Abstract
Background
The aim of this study was to demonstrate how tenofovir alafenamide (TAF) and other hepatitis B treatment drugs differentially impact lipid profiles in chronic hepatitis B patients.
Methods
We searched PubMed, Ovid MEDLINE, EMBASE, and the Cochrane Library to identify studies on the changes in cholesterol level in hepatitis B patients who underwent TAF therapy. The changes in lipid profiles (e.g., HDL-c, LDL-c, total cholesterol [TC], and triglyceride [TG]) were compared between the TAF treatment group and the baseline, other nucleoside analogs (NAs), and tenofovir disoproxil fumarate (TDF)-only treatment groups. In addition, risk factors for worsening cholesterol level when treated with TAF were examined.
Results
Twelve studies involving 6,127 patients were selected. After 6 months of TAF treatment, LDL-c, TC, and TG were increased by 5.69 mg/dL, 7.89 mg/dL, and 9.25 mg/dL, respectively, from the baseline level. In particular, with the treatment of TAF, levels of LDL, TC, and TG rose by 8.71 mg/dL, 18.34 mg/dL, and 13.68 mg/dL, respectively, showing a greater deterioration of cholesterol when the TAF treatment was implemented compared to other NAs (e.g., TDF or entecavir). When TAF was compared to TDF, LDL-c, TC, and TG worsened with a mean difference of 14.52 mg/dL, 23.72 mg/dL, and 14.25 mg/dL, respectively. As a result of a meta-regression analysis, risk factors for worsening lipid profiles were found to be treatment-experienced, previous diabetes, and hypertension.
Conclusions
TAF continues to worsen lipid profiles including LDL-c, TC, and TG after 6 months of use compared to the other NAs.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Chronic hepatitis B (CHB) has a global prevalence of 4.1% in all ages and there are approximately 316 million people infected with CHB [1]. Over a lifetime, 25% of patients with CHB develop hepatocellular carcinoma (HCC), and 4 out of 100,000 CHB patients die each year due to liver-related diseases [2,3,4,5]. To reduce the mortality of CHB, it is important to reduce liver inflammation and hepatitis B virus (HBV) activity, where antiviral treatment plays a key role [6].
One of the characteristics of HBV is HBV covalently closed circular DNA (cccDNA) making it difficult to cure CHB. Thus, a realistic goal will be implementing a functional cure that is seroconversion of hepatitis B surface antigen. Similarly, long-term administration of antiviral drugs is required for this reason [6]. Recently, as life expectancy has increased globally and effective hepatitis B vaccines have been developed, the prevalence of HBV in children is decreasing [7]. Therefore, the average age of patients with CHB increased, and the duration of antiviral treatment also increased. That is, while it was sufficient to focus the treatment only on hepatitis B itself a few decades ago, lately, more clinical attention should be paid to accompanying comorbidities. In fact, patients with CHB have a higher prevalence of non-liver comorbidities such as hypertension, diabetes, dyslipidemia, chronic kidney disease, and osteoporosis compared to normal populations [8]. Since antiviral drugs are likely to be taken for a very long time, it is important to select antiviral drugs considering these comorbidities [9].
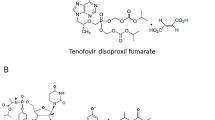
Tenofovir's first prodrug, tenofovir disoproxil fumarate (TDF) was approved by the Food and Drug Administration (FDA) for the treatment of human immunodeficiency virus type 1 (HIV-1) infection in 2001 and CHB in 2008. However, there have been concerns about the deterioration of renal function and bone density when using TDF for a long time [10]. Since tenofovir alafenamide (TAF) with improved bone and renal safety compared to TDF was approved by the FDA in 2015, it has been recommended as a first-line treatment and its use has been rapidly increasing recently. However, problems with the long-term use of TAF have been reported in some studies. In HIV-infected patients, switching from TDF-based regimens to TAF-based regimens, changes in lipid profile, weight gain, and cardiovascular risk were reported [11, 12]. In patients with CHB, it was also reported that there was an increase in low-density lipoprotein (LDL)-cholesterol and urinary glucose in the TAF group contrary to the TDF group [13]. On the other hand, there were also studies in which TAF did not show significant changes in the lipid profile compared to other antiviral agents [14].
