Abstract
Introduction
Platinum-based chemotherapy and 3rd generation drugs is still the main treatment option for advanced non-small cell lung cancer (NSCLC) patients without activating EGFR mutations or ALK rearrangements. However, the side effects associated with cytostatics are well known. Changes in the genes (e.g. single nucleotide polymorphisms, SNPs) encoding proteins regulating DNA repair or cell division could potentially influence on both the susceptibility of cancer cells to chemotherapy, and the occurrence of toxicities.
Materials and methods
In presented study, the relationship between the fourteen SNPs in nine DNA repair and cell division regulating genes: ERCC1, XPD, XPA, XPC, XRCC1, XPG, RRM1, BRCA1, STMN1 and the toxicity of first-line chemotherapy in NSCLC patients were investigated. SNPs were determined by SNaPshot PCR® in DNA isolated from peripheral blood of 55 NSCLC patients treated with platinum compound and vinorelbine. The toxicity of therapy was evaluated according to the Common Toxicity Criteria (CTC) Version 4.03.
Results
The odds ratio (OR) of severe haematological toxicity was significantly lower in carriers of the T allele of XRCC1 gene (1196A > G, OR = 0.22, 95 % CI: 0.06–0.82, p = 0.018) and higher in the carriers of the T allele (2704C > A) of XPC gene (OR: 7.50, 95 % CI: 0.89–63.17, p = 0.036) compared to the remaining patients. Risk of severe hepatotoxicity was significantly lower in carriers of the C allele of STMN1 (−2166T > C, OR = 0.09, 95 % CI: 0.01–1.12, p = 0.025) than in patients with T allele of this gene. In carriers of G allele (2251A > C, OR: 0.24, 95 % CI: 0.07–0.81, p = 0.017) and T (934G > A, OR: 0.26, 95 % CI: 0.07–0.90, p = 0.029) of XPD gene, risk of severe nephrotoxicity was significantly lower than in other patients.
Conclusions
Selected SNPs of genes encoding DNA repair enzymes and cell division regulation proteins could be useful biomarkers for prediction of platinum and vinorelbine-based chemotherapy toxicity in patients with advanced NSCLC.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Lung cancer (85 % of cases are represented by NSCLC) is still the leading cause of death from malignancies in the world [1, 2]. This is despite the dynamic development of early diagnostic methods, molecularly targeted therapies and immunotherapy of cancer. The majority of NSCLC patients are diagnosed at an advanced stage of disease, which limits the therapeutic options. Therefore, systemic therapy, based on chemo- or chemoradiotherapy, is the most important method of treatment of NSCLC patients. However, chemotherapy is characterized by moderate efficacy and significant toxicity. Molecularly targeted drugs (tyrosine kinases inhibitors of EGFR, e.g. erlotinib, gefitinib, afatinib or ALK, e.g. crizotinib, ceritinib) are more effective, however, only in patients with specific molecular abnormalities (activating mutations in the EGFR gene or ALK gene rearrangements) [3, 4]. In the first line of NSCLC treatment, a combination of platinum compound (cisplatin or carboplatin) and third generation drug (gemcitabine, vinorelbine, pemetrexed, docetaxel or paclitaxel) is used [5]. The various cytostatic drugs have different mechanisms of action: direct or indirect damage of DNA, interfering of DNA replication or damage of the mitotic spindle. Due to the cell structure destruction and blocking life processes, cytostatics affect both normal and cancerous cells and cause numerous side effects.
STMN1 (oncoprotein-18) is a protein related to microtubule dynamics and regulation of the cell cycle [11, 12]. Expression of STMN1 and the presence of different tubular protein isoforms (e.g. TUBB3) have the greatest impact on the possibility of cell proliferation. In available literature, there are no data about influence of STMN1 gene polymorphisms (including −2166T > C, rs182455) on the chemotherapy toxicity in lung cancer patients. However, on the basis of knowledge about the correlation between the expression of STMN1 and efficacy of therapies based on taxanes or vinca alkaloids, it can be assumed that the STMN1 gene polymorphisms could be considered as a predictive factor in lung cancer patients [6, 7].
