Abstract
Purpose
To investigate biological impact of the downregulation of yes-associated protein (YAP) through RNA interference in the process of epithelial–mesenchymal transition in MHCC97H and MHCC97L.
Methods
MHCC97H and MHCC97L cells were transiently transfected by YAP-siRNA. Furthermore, protein expressions and mRNA levels of characteristic markers of epithelial–mesenchymal transition (E-cadherin, N-cadherin) were examined by Western blotting and real-time polymerase chain reaction, and transwell invasion assay was used to detect changes of invasiveness of MHCC97H and MHCC97L cells.
Results
The transfected group with YAP-siRNA in MHCC97H after 72 h by Western blotting showed obviously higher expression of E-cadherin compared with the control group (P < 0.05), and lower expression of N-cadherin (P < 0.05). In MHCC97L cells, the expression of E-cadherin was also significantly increased (P < 0.05); however, N-cadherin expression did not significantly change (P > 0.05). Moreover, compared with the control group, Transwell invasion assay showed that the number of the transfected groups was significantly decreased in MHCC97H and MHCC97L cell lines (both P < 0.05). The result of real-time polymerase chain reaction indicated that mRNA levels of E-cadherin increased (P < 0.05), but the mRNA levels of N-cadherin did not significantly change (P > 0.05) in these two cell lines, indicating some effects of post-transcriptional regulation mechanism after silencing YAP.
Conclusions
YAP expression in human hepatocellular carcinoma cell lines MHCC97H and MHCC97L is closely related with the characteristic markers of epithelial–mesenchymal transition, N-cadherin and E-cadherin expression.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Hepatocellular carcinoma (HCC) is the sixth most prevalent cancer and third leading cause of cancer-related mortality worldwide [1]. Due to high incidence of tumor recurrence, frequent intrahepatic spread, and extrahepatic metastasis during the initial diagnosis, the recurrence rate in 5 years in patients who have undergone tumor resection remains approximately 70 % [2]. The overall survival time after liver resection remains the major obstacle to achieve long survival [3]. Thus, improved understanding of the molecular mechanism of HCC recurrence is essential for the development of new therapeutic strategies. The ability of epithelial cells to undergo mesenchymal transitions during embryogenesis, wound healing, and malignant progression is now widely accepted as a core biological process [4]. It has recently become clear that epithelial–mesenchymal transition (EMT) plays a great role not only in cancer cell proliferation, invasion, and metastasis, but also in tumor recurrence. During this process, the expression of epithelial marker E-cadherin is down-regulated, and the expression of mesenchymal markers, fibronection, vimentin, and N-cadherin, is up-regulated [5].
The Hippo signaling pathway originally discovered in Drosophila consisting of several negative growth regulators acting in a kinase cascade that ultimately phosphorylates and inactivates Yorkie (Yki), a transcriptional coactivator that positively regulates cell growth, survival, and proliferation [6]. Core components of the Hippo pathway include the Mst1/2, Lats1/2, and YAP, which consists of a kinase cascade in which Mst1/2 forms a complex with the adaptor protein WW45 and phosphorylates the kinases Lats1 and Lats2 as well as the adaptor protein Mob. A Lats/Mob complex then phosphorylates and represses the transcriptional coactivator YAP, YAP is phosphorylated and inhibited by the Lats tumor suppressor, and this phosphorylation results in its association with 14-3-3 binding motif and from the nucleus into the cytoplasm. Overexpression of YAP in the Hippo pathway during cancer development and progression are now clear [7]. YAP, which was termed a candidate oncogene, is a key component of the Hippo signaling pathway and plays a critical role in the development and progression of multiple cancer types, including HCC [8]. YAP1 has been reported to be potently prometastatic in breast cancer and melanoma cells [9]. However, the association of YAP involving in EMT of HCC had not been thoroughly investigated. In the present study, we explored the knockdown of yes-associated protein (YAP) through RNA interference in the process of epithelial–mesenchymal transition in MHCC97H and MHCC97L cells.
Materials and methods
Cell culture
The HCC cell lines MHCC97H and MHCC97L (HCC cell lines with high and low migratory potential, respectively) used in this study were obtained from the Shanghai Institute of Cell Biology (Shanghai, China) and were maintained in DMEM containing 10 % fetal bovine serum (Gibco, Grand Island, NY, USA) at 37° C with 5 % CO2.
