Abstract
Background
Anti-cancer effect of metformin on different kinds of lung cancer has been studied frequently. However, the association between metformin and the prognosis of lung cancer in type 2 diabetes patients is still controversial.
Methods
An electronic search was conducted using PubMed/Medicine, EMBASE and Cochrane library databases. Statistical analyses were carried out using either random-effects or fixed-effects models according to the heterogeneity examined by I 2 statistics.
Results
Six studies involving 2350 patients were included in the current meta-analysis. In all, the pooled HR of overall survival (OS) was 0.90 (95 % CI 0.84–0.96; P = 0.003). Sub-group analysis showed that when stratified by region the HR of OS was 0.52 (95 % CI 0.31–0.87; P = 0.012) and 0.86 (95 % CI 0.67–1.11, P = 0.361) for Asian and Western countries. When stratified by study design, the HR of OS was 0.78 (95 % CI 0.52–1.15, P = 0.206) and 0.82 (95 % CI 0.59–1.16, P = 0.264) for cohort and medical data-based studies. When stratified by lung cancer subtype, HR of OS was 0.52 (95 % CI 0.31–0.87; P = 0.012), 1.06 (95 % CI 0.51–2.19; P = 0.878) and 0.82 (95 % CI 0.59–1.16; P = 0.264) for SCLS, NSCLC and non-divided subtypes, respectively.
Conclusion
Metformin use may associate with a good prognosis in lung cancer patients with type 2 diabetes but the effect was modest. However, it could achieve benefits in a selective sub-group of lung cancer patients especially in SCLC patients from Asian. Further studies are warranted to confirm this efficacy.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Cancer and diabetes are increasingly prevalent all over the world. Growing evidence has suggested that patients with diabetes often have clinical risk factors for the development of cancer. An epidemiologic link between type 2 diabetes mellitus (T2D) and an increased incidence of breast cancer, colorectal cancer, gastrointestinal malignancies, pancreatic cancer, renal cancer, bladder cancer, and thyroid cancer, as well as a worse long-term outcome for cancer survival, has been reported [1–4].
Primary lung cancer is the leading cause of cancer-related mortality among males in both more and less developed countries, and has overtaken breast cancer as the leading cause of cancer death among females in more developed countries [5]. Further, although treatments for lung cancer have rapidly developed in recent years, the overall prognosis of these patients still remains poor.
Metformin, a diabetes drug with well-established side effect and safety profiles, is commonly prescribed as first-line treatment for type 2 diabetes. Generally, this drug improves blood glucose control and insulin sensitivity by decreasing hepatic glucose production and intestinal glucose absorption and increasing peripheral glucose uptake. Further, it has been widely studied for its anti-tumor activities in a number of cancers, including lung cancer. Although the underlying molecular mechanisms are not well understood [6, 7], it can be produced by both direct (insulin-independent) and indirect (insulin-dependent) ways [8].
Metformin use and the cancer risk have been studied popularly. Mazzone et al. [9, 10] found that the use of metformin is associated with a lower likelihood of developing lung cancer in diabetic patients, which was concordant with the study by Lai et al. [10]. By contrast, the study by Bodmer et al. [11] reached the opposite result. Another observational study by Smiechowski et al. [7] demonstrated that metformin use was not associated with a decreased risk of lung cancer in patients with T2D.
Also, the anti-cancer effect of metformin on different kinds of lung cancer has been studied frequently. Xu et al. reported that prognosis of small cell lung cancer (SCLC) patients with diabetes treated with metformin was improved [12]. Lin et al. conclude that metformin is associated with improved survival among patients with diabetes with stage IV non-small cell lung cancer (NSCLC) [13]. However, Mazzone et al. found that the diabetics who develop lung cancer while receiving metformin may have a more aggressive disease and worse prognosis [9].
Based on these findings, the association between metformin and the prognosis of lung cancer in T2D patients is still controversial and it is necessary to conduct a meta-analysis to further confirm the effect. So the current meta-analysis was performed to investigate the association between metformin use and lung cancer prognosis of individuals with T2D.