DNA repair capacity plays important roles in carcinogenesis, response to cancer treatment, and toxicity of chemotherapy. Polymorphisms (e.g. single nucleotide polymorphisms, SNPs) of the genes encoding DNA repair enzymes associated with the changes of DNA repair effectiveness may influence on both susceptibility of tumour cells to chemotherapy as well as the occurrence of the related toxicity. The above hypothesis is confirmed by some of the recently published researches. Several SNPs of genes encoding enzymes involved in different mechanisms of DNA repair, including nucleotide excision repair (NER): ERCC1, XPA, XPC, XPG, XPD, MMS18L, base excision repair (BER): XRCC1, BRCA1, mismatch repair (MMR): RECQ1 as well as nucleotide synthesis: RRM1, TS, MTHFR, have been investigated in patients with advanced NSCLC [8–13]. These SNPs, associated with lung cancer risk and response to treatment, may be also the predictors for toxicity of chemotherapy [14–17]. Unfortunately, only few clinical trials, that assess the association between SNPs of DNA repair genes and the toxicity of various chemotherapy regimens, are available in literature. In most cases, these are retrospective studies and the obtained results are often inconsistent, which further complicates their unequivocal evaluation.
The aim of this study was to evaluate the relationship between the 14 SNPs located in 9 genes regulating DNA repair or cell division (ERCC1: 19007C > T, rs11615; 8092C > A, rs3212986; XPD: 2251A > C, rs13181; 934G > A, rs1799793; XPA: 4A > G, rs1800975; XPC: 1385C > T, rs2228000; 2704C > A, rs2228001; XRCC1: 580C > T, rs1799782; 1196A > G, rs25487; XPG: 3310G > C, rs17655; RRM1: −37C > A, rs12806698; −524C > T, rs11030918; BRCA1: 181T > A/C/G, rs28897672; STMN1: −2166T > C, rs182455) and the toxicity of first-line chemotherapy based on platinum and vinorelbine in advanced NSCLC patients.
Materials and methods
The study group
This retrospective study included 55 Caucasian patients with inoperable, locally advanced or advanced NSCLC (IIIB and IV) treated in 2010–2013 at the Department of Pneumonology, Oncology and Allergology, Medical University of Lublin. The project was approved by the Committee of Ethics and Research at the Medical University of Lublin (no. consent: KE-0254/142/2010). The condition of participation in the study was patients’ written consent to the use of clinical data and material in the form of peripheral blood. NSCLC diagnoses were based on pathomorphological examination. Standard regimen and dosing of chemotherapy were used in the I line of chemotherapy (recommended by Polish Society of Clinical Oncology consistent with the guidelines of the European Society for Medical Oncology, ESMO and the National Comprehensive Cancer Network, NCCN). All patients received platinum compounds and vinorelbine.
Stage of a disease was evaluated according to TNM classification (VII edition by the Union for International Cancer Control, UICC). The median number of cycles of I-line chemotherapy was 4 (4–6). Based on an interview and the available medical documentation detailed demographic and clinical data (gender, age, smoking status, type of NSCLC, stage of disease, weight loss and performance status, type and number of cycles of chemotherapy, side effects) were collected. Response to treatment was evaluated by RECIST Version 1.1 (Response Evaluation Criteria in Solid Tumours). Adverse events were assessed after 2nd and 4th cycle, based on CTC Version 4.03 (Common Toxicity Criteria). Haemoglobin level as well as blood red and white cells number and percentage were assessed before any medication of anaemia or bone marrow damage (e.g. red blood cells transfusion or granulocyte colony-stimulating factor (G-CSF) administration). The later obtained data were discarded. The degree of renal failure was determined on the basis of serum creatinine level and glomerular filtration rate (eGFR). Serum bilirubin and transaminases (AST, ALT) levels were used for estimation of liver failure. The factors describing the toxicity were observed for 4 weeks after the chemotherapy termination.
The applied methods
For the isolation of DNA from peripheral blood leukocytes, DNA Blood Mini Kit (Qiagen, Canada) was used. The quantity and quality of extracted DNA were performed using a spectrophotometer BioPhotometer plus cuvette equipped with filters UV/IS (Eppendorf, Germany). Analysis of SNPs of studied genes was carried out by the mini-sequencing technique (SNaPshot® PCR) and ABI PRISM SNaPshot® Multiplex (Life Technologies, USA).
Genotyping results of analysed genes were retrospectively related to demographic and clinical characteristics and the occurrence of chemotherapy toxicity (haematological and non-haematological). Statistical analysis of the results was performed using the computer software MedCalc Version 10 (MedCalc Software, Belgium). p < 0.05 was considered statistically significant. The Hardy–Weinberg (HW) equilibrium and the Chi-Square (χ 2) test were used for assessment of allele and genotypes frequencies as well as for evaluation of relationship demographic and clinical factors with the distribution of polymorphic variants of the studied genes.
