Abstract
Introduction
The esophageal squamous cell carcinoma (ESCC) is the predominant pathological type and accounts for more than 80 % of esophageal cancer in China. The successful use of anti-epidermal growth factor receptor (EGFR) treatment in head and neck squamous cell carcinoma provides the rationale for introducing anti-EGFR targeting treatment in ESCC. One of our prospective phase II clinical trials analyzed the efficacy of nimotuzumab, an anti-EGFR agent, combined with chemotherapy (paclitaxel and cisplatin) to treat unresectable ESCC.
Materials and methods
We analyzed the correlation of the clinical response with EGFR expression by immunohistochemical staining (IHC).
Results
Totally 55 tumor samples were analyzed. 18/55 (32.7 %) cases were with high EGFR expression while the other 37/55 (67.3 %) cases were with low to moderate EGFR expression. The expression of EGFR was not related to gender, age, tumor location, tumor differentiation and clinical stage of disease. The objective response rate (ORR) in high EGFR expression group was 55.6 % (10/18) while that in low to moderate EGFR expression group was 54.1 % (20/37) (P = 0.57). Both the progression-free survival (PFS) and overall survival (OS) in high EGFR expression group were much shorter than those in low to moderate EGFR expression group (PFS: 5.8 ± 0.5 vs. 11.0 ± 2.8 months, P = 0.007; OS: 9.7 ± 0.5 vs. 21.5 ± 1.5 months, P = 0.03).
Conclusions
The results showed that over-expression of EGFR was related to poor survival of ESCC. The over-expression of EGFR by IHC might not be an ideal predictive biomarker of nimotuzumab treatment. Other EGFR pathway-associated molecules should be analyzed in further studies.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Esophageal cancer is composed of tumors of three distinct anatomic areas and two distinct histological subtypes: squamous cell carcinoma and adenocarcinoma. Though the adenocarcinoma is common in western countries, the majority of esophageal cancer in Asia, especially in China, is squamous cell carcinoma which accounts for more than 80 % of the disease [1].
Previous research had revealed that the epidermal growth factor receptor (EGFR) is over-expressed in esophageal cancer. Both the protein over-expression and gene amplification of EGFR had been reported to be associated with poor prognosis in esophageal squamous cell carcinoma (ESCC) [2]. In preclinical studies, cetuximab could decrease EGFR pathway signaling via reduced phosphorylation of EGFR and AKT in esophageal and gastric cancer cell lines [3]. Combination of chemotherapy and cetuximab resulted in synergistic inhibition of cell proliferation and enhanced apoptosis [4]. A Meta study including nine studies and 802 patients showed that over-expression of EGFR was significantly correlated with the lymph node status, tumor differentiation grade, and poor overall survival (OS) with a pooled HR of 1.60 [5].
The success of anti-EGFR targeting treatment in non-small cell lung cancer, colorectal cancer, and head and neck cancer encouraged pilot studies of introducing anti-EGFR target agents in treatment of esophageal cancer. The phase III EXTREME study demonstrated that combination of cetuximab and platinum/5-fluorouracil significantly improved OS in squamous cell carcinoma of the head and neck compared with chemotherapy alone [6]. Therefore, it provides the rationale for introducing anti-EGFR targeting treatment in ESCC. A number of phase 1 and 2 studies had explored the toxicities and safety of anti-EGFR agents such as cetuximab, panitumumab, and gefitinib in esophageal cancer. A randomized phase 2 study by Richards et al. analyzed the combination treatment of cetuximab and docetaxel plus oxaliplatin to treat advanced gastroesophageal cancer patients. The objective response rate (ORR) was 36.0 % and the progression-free survival (PFS) and OS were 4.3 and 8.5 months, respectively [7]. Then, they compared cetuximab with chemotherapy (docetaxel plus oxaliplatin) vs. chemotherapy alone in advanced adenocarcinoma of the gastroesophageal junction and stomach cancer in 150 patients. Though there were no statistical significant improvement, their results showed that the combination of cetuximab and chemotherapy was tolerable and with prolonged median PFS (5.1 vs. 4.7 months), and prolonged OS (9.4 vs. 8.5 months) [8]. However, a phase 2/3 multicenter randomized trial, SCOPE 1, reported that an addition of cetuximab to chemoradiotherapy (CRT) had more frequent toxicities, but no survival benefits (OS 22.1 vs. 25.4 months, P = 0.035) [9]. The REAL3 study compared chemotherapy (epirubicin, oxaliplatin, and capecitabine) with or without another anti-EGFR agent panitumumab and found that the combination was associated with worse OS (8.8 vs. 11.3 months; P = 0.01) [10]. Thus, more studies should be done to explore the clinical impacts of anti-EGFR treatment in esophageal cancer and potential biomarker to select patients who could benefit from such treatment.