RNA extraction, reverse transcription, and quantitative real-time polymerase chain reaction (qRT-PCR)
Total RNA from tissues and cells was extracted using Trizol reagent (Invitrogen, Carlsbad, CA). For detection of YAP, E-cadherin, and N-cadherin, total RNA was transcribed into cDNA using The Transcriptor First Strand cDNA Synthesis Kit (Roche Applied Scienceis) designed to reverse transcribe RNA. Primers used are as follows: GAPDH-F, 5′-CGGAGTCAACGGATTTGGTCGTAT-3′, GAPHH-R, 5-AGCCTTCTCCATGGTGGTGAAGAC-3′; YAP-F, 5′-CTGATGCAGGCACTGCAGGAG-3′, YAP-R, 5′-ACTGGTGGGGGCTGTGACG-3′; E-cadherin-F, 5′-GACCGAGAGAGTTTCCCTACG-3′; E-cadherin-R, 5′-TCAGGCACCTGACCCTTGTA-3′; N-cadherin-F, 5′-GAGATCCTACTGGACGGTTCG-3′; N-cadherin-R, 5′-TCTTGGCGAATGATCTTAGGA-3′. Studying gene expression levels, via two-step RT-PCR, using qualitative RT-PCR on the LightCycler® Carousel-Based System, the LightCycler® 480 System, the PCR reaction was evaluated using melting curve analysis. Glyceraldehyde 3-phosphate dehydrogenase (GAPDH) was amplified to ensure cDNA integrity, and to normalize expression, SYBR Green/ROX qPCR Master Mix Amplification of the generated cDNA was performed using SYBR Premix EX Taq II (Roche Applied Scienceis). All of the above experiments were performed according to the manufacturer’s instructions. All of the reactions were run in triplicate, and data were analyzed according to the comparative Ct (2−ΔΔCt) method.
Cell transfection
YAP-siRNA (h) was synthesized from SANTA CRUZ BIOTECHNOLOGY, Inc. The plasmids were transfected into cells using Lipofectamine RNAiMAX (Invitrogen) and were incubated for 48 h according to the manufacturer’s instructions. Stable cell lines were selected using the appropriate antibiotics for at least 48 h after transfection.
Transwell assay
Transwell assay was performed using the Matrigel-coated (8 lm pore size; BD, Franklin Lakes, NJ, USA) filters in 24-well plates. Briefly, cells were trypsinized and seeded onto the upper chamber of the transwells (1 × 105 cells/well) in supplement-free serum DMEM medium. The lower chamber of the transwells was filled with the DMEM medium (including 10 % fetal bovine serum).The chambers were incubated at 37 °C with 5 % CO2 for 24 h. At the end of incubation, cells on the upper surface of the filter were removed using a cotton swab. Cells migrating through the filter to the lower surface were fixed with 4 % paraformaldehyde for 10 min and stained with 0.1 % crystal violet for 10 min. Migrated cells were viewed and photographed under a phase-contrast microscope (Olympus, Tokyo, Japan) and counted in five randomly chosen fields.
Protein extraction and Western blot analysis
Cells were washed three times with ice-cold phosphate-buffered saline (PBS) and lysed in RIPA buffer (50 mM Tris (pH 7.4), 150 mM NaCl, 0.5 % sodium deoxycholate, 1 mM EDTA, 1 % Triton X-100) containing fresh protease, and phosphatase inhibitor cocktails (Sigma) by incubating for 20 min at 4 °C. The protein concentration was determined using the Bio-Rad assay system (Bio-Rad, Hercules, CA, USA). Equal amounts of protein extracts (30 μg) were subjected to 10 % sodium dodecyl sulfate–polyacrylamide (SDSPAGE) gel electrophoresis and transferred to polyvinylidenedifluoride (PVDF) membranes (Millipore, Billerica, MA) and sequentially incubated with indicated primary antibodies against E-cadherin, N-cadherin (1:1000, Cell Signaling Technology),YAP, and GAPDH (1:1000, Cell Signaling Technology) overnight at 4 °C. Horseradish peroxidase (HRP)-conjugated secondary antibody (1:2000, Abcam) was incubated at room temperature for 1 h. The blots were developed using enhanced chemiluminescence detection reagents and scanned with a Molecular Imager system (Bio-Rad).
Statistical analysis
Each experiment was repeated at least three times. Derived values were presented as the mean ± SD. Student’s t test (two tailed) or Student–Newman–Keuls (SNK test, ANOVA) was employed to analyze the differences using SPSS 13.0 software. P < 0.05 was considered to be statistically significant.