Results
Clinical characteristics
Baseline characteristics of study population are presented in Table 1. None of patients has received radical radiotherapy; however, 14.5 % of patients were radiated as palliative treatment to reduce symptoms caused by airway obstruction or by distant metastasis. There was no complete remission (CR) as a result of first-line chemotherapy. Control of the disease was recorded in 70.9 % of patients, of which the PR and SD occurred in 20 % and 50.9 % of patients. PD was observed in 29.1 % of patients. The median progression-free survival (PFS) and follow-up time were 5 ± 3 and 9 ± 3 months, respectively.
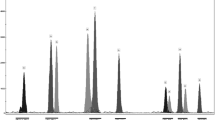
SNPs analysis
The genotypes distribution of investigated genes is shown in Table 2. Only AA homozygotes (100 %) of BRCA1 gene were found in the study group. Accordingly, the polymorphism of this gene was not included in the statistical analysis. Genotype frequencies were in accordance with Hardy–Weinberg equilibrium model and consistent with previous studies (if they were available).
Chemotherapy toxicity
Patients who received at least two cycles of chemotherapy were evaluated for possible side effects. Severe toxicity (grade 2–4) was detected in 17 patients (30.9 %) after second and in 29 patients (52.7 %) after fourth cycle of chemotherapy, including all assessed types of toxicity. H aematologic toxicity was most common adverse events. Grade 2–4 haematologic toxicity after second cycle of chemotherapy appeared in 4 patients (7.3 %), whereas grade 2–4 toxicity after fourth cycle of chemotherapy—in 14 patients (25.5 %). Lack of haematological toxicity was recorded in 15 patients (27.3 %) after second cycle of chemotherapy and in 4 patients (7.3 %) after forth cycle of chemotherapy. Severe hepatotoxicity was not found in any patient after 2nd cycle of chemotherapy, but its occurrence was observed in 3 patients (5.5 %) after 4th cycle of chemotherapy. Hepatotoxicity was not detected in 47 patients (85.5 %) after 2nd cycle of chemotherapy and in 43 patients (78.2 %) after 4th cycle of chemotherapy. Grade 2–4 hepatotoxicity was recorded in 15 patients (27.3 %) after 2nd cycle of chemotherapy and 16 patients (29.1 %) after 4th cycle of chemotherapy. No nephrotoxicity was observed in 18 (32.7 %) and 16 (29.1 %) patients, retrospectively. Severe nephrotoxicity after 2nd cycle of chemotherapy was observed significantly more frequently in elderly patients (≥64 years) compared to younger patients (<64 years) (p = 0.001, χ 2 = 14.610). Other toxicities occurred with similar frequency in groups of patients with different clinical-demographic characteristics (Table 3).
SNPs and chemotherapy toxicity
Association between toxicity after chemotherapy and SNPs in genes encoding proteins regulating DNA repair and mitotic spindle were presented in Supplementary Tables 1S–3S. The odds ratio (OR) of early (after 2nd cycle of chemotherapy) severe haematological toxicity was significantly lower in carriers of G allele of XPD gene (934G > A, OR = 0.08, 95 % CI 0.01–0.40, p = 0.0005) and XPA gene (4A > G, OR = 0.07; 95 % CI 0.01–1.41, p = 0.018) than in carriers of A allele of these genes. Risk of early severe nephrotoxicity was significantly lower in carriers of C allele of XPD gene (2251A > C, OR = 0.07, 95 % CI 0.02–0.31, p < 0.0001) than in patients with A allele of this gene.
The OR of severe haematological toxicity after 4th chemotherapy cycle was significantly lower in carriers of A allele of XRCC1 gene (1196A > G, OR = 0.22, 95 % CI 0.06–0.82, p = 0.018), however, significantly higher in carriers of A allele of XPC gene (2704C > A,OR = 7.50, 95 % CI 0.89–63.17, p = 0.036) compared to patients with other alleles of these genes. The OR of severe hepatotoxicity after 4th chemotherapy cycle was significantly lower in carriers of C allele of STMN1 gene (−2166T > C, OR = 0.09, 95 % CI 0.01–1.12, p = 0.025) than in carriers of T allele of this gene. Risk of severe nephrotoxicity after 4th chemotherapy cycle was significantly lower in carriers of C allele (2251A > C, OR = 0.24, 95 % CI 0.07–0.81, p = 0.017) and A allele (934G > A, OR = 0.26, 95 % CI 0.07–0.90, p = 0.029) of XPD gene compared to patients carried A or G allele of this gene. No statistically significant association between the other examined SNPs and chemotherapy toxicities was found.