In China, a humanized anti-EGFR monoclonal antibody, nimotuzumab, had been studied in several clinical trials. Nimotuzumab alone or combined with chemotherapy or radiotherapy was well tolerated. Liang et al. analyzed the efficacy of a combination treatment of nimotuzumab with radiotherapy in local advanced esophageal cancer. This phase II study enrolled 52 patients and the 3-year OS rate was 26.2 %. Nimotuzumab-related skin rash was observed in only four patients (7.7 %), but did not require treatment. Other radiotherapy associated Grade 3 toxicities including esophagitis and gastrointestinal, dermatological and hematological toxicities were observed in 21.4 % patients [11]. In another phase I study, 19 patients with local advanced esophageal cancer received chemotherapy (Cisplatin and 5-FU) and nimotuzumab. The ORR was 42.1 % and disease control rate was 68.4 %. The combination was well tolerated and the main adverse events were chemotherapy-associated leucopenia, vomiting, and asthenia [12].
In this study, we analyzed the expression of EGFR in tumor tissue of patients with ESCC by immunohistochemical staining (IHC) and its relationship with a combination treatment of nimotuzumab and chemotherapy in a prospective phase II study.
Materials and methods
Patients and treatment
Patients enrolled in this study were from a prospective phase II clinical trial of “Nimotuzumab plus paclitaxel and cisplatin as 1st line treatment for esophageal squamous cell cancer: a single center prospective clinical trial” (NCT01336049) conducted by the Peking University Cancer Hospital. The ethic committee of the Peking University Cancer Hospital had approved this trial and the written informed consent was signed voluntarily by the subjects before enrollment.
Patients must have histological confirmed esophageal squamous cell carcinoma with unresectable local advanced or metastatic tumor. Measurable disease according to the RECIST 1.0 criteria was required. Prior palliative chemotherapy and radiotherapy were excluded except for the non-target lesion radiation and adjuvant chemotherapy with an interval of at least 6 months. The age of patients should range from 18 to 75 and both genders were eligible. Patients should have no history of paclitaxel (except for adjuvant treatment) and the total dose of cisplatin should be less than 300 mg/m2 in previous treatments. Patients should have normal marrow, renal, and liver function, performance status of a Karnofsky score ≥80, and a life expectancy of ≥3 months.
Patients were given cisplatin 30 mg/m2 on day 1 and day 2, paclitaxel 175 mg/m2 on day 1, cycled every 21 days for at least 2 cycles. Nimotuzumab was given 200 mg weekly. CT scan was conducted before treatment, every two cycles after treatment, and every 6 months during the follow-up (The ultrasonic check of abdomen instead of CT scan was allowed during follow-up if there were not metastatic tumors in abdomen).
Immunohistochemical analysis
The tissues of tumor were collected by gastroscopic biopsy or surgical removed mass. The immunohistochemical staining procedure was performed according to the standard staining protocol. The tumor tissue was incubated overnight at 4 °C in a moist chamber with rabbit monoclonal antibody anti-EGFR (Zhongshan Jinqiao Biotechnology Co. Ltd., China; 1:100 dilution). A negative control was obtained by replacing the primary antibody with a normal goat serum. Known EGFR-expressing slides provided by Zhongshan Jinqiao Biotechnology Co. Ltd., China were used as positive controls.
Statistical analysis
This trial is a single arm study. All patients were classified into two arms according to their EGFR status of tumor tissues. Tumors in surgical removed samples or gastroscopic biopsy samples were considered to be low EGFR expression when there was no staining or membrane staining of EGFR in <10 % tumor cells was observed. Moderate complete and/or incomplete membrane staining in >10 %, but <50 % tumor cells was considered as moderate EGFR expression cases, while strong complete and/or incomplete membrane staining in >50 % tumor cells was considered as high EGFR expression cases.