Materials and methods
Literature search to identify related studies
A comprehensive literature search was performed for all the studies addressing the association between metformin use and lung cancer prognosis. Electronic databases searched included PubMed/MEDLINE and EMBASE until June 2015, without language restrictions. We also carried out independent searches using the Cochrane library databases to ensure that no studies were overlooked. The Mesh terms and/or the text words used included ‘metformin’ or ‘biguanides’ and lung ‘cancer’ or ‘neoplasms’. In addition, the list of articles was supplemented through extensive crosschecking of the reference lists of all retrieved articles. Unpublished data and conference proceedings were not included.
Selection criteria
Two reviewers (R. H. Tian and Y. G. Zhang) independently assessed the eligibility of each article. After screening all titles and reading the abstracts, the full text of the selected articles was reviewed to determine their eligibility for inclusion in the study and any discrepancy between the reviewers was resolved by consensus. The inclusion criteria of the meta-analysis are as following: (1) randomized controlled trials, data-based or cohort studies; (2) designed to evaluate the association between metformin and the prognosis of lung cancer in type 2 diabetic patients; and (3) contained sufficient information to allow adequate estimation of hazard ratio (HR), odds ratio (OR), or relative risk (RR) and 95 % confidence interval (95 % CI) of overall survival (OS), disease-free survival (DFS) or progress-free survival (PFS) to estimate the prognosis of lung cancer patients with T2D using metformin compared to other anti-diabetic treatments or no treatment.
Data extraction
Data extraction was conducted independently by two investigators (RH Tian and JW Yang). For each enrolled study, collected data included the following: (1) basic information of each eligible study such as author names, year of publication and country or area; (2) characteristics of patients such as median or mean age, gender composition, tumor type; (3) information of study designation such as number of enrolled subjects, group sample size, and follow-up time; (4) results of treatment such as OS, median DFS or PFS and adjusted HRs with their 95 % CIs. To resolve disagreements between reviewers, a third reviewer (Z. Wu) assessed all discrepant items and the majority opinion was used to choose studies for analysis.
Quality assessment
To ascertain the validity of the eligible studies, the quality of each study was evaluated in reference to the Newcastle–Ottawa statement by two investigators (R. H. Tian and H. l. Ji) [14]. In this ‘star system’ scale, studies were judged on three aspects: selection, comparability and exposure. For the selection and exposure categories, a maximum of one star was awarded for each numbered item, whereas for the comparability, a maximum of two stars was awarded. Therefore, the quality of each study, with nine stars at most, was classified as follows: ≤5 stars as low quality and ≥6 stars as high quality. Also, to resolve disagreements between reviewers, a third reviewer (X. Liu) assessed all discrepant items and the majority opinion was used to award the stars.
Statistical analyses
Pooled HRs with 95 % CI were analyzed. Heterogeneity analysis was performed by calculating the I 2 index, which was interpreted as low (25 %), moderate (50 %) and high heterogeneity (75 %) [15]. For the meta-analysis, both fixed-effects (weighted with inverse variance) and random-effects models were considered. A random-effects model was chosen when heterogeneity was >50 %, while a fixed-effects model was chosen when heterogeneity was <50 % [16]. Publication bias was assessed using a standard funnel plot, and funnel plot asymmetry was further tested using Begg’s and Egger’s regression methods [17]. Forest plots were sorted according to first author’s name, year of publication and country to illustrate the HR with 95 % CI. All statistical analyses were performed using Stata Version 12.0 software (Stata Corporation, College Station, TX).
Results
Study characteristics and quality assessment
The current meta-analysis was carried out in accordance with the guidelines of PRISMA [18]. The literature search identified 186 potentially relevant articles. 61 papers were excluded because of duplicates. After screening titles and abstracts, 77 irrelevant articles were excluded because they involved animal/in vitro studies, letters or commentaries and other cancer types. After reading the full text of the remaining 48 studies, 42 were excluded because review articles or case reports, other treatment agents, assessing risk of cancer and no sufficient data. Finally, six studies [9, 12, 13, 19–21] involving 2350 patients matched our inclusion criteria and included in the current meta-analysis. The process of study selection is shown in a flow chart (Fig. 1).