Results
Knockdown of YAP is involved in the invasive ability of HCC cell lines
To assess the effect of YAP knockdown in HCC cell invasive ability, the transwell assay was employed. We transfected sequences of YAP-siRNA or control-siRNA (consists of a scrambled sequence that will not lead to the specific degradation of any cellular message). The results showed that the cells number of YAP-siRNA group was significantly decreased in MHCC97H compared with the control group (66 ± 6.89 vs 117 ± 7.23, P < 0.05) (Fig. 1a, b), and compared with the control group, the number of the YAP-siRNA group was also significantly decreased in MHCC97L (40 ± 2.65 vs 77 ± 4.33, P < 0.05) (Fig. 1a, b). The result indicated that knockdown of YAP inhibits the invasive ability of HCC cell lines.
The invasive ability of MHCC97H and MHCC97L cells can be blocked by YAP downregulation. a the change of MHCC97H and MHCC97L cells number in the YAP-siRNA group and the control group. b Compared with the control group, MHCC97H cells (66 ± 6.89 vs 117 ± 7.23, P < 0.05) and MHCC97L cells (40 ± 2.65 vs 77 ± 4.33, P < 0.05) in YAP-siRNA (h) group were significantly decreased compared with the control group, the figure shows mean (mean) and standard error (SE), *P < 0.05, optical microscope magnification (×200)
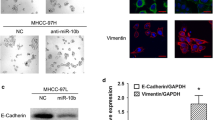
Knockdown of YAP changed the mRNA and protein levels of EMT markers in MHCC-97H cells
In order to examine the effects of YAP knockdown in MHCC-97H cell line, we transfected two sequences of YAP-siRNA (1 and 2) or control-siRNA. At 72 h, after YAP-siRNA compared with the control group, we observed that the YAP-siRNA group in MHCC97H showed obviously higher protein expression levels of E-cadherin (P < 0.05), and lower expression of N-cadherin (P < 0.05) (Fig. 2a, b). Compared with the control group, the mRNA levels of E-cadherin increased (P < 0.05), but the mRNA levels of N-cadherin and vimentin did not significantly change (P > 0.05), indicating some effects of post-transcriptional regulation mechanism after knockdown of YAP in MHCC97H (Fig. 4a).
YAP-specific siRNA effectively suppressed the protein level of EMT marker after 72 h in MHCC97H. a The protein level of E-cadherin compared with the control group was up-regulated (P < 0.05), N-cadherin in the experimental group was down-regulated (P < 0.05). b Semiquantification of Western blot bands shown in densitometric analysis of E-cadherin and N-cadherin bands was performed and normalized with that of GAPDH. The significance of the difference was assessed using student’s t test, GAPDH as an internal control, the figure shows mean (mean) and standard error (SE), *P < 0.05
Silencing of YAP changed the mRNA and protein levels of EMT markers in MHCC-97L cells
MHCC97L cells were also transiently transfected by YAP-siRNA, and were examined by Western blotting and real-time polymerase chain reaction. In MHCC97L cells, compared with the control group, the protein expression of E-cadherin was also significantly increased (P < 0.05); however, the protein expression of N-cadherin did not significantly change (P > 0.05) (Fig. 3a, b). The result of real-time polymerase chain reaction indicated that mRNA levels of E-cadherin were increased (P < 0.05), but mRNA levels of N-cadherin were not significantly changed (P > 0.05), compared with the control group (Fig. 4b).
YAP-specific siRNA effectively suppressed the protein level of EMT marker after 72 h in MHCC97L. a The protein level expression of E-cadherin was significantly increased (P < 0.05); however, N-cadherin expression did not significantly change (P > 0.05). b Semiquantification of Western blot bands shown in Densitometric analysis of E-cadherin and N-cadherin bands was performed and normalized with that of GAPDH. The significance of the difference was assessed using student’s t test, GAPDH as an internal control, the figure shows mean (mean) and standard error (SE), *P < 0.05
Discussion
Recently, growing evidence has shown that tumor progression, including local invasion, spreading through the circulation and metastasis, is mediated by EMT [10]. Several cancer-associated cascades have emerged as important regulatory signaling for EMT. These include phosphoinositide 3-kinase (PI3 K)/Akt, Wnt, Notch, Hedgehog, and nuclear factor-κB (NF-κB)-dependent pathways [11–13]. As EMT markers, the downregulation of E-cadherin and upregulation of N-cadherin protein play a promoting factor in tumor cell invasion and metastasis [14, 15]. YAP overexpression has been demonstrated nuclei associated with the development of a variety of tumors, and is considered a tumorigenic gene [16]. In vivo, YAP1 has been reported to be potently prometastatic in breast cancer and melanoma cells; the metastatic potential of breast cancer and melanoma cells is strongly correlated with increased TEAD transcriptional activity, and increased YAP/TEAD activity plays a causal role in cancer progression and metastasis [9]. The association of YAP with EMT of HCC had not been thoroughly investigated.