Discussion
Cytostatic drugs, used currently in chemotherapy of NSCLC, are harmful for both tumour and normal cells. Direct or indirect damage of the genetic material, related to the regulation of cell division, occurs in the rapidly proliferating and active cells. Numerous side effects in bone marrow, kidneys and liver are observed at the site of cytostatics metabolism and after cytostatics exposure. Alkylating agents (platinum compounds: cis- and carboplatin) and inhibitors of mitosis through interaction with tubulin (vinorelbine, docetaxel, paclitaxel) induce myelosuppression, renal and liver failure, hair loss, diarrhoea, nausea and vomiting, peripheral neuropathy, weakness, hearing disorders [18].
Qualification of NSCLC patients to different chemotherapy regimens is based mainly on the performance status of the patient, convenience of the drugs use and the personal experiences of physician. However, currently available chemotherapy regimens are characterized by significant differences in toxicity. It is clear that toxicity profile is not applies equally to all patients and is associated with molecular differences [6, 7, 19–21]. Changes in the structure, function or expression of particular proteins are conditioned by the occurrence of SNPs in coding or non-coding sequences (mainly promoter) of genes [22]. SNPs analysis can be realized in materials that are easy to obtain (e.g. DNA from peripheral blood leukocytes). Consequently, in many studies (unfortunately mainly retrospective), the effects of the individual polymorphic variants of different genes on the effectiveness and toxicity of the chemotherapy regimens were examined. However, most of the major research was carried out on Asian patients. Moreover, the results presented in the literature are often contradictory and inconclusive.
Zhang et al. [8] examined polymorphisms of ERCC5, ERCC6, MMS19L, CCNH, XPC, RRM1 genes in 365 Asian patients with locally advanced or advanced NSCLC treated with platinum-based chemotherapy. Authors showed that presence of G allele in codon 811 of MMS19L gene was associated with the occurrence of haematological toxicity (leukopenia, thrombocytopenia), hepatotoxicity (icterus) and nephrotoxicity. However, polymorphism C37A (rs 12806698) in RRM1 gene was associated with higher incidence of vomiting and D1104H (rs17655) in ERCC5 gene—with susceptibility to infections. Lambet al. [23] showed that SNPs in ERCC4 and XPC genes were significantly related to risk of neutropenia in 90 Caucasian male patients treated with the combination of carboplatin and paclitaxel. Wu et al. [11] noted that the incidence of severe haematologic toxicity (especially leucopoenia) was significantly higher in the AA genotype carriers (396A > C, rs238406) of XPD gene in 209 Asian NSCLC patients received chemotherapy based on platinum compounds. Two other SNPs (934G > A, rs1799793; 2133C > T, rs1052555) of this gene had no effect on the occurrence of chemotherapy toxicity. Suk et al. [10] showed a relationship between the presence of A allele of ERCC1 gene (8092C > A, rs3212986) and an increased risk of serious gastrointestinal tract toxicity in 214 Caucasian patients with inoperable or advanced NSCLC treated with platinum-based chemotherapy.
Many authors have failed to find any association between the occurrence of DNA repair genes polymorphisms and risk of chemotherapy toxicity. An example is a study of Li et al. conducted in 115 Asian and locally advanced or metastatic NSCLC patients treated with platinum-based chemotherapy. SNPs 2251A > C (rs13181) of XPD gene and 1196 > G (rs25487) of XRCC1 gene were not significantly associated with haematological and gastrointestinal toxicity as well as hepatotoxicity [24]. Sullivan et al. [25] examined 116 Caucasian NSCLC Caucasian patients treated platinum-based chemotherapy. Authors analysed 17 SNPs in 8 genes (ERCC1: rs11615, rs3212948, rs3212986, ERCC2/XPD: rs1799793, rs13181; ERCC3/XPB: rs4150454, rs4150402, rs3738948; ERCC4/XPF: rs1799801; ERCC5/XPG: rs1047768, rs17655; XPA: rs1800975; XRCC1: rs25487, rs25489, rs1799782, rs3213239, XRCC2, rs3218536) related to DNA repair. They did not find any association between these polymorphisms and haematological and gastrointestinal toxicities.
In the present study, we showed that the risk of early, severe haematological toxicity or nephrotoxicity significantly depends on polymorphisms in XPD and XPA gene in NSCLC patients treated with platinum compounds and vinorelbine. In contrast, a higher risk of severe haematological toxicity after 4th chemotherapy cycle correlated with specific genotypes of XPC, XRCC1 and XPD genes.