Response to the treatment was evaluated by the investigators according to the Response Evaluation Criteria in Solid Tumors (RECIST) version 1.0. The Chi-square test and fisher’s exact test (in case of sample size less than 5) were used to evaluate difference between groups in all tests performed, with the resultant P value representing a two-sided test of statistical significance. Kaplan–Meier survival curves for different strata were plotted for OS and PFS. The differences were tested by the log-rank test. All statistical tests were performed with SPSS 17.0 software (SPSS, Inc., Chicago, IL) and a P value of <0.05 was considered statistically significant.
Results
Clinical characteristics
The clinical and pathological characteristics of patients with ESCC are summarized in Table 1. Totally 55 patients with unresectable local advanced or metastatic tumor were enrolled. There were 45 men and 10 women. The median age was 60.7 years old (range 42–76 years). In accordance with the World Health Organization criteria, one case (1.8 %) was well-differentiated tumor, 24 (43.6 %) were moderately differentiated tumor, and 29 (52.7 %) were poorly differentiated tumor. 35 of 55 tumors (63.6 %) were of the lower thoracic esophagus, 14 of 55 (25.5 %) were of the middle thoracic esophagus, and the other 6 (10.9 %) were of the upper thoracic or cervical esophagus. 31 of 55 (56.4 %) patients were with local advanced disease while the other 24 (43.6 %) patients were with metastatic disease.
Expression of EGFR in tumors
In all the 55 patients, 18 (32.7 %) cases were of low EGFR expression. 19 (34.5 %) cases were of moderate EGFR expression. 18 (32.7 %) cases were of high EGFR expression. The EGFR expression had no statistical correlation with younger age (under 60), gender, performance status scale, location of primary tumor, differentiation of tumor cell, and clinical stage (Table 1).
Correlation of EGFR expression with nimotuzumab treatment
54 patients received at least two cycles of the combination treatment of nimotuzumab and paclitaxel plus cisplatin chemotherapy. Only one patient quitted after one cycle of treatment due to progression of disease. The average was 3.3 cycles (range 1–6 cycles). No complete response was observed. 30/55 (54.5 %) cases were of partial response. 23/55 (41.8 %) cases were of stable diseases. The other 2/55 (3.63 %) cases were of progression disease. The ORR rate was 55.6 % (10/18) in high EGFR expression group compared with that of 54.1 % (20/37) in low to moderate EGFR expression group. There was no statistical difference between two groups (P = 0.57) (Table 2).
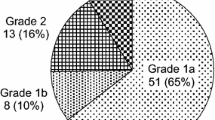
Patients were followed every 6 months and the last follow-up date was July 2014. The median follow-up time was 24 months. The PFS was only 5.8 ± 0.5 months (95 % CI 4.9–6.7 months) in high EGFR expression group while that in low to moderate EGFR expression group was 11.0 ± 2.8 months (95 % CI 5.5–16.6 months). There was significant difference (P = 0.007). Furthermore, the 1-year survival rate in low to moderate EGFR expression group was 74.8 % while that in high EGFR expression group was only 44.4 %. The median OS in high EGFR expression group was 9.7 ± 0.5 months (95 % CI 8.7–10.7 months) and much shorter than that of 21.5 ± 1.5 months (95 % CI 18.6–24.5 months) in low to moderate EGFR expression group (P = 0.03). It implied that the EGFR high expression was associated with poor prognosis of ESCC (Fig. 1).
The survival of ESCC patients treated with a combination of nimotuzumab and paclitaxel plus cisplatin in different EGFR status arms. The median PFS was poor in high EGFR expression group compared that in low or moderate EGFR expression group (5.8 ± 0.5 vs. 11.0 ± 2.8 months, P = 0.007). The median OS was also shorter in high EGFR expression group than that in low or moderate EGFR expression group (9.7 ± 0.5 vs. 21.5 ± 1.5 months, P = 0.03)
Adverse events
All patients tolerated the combination treatment well and there were no serious adverse events. Different from cetuximab, there was no grade 3 or 4 acneiform rash. The most common grade 3 and 4 adverse events were leukopenia 21.8 % (12/55), anorexia 9.1 % (5/55), vomiting 7.3 % (4/55), neuropathy 5.5 % (3/55), arthralgia 1.8 % (1/55), and fatigue 1.8 % (1/55). The dose of paclitaxel reduced in 17 patients while dose of cisplatin reduced in 2 patients due to grade 3 or 4 toxicities (Table 3).