In the present study, we found that knockdown of YAP in MHCC97H showed obviously higher expression of E-cadherin compared with the control group (P < 0.05), and lower expression of N-cadherin (P < 0.05). In MHCC97L cells, the expression of E-cadherin was also significantly increased (P < 0.05); however, N-cadherin expression did not significantly change (P > 0.05). Knockdown of YAP can cause changes in protein levels of EMT markers. For the result of different N-cadherin expression in the two cell lines, we consider MHCC97L cell lines may be low migratory potential, whose EMT phenomenon caused by the presence of the cell itself is not obvious, so the mesenchymal markers N-cadherin did not change significantly. Additionally, Transwell invasion assay showed that the number of the transfected group cells was significantly decreased in MHCC97H and MHCC97L (P < 0.05), compared with the control group. The invasion assay confirmed that the silencing of YAP protein significantly inhibits the invasion capacity of HCC cell lines, indicating that inhibition of the expression of YAP protein can suppress the invasive ability of HCC.
YAP may regulate EMT through multiple mechanisms. Some studies delineate one mechanism, in which YAP1 is required for TGFβ signaling by interacting with the Smad2/3/4 complex. Interestingly, a recent study also linked Hippo signaling pathway with TGFβ signaling by showing that TGFβ stimulates Smad2/3/4 binding to WWTR1 (also known as TAZ), a YAP1 paralogue. As a result, WWTR1 was recruited to TGFβ response elements in human embryonic stem cells. Loss of WWTR1 led to failure of Smad2/3/4 complexes to accumulate in the nucleus and activate transcription [17, 18]. In human breast cancer cell line MCF10A cells, Michael Overholtzer et al. found that overexpression of YAP protein can promote breast cancer MCF10A cells EMT phenomenon. Silencing expression of MCF7 breast cancer cell line Hs578T in YAP protein significantly reduced tumor cell migration and invasion [7]. In HCT116 colon cancer cells, the capacity for proliferation, metastasis, and invasion was dramatically reduced by knockdown of YAP and TAZ. Co-overexpression of YAP and TAZ is an independent predictor of prognosis for patients with CRC [19]. Nallet-Staub et al. found that Stable YAP knockdown dramatically reduced the expression of the classical Hippo target CCN2/connective-tissue growth factor (CTGF), as well as anchorage-independent growth, capacity to invade Matrigel. Inversely, YAP overexpression increased melanoma cell invasiveness, associated with increased TEA domain-dependent transcription and CCN2/CTGF expression [20]. Our experiments found that knockdown of YAP in MHCC97L and MHCC97H cells dramatically inhibits the invasive ability of cells. The expression of YAP is associated with EMT of HCC. In MHCC97L and MHCC97H cells, the mRNA levels of N-cadherin did not change difference (P > 0.05), we consider that there maybe some post-transcriptional regulation mechanism. Yu et al. found that yes-associated protein 1 (YAP1) as a novel target of miR-200a and found that targeting of YAP1 by miR-200a resulted in decreased expression of proapoptotic proteins, which leads to anoikis resistance. Overexpression of miR-200a protected tumor cells from anoikis and promoted metastases in vivo [21].
In summary, the present study conclusively presents evidence of the following: that YAP knockdown is able to suppress cell invasion in MHCC97H and MHCC97L by modulating the characteristic markers of EMT. Furthermore, the association of YAP involving in EMT of HCC using mice needs to be further confirmed. Collectively, a novel molecular mechanism of HCC EMT could be proposed, based on which a potentially effective therapeutic approach could be developed for the inhibition of invasion, and metastasis of HCC.
References
Jemal A, Bray F, Center MM, Ward E, Forman D. Global cancer statistics. CA Cancer J Clin. 2011;61:69–90.
Roayaie S, Obeidat K, Sposito C, Mariani L, Bhoori S, Pellegrinelli A, et al. Resection of hepatocellular cancer ≤2 cm: results from two Western centers. Hepatology. 2013;57:1426–35.
Mann CD, Neal CP, Garcea G, Manson MM, Dennison AR, Berry DP. Prognostic molecular markers in hepatocellular carcinoma: a systematic review. Eur J Cancer. 2007;43:979–92.
Kalluri R, Weinberg RA. The basics of epithelial-mesenchymal transition. J Clin Invest. 2009;119:1420–8.