At present, no data are available about the role of polymorphisms of STMN1 gene (including rs 182455) in sensitivity to chemotherapy and risk of chemotherapy toxicity in NSCLC patients. In studies conducted in breast and ovarian cancer cell lines, Alla et al. and Balachandran et al. [26, 27] demonstrated that the increased expression of STMN1 reduced microtubule polymerization with significantly reduction of paclitaxel binding. The increased expression of STMN1 leads to increased vinblastine’s annealing, indicating that the disorders in expression of STMN1 may be associated not only with resistance to the taxanes but also to vinca alkaloids. Meng et al. [7] showed that a low level of STMN1 expression is a favourable predictor of response to neoadjuvant chemotherapy based on docetaxel in 54 women with advanced breast cancer. Both vinca alkaloids and taxanes affect not only tumour cells. Therefore, disturbances in the expression of the STMN1 gene can influence on side effects of chemotherapy. In the present study, for the first time, the relationship of SNP −2166T > C of STMN1 gene with hepatotoxicity was described in NSCLC patients treated with platinum compounds and vinorelbine.
Undoubtedly, the limitations of this study are retrospective nature and small examined group. While, the advantages of the present study are homogenous group of patients (treated only with platinum compounds and vinorelbine first-line chemotherapy) and large number of analysed polymorphisms (14 SNPs located in 9 genes). However, in order to verify the obtained results large prospective study should be carried out.
Conclusions
As shown, several SNPs of genes, whose proteins are involved in the mechanism of action of currently used cytostatics may play important role in predicting the adverse events of platinum compounds and vinorelbine chemotherapy in NSCLC patients. Probably, different types of chemotherapy toxicities are depend on SNPs in XPX, XPD, XRCC1 and STMN1 genes. Determination of selected SNPs of genes encoding DNA repair enzymes and protein associated with regulation of cell division may become a useful tool for predicting the toxicity associated with chemotherapy in NSCLC patients.
References
Cancer incidence in five continents, vol. X (electronic version) Lyon, IARC. http://ci5.iarc.fr. last accessed on 06 Dec.2014.
Heuvers ME, Hegmans JP, Stricker BH, Aerts JG. Improving lung cancer survival; time to move on. BMC Pulm Med. 2012;12:77.
Revannasiddaiah S, Thakur P, Bhardwaj B, Susheela SP, Madabhavi I. Pulmonary adenocarcinoma: implications of the recent advances in molecular biology, treatment and the IASLC/ATS/ERS classification. J Thorac Dis. 2014;6(Suppl 5):S502–25.
Stinchcombe TE. Novel agents in development for advanced non-small cell lung cancer. TherAdv Med Oncol. 2014;6(5):240–53.
NCCN Clinical Practice Guidelines in Oncology (NCCN Guidelines®) Non-small cell lung cancer Version 1.2015 (2014) www.nccn.org. last accessed on 06.Dec 2014.
Rosell R, Scagliotti G, Danenberg KD, Lord RV, Bepler G, Novello S. Transcripts in pretreatment biopsies from a three-arm randomized trial in metastatic non-small-cell lung cancer. Oncogene. 2003;22:3548–53.
Meng XL, Su D, Wang L, Gao Y, Hu YJ, Yang HJ, et al. Low expression of stathmin in tumor predicts high response to neoadjuvant chemotherapy with docetaxel-containing regimens in locally advanced breast cancer. Genet Test Mol Biomarkers. 2012;16:689–94.
Zhang L, Gao G, Li X, Ren S, Li A, Xu J, et al. Association between single nucleotide polymorphisms (SNPs) and toxicity of advanced non-small-cell lung cancer patients treated with chemotherapy. PLoS ONE. 2012;7(10):e48350.
Joerger M, Burgers SA, Baas P, Smit EF, Haitjema TJ, Bard MP, et al. Germline polymorphisms in patients with advanced nonsmall cell lung cancer receiving first-line platinum-gemcitabine chemotherapy: a prospective clinical study. Cancer. 2012;118(9):2466–75.
Suk R, Gurubhagavatula S, Park S, Zhou W, Su L, Lynch TJ, et al. Polymorphisms in ERCC1 and grade 3 or 4 toxicity in non-small cell lung cancer patients. Clin Cancer Res. 2005;11(4):1534–8.