Discussion
The successful use of anti-EGFR targeting treatment in colorectal cancer, non-small cell lung cancer, and head and neck squamous cell cancer had promoted a number of pilot studies of introducing this treatment in esophageal cancer. Most phase 1 and phase 2 studies of small cases suggested that such treatment alone or combining with standard chemotherapy or radiotherapy was well tolerated with limited toxicities in esophageal cancer [7, 8]. However, results of two following multicenter randomized clinical trials, SCOPE1 and REAL3, showed that an addition of anti-EGFR agents cetuximab or panitumumab to standard treatments failed to bring survival benefits, but with serious toxicities [9, 10].
Several things should be taken into consideration. First, the incidence of esophageal adenocarcinoma is much higher in western countries. In SCOPE1 study, more than 25 % patients (25 % in control arm and 26 % in cetuximab arm) were with esophageal adenocarcinoma while 545/553 (99 %) patients were adenocarcinoma in REAL3 study [9, 10]. Therefore, findings of these clinical trials should be reviewed in ESCC.
Second, the combination of cetuximab with CRT in SCOPE1 study or panitumumab with chemotherapy in REAL3 study had higher 3–4 grade non-hematological toxicities. It was reported that there were 22 % dermatological toxicities (rash, hand–foot syndrome, acne, etc.) and 24 % metabolic/laboratory abnormal in CRT plus cetuximab arm in SCOPE1 study. However, in our study, there were no grade 3–4 dermatological toxicities and metabolic abnormal. The most common grade 3–4 adverse events were leukopenia 21.8 % (12/55), anorexia 9.1 % (5/55), vomiting 7.3 % (4/55) and neuropathy 5.5 % (3/55), which were similar to those reported in SCOPE1 study. It is might be the different anti-EGFR agents nimotuzumab used in our study. Nimotuzumab has a tenfold lower affinity to the EGF receptor compared with cetuximab. It required bivalent binding for stable attachment to the cellular surface. These characteristics of nimotuzumab made it to selectively bind tumor cells with moderate to high EGFR expression levels. Clinical studies had demonstrated that nimotuzumab was very well tolerated and the most frequent adverse reactions were grade 1–2 infusion reactions and skin rashes [13, 14]. It alone or combining with radiotherapy or chemotherapy all showed anti-tumor activities, but limited toxicities in cancers such as glioma [15], oral cancer [16], pancreatic cancer [17, 18] and also esophageal cancer [11, 12, 19].
Different from colorectal cancer and lung cancer, there is not certain biomarkers reported to associated with the efficacy of anti-EGFR treatment in esophageal cancer. Clinical data confirmed that the efficacy of cetuximab and panitumumab was confined to patients with wild-type KRAS and BRAF in colorectal cancer [20]. However, in esophageal cancer, the mutation of KRAS and BRAF was rare [21, 22]. Bettstetter et al. analyzed the RAS and RAF mutation in 117 resected esophageal adenocarcinoma samples. The KRAS mutations were detected in 3 % tumors and no NRAS or BRAF mutations were detected [21]. Shigaki et al. reported that the KRAS mutation was only 0.5 % (1 of 203) and RAF was absent (0 of 203) in esophageal squamous cell carcinoma [22]. Due to the rare mutation rates, the status of KRAS and BRAF might not be of great value to predict clinical outcome of anti-EGFR treatment in esophageal cancer.
The mutation of EGFR in the tyrosine kinase domain had been confirmed as a predictor of good response to tyrosine kinase inhibitors (TKI) treatment in non-small cell lung cancer [23]. However, mutations in the EGFR kinase domain were also rare in esophageal cancers. Puhringer-Oppermann et al. reported that only 1 of 105 samples of esophageal cancer with silent mutation in exon 19 of EGFR [24]. Sunpaweravong et al. reported that no mutation in the tyrosine kinase domain of EGFR was detected in 48 ESCC patients though EGFR protein was over-expressed in 46 % patients [25]. Maeng et al. analyzed 87 ESCC tissue specimens using OncoMap 4.0 (a mass-spectrometry-based assay) and found only 1 EGFR mutation [26]. Furthermore, clinical trials showed that TKI inhibitor erlotinib had tolerable toxicities, but limited response in both squamous cell and adenocarcinoma of esophagus [27, 28]. Thus, the EGFR mutation was no likely to be an effective predictor of anti-EGFR treatment.