Thiery JP, Acloque H, Huang RY, Nieto MA. Epithelial-mesenchymal transitions in development and disease Cell. 2009;139:871–90.
Pan D. The hippo signaling pathway in development and cancer. Dev Cell. 2010;19:491–505.
Zhao B, Li L, Lei Q, Guan KL. The Hippo-YAP pathway in organ size control and tumorigenesis: an updated version. Genes Dev. 2010;24:862–74.
Xu MZ, Yao TJ, Lee NP, Ng IO, Chan YT, Zender L, et al. Yes-associated protein is an independent prognostic marker in hepatocellular carcinoma. Cancer. 2009;115:4576–85.
Lamar JM, Stern P, Liu H, Schindler JW, Jiang ZG, Hynes RO. The Hippo pathway target, YAP, promotes metastasis through its TEAD-interaction domain. Proc Natl Acad Sci USA. 2012;109:E2441–50.
Yang J, Weinberg RA. Epithelial-mesenchymal transition: at the crossroads of development and tumor metastasis. Dev Cell. 2008;14:818–29.
Iwatsuki M, Mimori K, Yokobori T, Ishi H, Beppu T, Nakamori S, et al. Epithelial-mesenchymal transition in cancer development and its clinical significance. Cancer Sci. 2010;101:293–9.
van Zijl F, Zulehner G, Petz M, Schneller D, Kornauth C, Hau M, et al. Epithelial-mesenchymal transition in hepatocellular carcinoma. Future Oncol. 2009;5:1169–79.
Matsumura T, Makino R, Mitamura K. Frequent down-regulation of E-cadherin by genetic and epigenetic changes in the malignant progression of hepatocellular carcinomas. Clin Cancer Res. 2001;7:594–9.
Zhou ZJ, Dai Z, Zhou SL, Hu ZQ, Chen Q, Zhao YM, et al. HNRNPAB induces epithelial-mesenchymal transition and promotes metastasis of hepatocellular carcinoma by transcriptionally activating SNAIL. Cancer Res. 2014;74:2750–62.
Derycke LD, Bracke ME. N-cadherin in the spotlight of cell-cell adhesion, differentiation, embryogenesis, invasion and signalling. Int J Dev Biol. 2004;48:463–76.
Zhao B, Lei QY, Guan KL. The Hippo-YAP pathway: new connections between regulation of organ size and cancer. Curr Opin Cell Biol. 2008;20:638–46.
Varelas X, Sakuma R, Samavarchi-Tehrani P, Peerani R, Rao BM, Dembowy J, et al. TAZ controls Smad nucleocytoplasmic shuttling and regulates human embryonic stem-cell self-renewal. Nat Cell Biol. 2008;10:837–48.
Zhang H, von Gise A, Liu Q, Hu T, Tian X, He L, et al. Yap1 is required for endothelial to mesenchymal transition of the atrioventricular cushion. J Biol Chem. 2014;289:18681–92.
Wang L, Shi S, Guo Z, Zhang X, Han S, Yang A, et al. Overexpression of YAP and TAZ is an independent predictor of prognosis in colorectal cancer and related to the proliferation and metastasis of colon cancer cells. PLoS One. 2013;8:e65539.
Nallet-Staub F, Marsaud V, Li L, Dodier S, Bataille V, Bataille V, et al. Pro-invasive activity of the hippo pathway effectors YAP and TAZ in cutaneous melanoma. J Invest Dermatol. 2014;134:123–32.
Yu SJ, Hu JY, Kuang XY, Luo JM, Hou YF, Di GH, et al. MicroRNA-200a promotes anoikis resistance and metastasis by targeting YAP1 in human breast cancer. Clin Cancer Res. 2013;19:1389–99.
Acknowledgments
We thank that the Laboratory staffs from Third Affiliated Hospital of Sun Yat-Sen University (Guangzhou, Guangdong, China) and Department of General Surgery, Xinhua Hospital, Shanghai Jiaotong University School of Medicine, (Shanghai, China) for the contribution.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Financial support
This study is supported by China National Natural Science Foundation (No. 81172038).
Additional information
S. Wang and H. Li contributed equally to this work.
Rights and permissions
About this article
Cite this article
Wang, S., Li, H., Wang, G. et al. Yes-associated protein (YAP) expression is involved in epithelial–mesenchymal transition in hepatocellular carcinoma. Clin Transl Oncol 18, 172–177 (2016). https://doi.org/10.1007/s12094-015-1353-4
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12094-015-1353-4