The baseline characteristics of each study are shown in Table 1. These six papers were all retrospective studies with 4 cohort studies and 2 data-based studies. Most of them were published very recently in 2015 from China and USA. All subtypes of lung cancer including SCLC as well as NSCLC with I to IV stage were involved. The median age of enrolled patients ranged from 56.2 to 72.5.
The quality of the six included studies was appraised in reference to the Newcastle–Ottawa statement and the stars number ranged from 6–8, which indicated a high quality of all the eligible studies (Table 2).
Publication bias
Several strategies were used in the study design to minimize the potential for publication bias. These were the extension of search strategy, strict inclusion criteria and the careful design of the analytic method. Publication bias was not found according to the funnel plot (Begg’s test, P = 0.436; Egger test, P = 0.311) (Fig. 2).
Pooled effect of metformin on survival outcomes of lung cancer
Four of the eligible studies reported the median OS in the metformin and non-metformin use group patients. The median OS in the metformin use groups ranged from 5–20 months while non-metformin use groups ranged from 3–19.2 months. All studies reported the HR value of OS when compared the overall survival of metformin and non-metformin use groups. The HR value ranged from 0.504–1.73 indicating that the prognosis value of metformin use in lung cancer patients with T2D was not confirmed. The result of meta-analysis demonstrated that the pooled HR was 0.90 (95 % CI 0.84–0.96; I 2 = 88.1 %; P = 0.003) (Fig. 3). The combined HR showed that metformin use may associate with a good prognosis in lung cancer patients with T2D but the effect was modest.
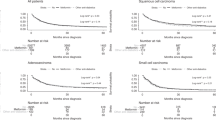
Furthermore, the studies were stratified to evaluate HR of OS by region (Asian or Western), study design (cohort or data-based study) and lung cancer subtypes (SCLC, NSCLC, or non-divided subtypes). To analyze study region on evaluating HR, the studies from Asia countries showed a statistically significant HR of 0.52 (95 % CI 0.31–0.87; I 2 = 0.0 %; P = 0.012), however, the studies from Western countries almost had no statistical significance (HR = 0.86, 95 % CI 0.67–1.11; I 2 = 89.9 %; P = 0.361). In analyzing study design on evaluating HR, both cohort and data-based design studies had no significance (HR = 0.78, 95 % CI 0.52–1.15, I 2 = 52.5 %; P = 0.216 and HR = 0.82, 95 % CI 0.59–1.16, I 2 = 91.4 %; P = 0.264, respectively) (Fig. 4). A sub-group analysis was also performed for studies concerned with different subtypes of lung cancer (Fig. 5). The meta-analysis demonstrated that the HR of OS was 0.52 (95 % CI 0.31–0.87; I 2 = 0.0 %; P = 0.012), 1.06 (95 % CI 0.51–2.19; I 2 = 71.6 %; P = 0.878) and 0.82 (95 % CI 0.59–1.16; I 2 = 91.4 %; P = 0.264) for SCLS, NSCLC and non-divided subtypes, respectively (Table 3).
Discussion
Our meta-analysis assessed the effects of metformin use on overall survival of lung cancer patients with type 2 diabetes mellitus. As per the literature to date, this is the first meta-analysis that has evaluated the association between metformin use and disease progression among these patients. We found four retrospective cohort studies and two data-based studies (utilized the real-world electronic medical records or cancer registry or administrative claims databases) for conducting this meta-analysis. We found that metformin marginally improved the overall survival of lung cancer patients with type 2 diabetes mellitus. The pooled HR was 0.90 (95 % CI 0.84–0.96; P = 0.003) which indicated that metformin use may associate with a good prognosis in lung cancer patients with T2D but the effect was modest. In sub-group analysis, metformin use significantly associated with a good prognosis in patients with SCLC, patients from Asian (cancer patients taking metformin have longer survival compared to those not taking metformin). However, as showed in Western, NSCLC and all subtypes of lung cancer sub-groups analysis, metformin use was not associated with a good prognosis in these patients.