The over-expression of EGFR in esophageal cancer had been reported in 30–80 % of tumors, and correlated with worse prognosis [25, 29]. In our study, 19 (34.5 %) cases were of moderate EGFR expression and 18 (32.7 %) cases were of high EGFR expression. High EGFR expression group had poor PFS (5.8 ± 0.5 vs. 11.0 ± 2.8 months, P = 0.007) and OS (9.7 ± 0.5 vs. 21.5 ± 1.5 months, P = 0.03) compared with low to moderate EGFR group. These results were similar to those published data. Ramos-Suzarte reported that nimotuzumab with radiotherapy resulted in an objective response rate of 47.8 % and over-expression of EGFR was associated with good clinical response [30]. But other studies showed that the EGFR expression did not correlate to survival and clinical responses. In a phase II study, combination of cetuximab and CRT was used to treat 29 ESCC patients. But the PFS in EGFR-expressing tumor and EGFR-negative tumor had no difference (P = 0.133) [31]. In another study, Liang et al. analyzed the EGFR expression status in tumors of patients with ESCC who were given nimotuzumab and radiotherapy. The results showed the 2-year OS rate was prolonged in EGFR (+++) group, but without statistic difference (P = 0.4) [11]. In our study, the ORR rate was 55.6 % (10/18) and 54.1 % (20/37) in high EGFR expression and low to moderate EGFR expression groups, respectively, with no statistical difference (P = 0.57). Both the PFS and OS in high EGFR expression group were shorter than those in low to moderate EGFR expression group. It implied that the expression of EGFR might not be an ideal biomarker of nimotuzumab treatment.
Some investigations had analyzed other biomarkers in esophageal cancer and their relation with anti-EGFR treatment. Maeng et al. detected 20 hotspot mutations in 80 tumors of ESCC patients. They found that the most frequent mutation was PIK3CA mutation in 11.5 % tissue samples [26]. Lee et al. analyzed the EGFR polymorphism of CA repeat length at the 5′-regulatory sequence in intron 1 in 148 esophageal cancer patients. Their results showed that the homozygous short allele (<20 CA) of the EGFR gene had a shorter survival time than those with the homozygous long allele (HR of death: 1.88) [32]. Further studies should be done to explore the correlation of such biomarkers with the efficacy of anti-EGFR treatment in ESCC.
In conclusion, the over-expression of EGFR was associated with poor survival of ESCC patients who received combination treatment of nimotuzumab and paclitaxel plus cisplatin. The over-expression of EGFR by IHC was more like a prognostic biomarker of disease than a predictive biomarker of nimotuzumab treatment. Other EGFR pathway-associated molecules should be analyzed in future studies.
References
Liu SZ, Wang B, Zhang F, Chen Q, Yu L, Cheng LP, et al. Incidence, survival and prevalence of esophageal and gastric cancer in Linzhou city from 2003 to 2009. Asian Pac J Cancer Prev. 2013;14:6031–4.
Gibault L, Metges JP, Conan-Charlet V, Lozac’h P, Robaszkiewicz M, Bessaguet C, et al. Diffuse EGFR staining is associated with reduced overall survival in locally advanced oesophageal squamous cell cancer. Br J Cancer. 2005;93:107–15.
Dragovich T, Campen C. Anti-EGFR-targeted therapy for esophageal and gastric cancers: an evolving concept. J Oncol. 2009;2009:804108.
Luo HY, Wei W, Shi YX, Chen XQ, Li YH, Wang F, et al. Cetuximab enhances the effect of oxaliplatin on hypoxic gastric cancer cell lines. Oncol Rep. 2010;23:1735–45.
Yu WW, Guo YM, Zhu M, Cai XW, Zhu ZF, Zhao WX, et al. Clinicopathological and prognostic significance of EGFR over-expression in esophageal squamous cell carcinoma: a meta-analysis. Hepatogastroenterology. 2011;58:426–31.