Wu W, Zhang W, Qiao R, Chen D, Wang H, Wang Y, et al. Association of XPD polymorphisms with severe toxicity in non-small cell lung cancer patients in a Chinese population. Clin Cancer Res. 2009;15(11):3889–95.
Li X, Shao M, Wang S, Zhao X, Chen H, Qian J, et al. Heterozygote advantage of methylenetetrahydrofolate reductase polymorphisms on clinical outcomes in advanced non-small cell lung cancer (NSCLC) patients treated with platinum-based chemotherapy. Tumour Biol. 2014;35(11):11159–70.
Krawczyk P, Kucharczyk T, Kowalski DM, Powrózek T, Ramlau R, Kalinka-Warzocha E, et al. Polymorphisms in TS, MTHFR and ERCC1 genes as predictive markers in first-line platinum and pemetrexed therapy in NSCLC patients. J Cancer Res ClinOncol. 2014;140:2047–57.
Wang Y, Liu ZD, Zhao LM, Du CX, Xi XM, Mi YL, et al. Individualized treatment of NSCLC: from research to clinical practice. Neoplasma. 2013;60(5):538–45.
Zhao H, Zhang H, Du Y, Gu X. Prognostic significance of BRCA1, ERCC1, RRM1, and RRM2 in patients with advanced non-small cell lung cancer receiving chemotherapy. Tumour Biol. 2014. [Epub ahead of print].
Qian B, Zhang H, Zhang L, Zhou X, Yu H, Chen K. Association of genetic polymorphisms in DNA repair pathway genes with non-small cell lung cancer risk. Lung Cancer. 2011;73(2):138–46.
Dong J, Hu Z, Shu Y, Pan S, Chen W, Wang Y, et al. Potentially functional polymorphisms in DNA repair genes and non-small-cell lung cancer survival: a pathway-based analysis. MolCarcinog. 2012;51(7):546–52.
Mazzone P, Mekhail T. Current and emerging medical treatments for non-small cell lung cancer: a primer for pulmonologists. Respir Med. 2012;106(4):473–92.
Bowden NA. Nucleotide excision repair: why is it not used to predict response to platinum-based chemotherapy? Cancer Lett. 2014;346(2):163–71.
Robertson AB, Klungland A, Rognes T, Leiros I. DNA repair in mammalian cells: base excision repair: the long and short of it. Cell Mol Life Sci. 2009;66(6):981–93.
Bonanno L, Favaretto A, Rosell R. Platinum drugs and DNA repair mechanisms in lung cancer. Anticancer Res. 2014;34(1):493–501.
Murphy A, Chu JH, Xu M, Carey VJ, Lazarus S, Liu A, et al. Mapping of numerous disease-associated expression polymorphisms in primary peripheral blood CD4 + lymphocytes. Hum Mol Genet. 2010;19:4745–57.
Lamba JK, Fridley BL, Ghosh TM, Yu Q, Mehta G, Gupta P. Genetic variation in platinating agent and taxane pathway genes as predictors of outcome and toxicity in advanced non-small-cell lung Pharmacogenomics. 2014;15(12):1565–74.
Li Y, Huang XE, Jin GF, Shen HB, Xu L. Lack of any relationship between chemotherapy toxicity in non-small cell lung cancer cases and polymorphisms in XRCC1 codon 399 or XPD codon 751. Asian Pac J Cancer Prev. 2011;12(3):739–42.
Sullivan I, Salazar J, Majem M, Pallarés C, Del Río E, Páez D, et al. Pharmacogenetics of the DNA repair pathways in advanced non-small cell lung cancer patients treated with platinum-based chemotherapy. Cancer Lett. 2014;353(2):160–6.
Alli E, Bash-Babula J, Yang JM, Hait WN. Effect of stathmin on the sensitivity to antimicrotubule drugs in human breast cancer. Cancer Res. 2002;62:6864–9.
Balachandran R, Welsh MJ, Day BW. Altered levels and regulation of stathmin in paclitaxel-resistant ovarian cancer cells. Oncogene. 2003;22:8924–30.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare no conflicts of interest regarding this study.
Informed consent
“Informed consent was obtained from all individual participants included in the study”.
Additional information
T. Powrózek and R. Mlak contributed equally to this work.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Powrózek, T., Mlak, R., Krawczyk, P. et al. The relationship between polymorphisms of genes regulating DNA repair or cell division and the toxicity of platinum and vinorelbine chemotherapy in advanced NSCLC patients. Clin Transl Oncol 18, 125–131 (2016). https://doi.org/10.1007/s12094-015-1343-6
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12094-015-1343-6