The relation between diabetes and cancer risk has been well documented [3]. The increased cancer risk in diabetes has been explained by obesity, insulin resistance, and/or increased levels of IGF-I and insulin [22]; and hyperglycemia also may play a role in enhancing tumor growth or resistance to anti-tumor therapy [23].
As a well-accepted anti-diabetes drug, the anti-cancer effect of metformin has also been studied all over the world. It could be benefit for performing better therapeutic strategies and improve the prognosis of cancer patients with T2D by elucidating the mechanisms that are involved in the anti-cancer effect of metformin. However, to date, the exact molecular mechanism of the anti-cancer role of metformin has not been fully unveiled. The potential mechanisms include the following: (1) The most widely accepted mechanism of metformin action is, by indirect activation of the central energy sensor, adenosine monophosphate-activated protein kinase (AMPK), which also plays a key role in insulin signaling [24, 25]. Metformin can also directly inhibit tumor cell growth/proliferation via modulation of cyclin D1-medicated cell cycle and the expression of tumor suppressor p53 in different tumor cells including pancreatic cancer and breast cancer [26]; (2) Enhance the tumor chemotherapy/radiotherapy sensitivity by the regulation of tumor micro-environment [27]; (3) Recently, one study reported that the underlying anti-cancer effect of metformin may be immunemediated [28]; (4) Metformin may also selectively inhibit the CSC phenotypes and functions, which may be responsible for inhibition of tumor development and progression. Moreover, emerging evidence suggests that metformin may play important roles in the modulation of tumor-associated or CSC-associated miRNAs that are critically important in the development and progression of a variety of tumors [29].
Several limitations had to be considered in the current meta-analysis. First, Asian patients are also the SCLC patients in the group analysis. Therefore, it cannot be known if the benefit observed by metformin use in these patients is related to the histology or the race of the patients. Second, the reason that patients were not receiving metformin was not clearly known. Most of the non-metformin patients will be requiring insulin because have worse controlled type 2 diabetes. The use of insulin could be a worse prognostic factor for itself (they have worse controlled diabetes). Also, insulin receptor (IR) and insulin-like growth factor receptor (IGF-1R) have been described as worse prognostic factors in lung cancer patients [30, 31], and these receptors could be stimulated by insulin administration, whilst metformin could decrease the circulating levels of insulin, having an indirect effect [8]. Third, although, most of the eligible studies included in this current study were adjusted for potential confounders, thus minimizing potential bias, heterogeneity across studies is still relatively high. The high heterogeneity could come from variety bias. In most study, the information on cancer treatment was not described clearly, which could affect the survival of cancer patients and thus biased the effect estimate of metformin on survival. Lack of metformin dose could be another major source of heterogeneity. In addition, different kinds of cancer stages, pathological types, size and metastasis may also explain the high heterogeneity. Fourth, the current meta-analysis was not based on individual patient data, which could be the cause of an overestimate of the treatment effects. Finally, we performed sub-group analysis according to region, cancer subtype and study design, but the limited data would potentially limit the evaluation of the therapeutic effects.
In conclusion, our meta-analysis demonstrated that adjuvant therapy of metformin, an anti-diabetes drug with well-established side effect and safety profiles, may associate with a good prognosis in lung cancer patients with T2D but the effect was modest. However, the sub-group analysis showed that metformin use may significantly improve the overall survival in SCLC patients and lung cancer patients in Asian. These findings suggest that metformin use could achieve benefits in a selective sub-group of lung cancer patients with diabetics. Further studies are warranted to confirm this efficacy especially blind randomized controlled clinical trial.
References
Richardson LC, Pollack LA. Therapy insight: influence of type 2 diabetes on the development, treatment and outcomes of cancer. Nat Clin Pract Oncol. 2005;2:48–53. doi:10.1038/ncponc0062.