Vermorken JB, Mesia R, Rivera F, Remenar E, Kawecki A, Rottey S, et al. Platinum-based chemotherapy plus cetuximab in head and neck cancer. N Engl J Med. 2008;359:1116–27.
Richards D, McCollum D, Wilfong L, Sborov M, Boehm KA, Zhan F, et al. Phase II trial of docetaxel and oxaliplatin in patients with advanced gastric cancer and/or adenocarcinoma of the gastroesophageal junction. Ann Oncol. 2008;19:104–8.
Richards D, Kocs DM, Spira AI, David McCollum A, Diab S, Hecker LI, et al. Results of docetaxel plus oxaliplatin (DOCOX) ± cetuximab in patients with metastatic gastric and/or gastroesophageal junction adenocarcinoma: results of a randomised Phase 2 study. Eur J Cancer. 2013;49:2823–31.
Crosby T, Hurt CN, Falk S, Gollins S, Mukherjee S, Staffurth J, et al. Chemoradiotherapy with or without cetuximab in patients with oesophageal cancer (SCOPE1): a multicentre, phase 2/3 randomised trial. Lancet Oncol. 2013;14:627–37.
Waddell T, Chau I, Cunningham D, Gonzalez D, Okines AF, Okines C, et al. Epirubicin, oxaliplatin, and capecitabine with or without panitumumab for patients with previously untreated advanced oesophagogastric cancer (REAL3): a randomised, open-label phase 3 trial. Lancet Oncol. 2013;14:481–9.
Liang J, E M, Wu G, Zhao L, Li X, Xiu X, et al. Nimotuzumab combined with radiotherapy for esophageal cancer: preliminary study of a Phase II clinical trial. Onco Targets Ther. 2013;6:1589–96.
Ling Y, Chen J, Tao M, Chu X, Zhang X. A pilot study of nimotuzumab combined with cisplatin and 5-FU in patients with advanced esophageal squamous cell carcinoma. J Thorac Dis. 2012;4:58–62.
Talavera A, Friemann R, Gomez-Puerta S, Martinez-Fleites C, Garrido G, Rabasa A, et al. Nimotuzumab, an antitumor antibody that targets the epidermal growth factor receptor, blocks ligand binding while permitting the active receptor conformation. Cancer Res. 2009;69:5851–9.
Boland WK, Bebb G. Nimotuzumab: a novel anti-EGFR monoclonal antibody that retains anti-EGFR activity while minimizing skin toxicity. Expert Opin Biol Ther. 2009;9:1199–206.
Solomon MT, Selva JC, Figueredo J, Vaquer J, Toledo C, Quintanal N, et al. Radiotherapy plus nimotuzumab or placebo in the treatment of high grade glioma patients: results from a randomized, double blind trial. BMC Cancer. 2013;13:299.
Meng J, Gu QP, Meng QF, Zhang J, Li ZP, Si YM, et al. Efficacy of nimotuzumab combined with docetaxel–cisplatin–fluorouracil regimen in treatment of advanced oral carcinoma. Cell Biochem Biophys. 2014;68:181–4.
Su D, Jiao SC, Wang LJ, Shi WW, Long YY, Li J, et al. Efficacy of nimotuzumab plus gemcitabine usage as first-line treatment in patients with advanced pancreatic cancer. Tumour Biol. 2014;35:2313–8.
Strumberg D, Schultheis B, Scheulen ME, Hilger RA, Krauss J, Marschner N, et al. Phase II study of nimotuzumab, a humanized monoclonal anti-epidermal growth factor receptor (EGFR) antibody, in patients with locally advanced or metastatic pancreatic cancer. Invest New Drugs. 2012;30:1138–43.
Ma NY, Cai XW, Fu XL, Li Y, Zhou XY, Wu XH, et al. Safety and efficacy of nimotuzumab in combination with radiotherapy for patients with squamous cell carcinoma of the esophagus. Int J Clin Oncol. 2014;19:297–302.
Jimeno A, Messersmith WA, Hirsch FR, Franklin WA, Eckhardt SG. KRAS mutations and susceptibility to cetuximab and panitumumab in colorectal cancer. Cancer J. 2009;15:110–3.
