte ratios as prognostic markers in breast cancer patients treated with neoadjuvant chemotherapy. Clin Transl Oncol. 2018;20(4):476–83. https://doi.org/10.1007/s12094-017-1732-0.
Graziano V, Grassadonia A, Iezzi L, Vici P, Pizzuti L, Barba M, Quinzii A, Camplese A, Di Marino P, Peri M, Veschi S, Alberti S, Gamucci T, Di Gioacchino M, De Tursi M, Natoli C, Tinari N. Combination of peripheral neutrophil-to-lymphocyte ratio and platelet-to-lymphocyte ratio is predictive of pathological complete response after neoadjuvant chemotherapy in breast cancer patients. Breast. 2019;44:33–8. https://doi.org/10.1016/j.breast.2018.12.014.
Mccoy JL, Rucker R, Petros JA. Cell-mediated immunity to tumor-associated antigens is a better predictor of survival in early stage breast cancer than stage, grade or lymph node status. Breast Cancer Res Treat. 2000;60(3):227–34. https://doi.org/10.1023/a:1006405504158.
Donskov F, Hokland M, Marcussen N, Torp Madsen HH, von der Maase H. Monocytes and neutrophils as “bad guys” for the outcome of interleukin-2 with and without histamine in metastatic renal cell carcinoma-results from a randomised phase II trial. Br J Cancer. 2006;94(2):218–26. https://doi.org/10.1038/sj.bjc.6602937.
Wang YH, Shen CY, Lin SC, Kuo WH, Kuo YT, Hsu YL, Wang WC, Lin KT, Wang LH. Monocytes secrete CXCL7 to promote breast cancer progression. Cell Death Dis. 2021;12(12):1090. https://doi.org/10.1038/s41419-021-04231-4.
Qian BZ, Pollard JW. Macrophage diversity enhances tumor progression and metastasis. Cell. 2010;141(1):39–51. https://doi.org/10.1016/j.cell.2010.03.014.
Fabbri F, Salvi S, Bravaccinni S. Know your enemy: Genetics, aging, exposomic and inflammation in the war against triple negative breast cancer. Semin Cancer Biol. 2020;2(60):285–93. https://doi.org/10.1016/j.semcancer.2019.10.015.
Carretero R, Sektioglu IM, Garbi N, Salgado OC, Beckhove P, Hämmerling GJ. Eosinophils orchestrate cancer rejection by normalizing tumor vessels and enhancing infiltration of CD8(+) T cells. Nat Immunol. 2015;16(6):609–17. https://doi.org/10.1038/ni.3159.
Louwman WJ, Janssen-Heijnen ML, Houterman S, Voogd AC, van der Sangen MJ, Nieuwenhuijzen GA, Coebergh JW. Less extensive treatment and inferior prognosis for breast cancer patient with comorbidity: a population-based study. Eur J Cancer. 2005;41(5):779–85. https://doi.org/10.1016/j.ejca.2004.12.025.
Acknowledgements
The authors thank Mr Manuel Rain Montecinos for his generous and dedicated contribution to the statistical analysis. The authors wish also to sincerely thank Miss Joselyn Maturana, Dra. Paula Escobar, Dr. Pedro Galaz, Dr Jorge Gamboa, Dr Rodrigo Iglesis, Dr Joaquín Irarrázabal, Dr Miguel Maturana, Dr Aliro Neira and Dra Karina Peña, without their valuable support this study could not have been accomplished.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Ethical standards
The manuscript does not contain clinical studies or patients’ data.
Informed consent
For this type of study, formal consent is not required.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Vargas, A., Holub, K. & Biete, A. Systemic inflammation in older patients with breast cancer: the missing point in geriatric evaluations to sharpen survival prediction. Clin Transl Oncol 24, 1800–1808 (2022). https://doi.org/10.1007/s12094-022-02836-5
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12094-022-02836-5