Noto H, Tsujimoto T, Sasazuki T, Noda M. Significantly increased risk of cancer in patients with diabetes mellitus: a systematic review and meta-analysis. Endocr Pract. 2011;17:616–28. doi:10.4158/ep10357.ra.
Gallagher EJ, LeRoith D. Obesity and diabetes: the increased risk of cancer and cancer-related mortality. Physiol Rev. 2015;95:727–48. doi:10.1152/physrev.00030.2014.
Wu L, Wang Z, Zhu J, Murad AL, Prokop LJ, Murad MH. Nut consumption and risk of cancer and type 2 diabetes: a systematic review and meta-analysis. Nutr Rev. 2015;73:409–25. doi:10.1093/nutrit/nuv006.
Torre LA, Bray F, Siegel RL, Ferlay J, Lortet-Tieulent J, Jemal A. Global cancer statistics, 2012. CA Cancer J Clin. 2015;65:87–108. doi:10.3322/caac.21262.
Aljada A, Mousa SA. Metformin and neoplasia: implications and indications. Pharmacol Ther. 2012;133:108–15. doi:10.1016/j.pharmthera.2011.09.004.
Smiechowski BB, Azoulay L, Yin H, Pollak MN, Suissa S. The use of metformin and the incidence of lung cancer in patients with type 2 diabetes. Diabetes Care. 2013;36:124–9. doi:10.2337/dc12-0740.
Del Barco S, Vazquez-Martin A, Cufi S, Oliveras-Ferraros C, Bosch-Barrera J, Joven J, et al. Metformin: multi-faceted protection against cancer. Oncotarget. 2011;2:896–917.
Mazzone PJ, Rai H, Beukemann M, Xu M, Jain A, Sasidhar M. The effect of metformin and thiazolidinedione use on lung cancer in diabetics. BMC Cancer. 2012;12:410. doi:10.1186/1471-2407-12-410.
Lai SW, Liao KF, Chen PC, Tsai PY, Hsieh DP, Chen CC. Antidiabetes drugs correlate with decreased risk of lung cancer: a population-based observation in Taiwan. Clin Lung Cancer. 2012;13:143–8. doi:10.1016/j.cllc.2011.10.002.
Bodmer M, Becker C, Jick SS, Meier CR. Metformin does not alter the risk of lung cancer: a case-control analysis. Lung Cancer. 2012;78:133–7. doi:10.1016/j.lungcan.2012.08.010.
Xu T, Liang G, Yang L, Zhang F. Prognosis of small cell lung cancer patients with diabetes treated with metformin. Clin Transl Oncol. 2015;. doi:10.1007/s12094-015-1311-1.
Lin JJ, Gallagher EJ, Sigel K, Mhango G, Galsky MD, Smith CB, et al. Survival of patients with stage IV lung cancer with diabetes treated with metformin. Am J Respir Crit Care Med. 2015;191:448–54. doi:10.1164/rccm.201407-1395OC.
Wells GA, Shea B, O’Connel D, Peterson J, Welch V, Losos M, et al. The Newcastle–Ottawa Scale (NOS) for assessing the quality of nonrandomised studies in meta-analyses. http://www.ohri.ca/programs/clinical_epidemiology/oxford.asp.
Higgins JP, Thompson SG, Deeks JJ, Altman DG. Measuring inconsistency in meta-analyses. BMJ. 2003;327:557–60. doi:10.1136/bmj.327.7414.557.
DerSimonian R, Laird N. Meta-analysis in clinical trials. Control Clin Trials. 1986;7:177–88.
Copas J, Shi JQ. Meta-analysis, funnel plots and sensitivity analysis. Biostatistics. 2000;1:247–62. doi:10.1093/biostatistics/1.3.247.
Moher D, Liberati A, Tetzlaff J, Altman DG. Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. J Clin Epidemiol. 2009;62:1006–12. doi:10.1016/j.jclinepi.2009.06.005.