Bettstetter M, Berezowska S, Keller G, Walch A, Feuchtinger A, Slotta-Huspenina J, et al. Epidermal growth factor receptor, phosphatidylinositol-3-kinase catalytic subunit/PTEN, and KRAS/NRAS/BRAF in primary resected esophageal adenocarcinomas: loss of PTEN is associated with worse clinical outcome. Hum Pathol. 2013;44:829–36.
Shigaki H, Baba Y, Watanabe M, Miyake K, Murata A, Iwagami S, et al. KRAS and BRAF mutations in 203 esophageal squamous cell carcinomas: pyrosequencing technology and literature review. Ann Surg Oncol. 2013;20(Suppl 3):S485–91.
Yang CH. EGFR tyrosine kinase inhibitors for the treatment of NSCLC in East Asia: present and future. Lung Cancer. 2008;60(Suppl 2):S23–30.
Puhringer-Oppermann FA, Stein HJ, Sarbia M. Lack of EGFR gene mutations in exons 19 and 21 in esophageal (Barrett’s) adenocarcinomas. Dis Esophagus. 2007;20:9–11.
Sunpaweravong P, Suwiwat S, Sunpaweravong S, Puttawibul P, Mitarnun W. Correlation of epidermal growth factor receptor mutation, immunohistochemistry, and fluorescence in situ hybridization in esophageal squamous cell carcinoma. J Med Assoc Thai. 2009;92:1136–42.
Maeng CH, Lee J, van Hummelen P, Park SH, Palescandolo E, Jang J, et al. High-throughput genotyping in metastatic esophageal squamous cell carcinoma identifies phosphoinositide-3-kinase and BRAF mutations. PLoS ONE. 2012;7:e41655.
Javle M, Pande A, Iyer R, Yang G, LeVea C, Wilding G, et al. Pilot study of gefitinib, oxaliplatin, and radiotherapy for esophageal adenocarcinoma: tissue effect predicts clinical response. Am J Clin Oncol. 2008;31:329–34.
Ilson DH, Kelsen D, Shah M, Schwartz G, Levine DA, Boyd J, et al. A phase 2 trial of erlotinib in patients with previously treated squamous cell and adenocarcinoma of the esophagus. Cancer. 2011;117:1409–14.
Wang Q, Zhu H, Xiao Z, Zhang W, Liu X, Zhang X, et al. Expression of epidermal growth factor receptor is an independent prognostic factor for esophageal squamous cell carcinoma. World J Surg Oncol. 2013;11:278.
Ramos-Suzarte M, Lorenzo-Luaces P, Lazo NG, Perez ML, Soriano JL, Gonzalez CE, et al. Treatment of malignant, non-resectable, epithelial origin esophageal tumours with the humanized anti-epidermal growth factor antibody nimotuzumab combined with radiation therapy and chemotherapy. Cancer Biol Ther. 2012;13:600–5.
Chen Y, Wu X, Bu S, He C, Wang W, Liu J, et al. Promising outcomes of definitive chemoradiation and cetuximab for patients with esophageal squamous cell carcinoma. Cancer Sci. 2012;103:1979–84.
Lee JM, Yang SY, Yang PW, Shun CT, Wu MT, Hsu CH, et al. Polymorphism in epidermal growth factor receptor intron 1 predicts prognosis of patients with esophageal cancer after chemoradiation and surgery. Ann Surg Oncol. 2011;18:2066–73.
Acknowledgments
We thank all the staff at the Gastrointestinal Department, Peking University Cancer Hospital, for their help in patient’s administration, data collection, and follow-up.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
All authors declare that there is no conflict of interest.
Ethical statement
The ethic committee of the Peking University Cancer Hospital had approved this trial in March, 2011. This clinical trial had been registered on ClinicalTrials.gov (NCT01336049).
Informed consent
The written informed consent was signed voluntarily by the subjects before enrollment.
Rights and permissions
About this article
Cite this article
Jia, J., Cui, Y., Lu, M. et al. The relation of EGFR expression by immunohistochemical staining and clinical response of combination treatment of nimotuzumab and chemotherapy in esophageal squamous cell carcinoma. Clin Transl Oncol 18, 592–598 (2016). https://doi.org/10.1007/s12094-015-1406-8
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12094-015-1406-8