Kong F, Gao F, Liu H, Chen L, Zheng R, Yu J, et al. Metformin use improves the survival of diabetic combined small-cell lung cancer patients. Tumour Biol. 2015;. doi:10.1007/s13277-015-3549-1.
Ahmed I, Ferro A, Cohler A, Langenfeld J, Surakanti SG, Aisner J, et al. Impact of metformin use on survival in locally-advanced, inoperable non-small cell lung cancer treated with definitive chemoradiation. J Thorac Dis. 2015;7:346–55. doi:10.3978/j.issn.2072-1439.2014.12.32.
Xu H, Aldrich MC, Chen Q, Liu H, Peterson NB, Dai Q, et al. Validating drug repurposing signals using electronic health records: a case study of metformin associated with reduced cancer mortality. J Am Med Inform Assoc. 2015;22:179–91. doi:10.1136/amiajnl-2014-002649.
Johnson JA, Gale EA. Diabetes, insulin use, and cancer risk: are observational studies part of the solution-or part of the problem? Diabetes. 2010;59:1129–31. doi:10.2337/db10-0334.
Yang X, Ko GT, So WY, Ma RC, Yu LW, Kong AP, et al. Associations of hyperglycemia and insulin usage with the risk of cancer in type 2 diabetes: the Hong Kong diabetes registry. Diabetes. 2010;59:1254–60. doi:10.2337/db09-1371.
El-Mir MY, Nogueira V, Fontaine E, Averet N, Rigoulet M, Leverve X. Dimethylbiguanide inhibits cell respiration via an indirect effect targeted on the respiratory chain complex I. J Biol Chem. 2000;275:223–8.
Owen MR, Doran E, Halestrap AP. Evidence that metformin exerts its anti-diabetic effects through inhibition of complex 1 of the mitochondrial respiratory chain. Biochem J. 2000;348(Pt 3):607–14.
Bao B, Wang Z, Li Y, Kong D, Ali S, Banerjee S, et al. The complexities of obesity and diabetes with the development and progression of pancreatic cancer. Biochim Biophys Acta. 2011;1815:135–46. doi:10.1016/j.bbcan.2010.11.003.
Zannella VE, Dal Pra A, Muaddi H, McKee TD, Stapleton S, Sykes J, et al. Reprogramming metabolism with metformin improves tumor oxygenation and radiotherapy response. Clin Cancer Res. 2013;19:6741–50. doi:10.1158/1078-0432.ccr-13-1787.
Eikawa S, Nishida M, Mizukami S, Yamazaki C, Nakayama E, Udono H. Immune-mediated antitumor effect by type 2 diabetes drug, metformin. Proc Natl Acad Sci USA. 2015;112:1809–14. doi:10.1073/pnas.1417636112.
Bao B, Azmi AS, Ali S, Zaiem F, Sarkar FH. Metformin may function as anti-cancer agent via targeting cancer stem cells: the potential biological significance of tumor-associated miRNAs in breast and pancreatic cancers. Ann Transl Med. 2014;2:59. doi:10.3978/j.issn.2305-5839.2014.06.05.
Kim JS, Kim ES, Liu D, Lee JJ, Behrens C, Lippman SM, et al. Activation of insulin-like growth factor 1 receptor in patients with non-small cell lung cancer. Oncotarget. 2015;6:16746–56.
Kim JS, Kim ES, Liu D, Lee JJ, Solis L, Behrens C, et al. Prognostic impact of insulin receptor expression on survival of patients with nonsmall cell lung cancer. Cancer. 2012;118:2454–65. doi:10.1002/cncr.26492.
Author information
Authors and Affiliations
Corresponding authors
Ethics declarations
Conflict of interest
None to declare.
Note
The manuscript does not contain clinical studies or patient data.
Rights and permissions
About this article
Cite this article
Tian, RH., Zhang, YG., Wu, Z. et al. Effects of metformin on survival outcomes of lung cancer patients with type 2 diabetes mellitus: a meta-analysis. Clin Transl Oncol 18, 641–649 (2016). https://doi.org/10.1007/s12094-015-1412-x
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12094-015-1412-x