Despite recommendations for the long-term use of TAF, studies on the side effects of TAF are still lacking. Accurate evaluation of the relationship between TAF and lipid profile is thought to provide useful clinical information for the selection of anti-viral agents for CHB patients with risk factors linked to cardiovascular comorbidities. Therefore, this study aims to investigate how the lipid profile changes with TAF treatment in CHB patients through a systematic literature review and meta-analysis.
Methods
The protocol for this review was registered with PROSPERO (International Prospective Register of Systematic Reviews, CRD42022373486) in advance. This systematic review and meta-analysis were performed according to the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) guidelines and the Meta-analysis of Observational Studies in Epidemiology (MOOSE) checklist.
Inclusion criteria, exclusion criteria, and study outcomes
Randomized controlled trials (RCT) were included. Prospective and retrospective cross-sectional or cohort studies that reported on the change in lipid profile in adult CHB patients (> 19 years) taking TAF were included. We included all studies without restrictions on medication duration, ethnicity, or country. The exclusion criteria were as follows: (i) case reports, (ii) case series of fewer than five patients, (iii) review articles, (iv) co-infection with HCV or HIV, and (v) studies that do not provide specific lipid profile values or provide values in ratios. The study's primary outcome was to determine the degree of changes in lipid profile following TAF treatment. Changes in lipid profile due to TAF were investigated under the following two clinical situations: (i) before and after taking TAF in the same patient, (ii) between TAF and non-TAF antiviral groups. The study's secondary outcome was to find out the risk factors of for changes in total cholesterol or LDL-cholesterol by TAF use. We first collected all factors related to changes in cholesterol in individual studies, and performed meta-regression analysis on items commonly mentioned in two or more studies.
Search strategy
The search terms included chronic hepatitis B-related index words, cholesterol-related index words, and TAF-related index words. We searched for synonymous terms and used them to develop search strategies. The keywords used in the Patient/Problem, Intervention, Comparison, and Outcome (PICO) model are shown in the Supplementary material. We searched Medline (PubMed), EMBASE, Cochrane Library databases, Web of Science, and KoreaMed using Medical Subject Headings terms to identify studies published in English between 1 January 2005 and 31 July 2022. The search strategies and results of each database search are shown in the methods section and Supplementary material. All search processes were conducted by a professional librarian (EAJ).
Study selection and data extraction
Two authors independently screened the titles and abstracts. Two reviewers (EGH and JJY) independently screened full-text articles for study relevance. Any discrepancy between the two reviewers was resolved by SKK after discussion. The two researchers also independently performed the risk of bias assessment for all included studies. The characteristics and results were extracted and recorded in standard form.
Methodological quality and risk of bias assessment
We used the Cochrane risk of bias tool [13] for randomized trials and the Risk of Bias Assessment tool for Non-randomised Studies (RoBANS) [15] for cohort studies to assess the risk of bias. The overall results are shown in the Supplementary material risk of bias section. Any discrepancy between the two authors (EGH and YSK) was resolved by discussion. Publication bias was assessed using funnel plots (Supplementary materials). Publication bias was evaluated only when there were three or more integrated studies.
Statistical analysis
We derived the pooled event rate as an outcome of a random-effects model, utilizing the following methods: i) the Freeman–Tukey variant of the arcsine square root transformed proportion to convert event rates to proportions, and ii) the Mantel–Haenszel method to compute the pooled event rate by back-transforming the weighted mean of transformed event rates. The comparison of lipid profile change in TAF and non-TAF antiviral groups was displayed as a mean difference for continuous variables and as a Freeman–Tukey variant for binary variables. Between-study variance estimation was calculated using the DerSimonian–Laird method. The comparative results were reported as mean differences and 95% confidence intervals. We evaluated inter-study heterogeneity using the I2 metric of inconsistency and the p value of the Cochran Q test. I2, the ratio of inter-study variance to the sum of intra-study and inter-study variance, ranges from 0 to 100%. Publication bias was evaluated by AS–Thompson’s test. Statistical analyses were performed using RevMan 5 (Cochrane Library) or the meta package in R (version 4.1.0; R Foundation for Statistical Computing, Vienna, Austria).
Results
Characteristics of included studies
Simultaneously screening the title and abstract, we identified 36 potentially relevant studies. Among them, 24 studies were excluded for the following reasons: studies without TAF prescription (n = 11), difficult to obtain the results of TAF alone group (n = 8), Studies in which cholesterol was not presented as an outcome (n = 3) and editorial or review article (n = 2). As a result, 12 studies were included in the meta-analysis (Fig. 1). Information on the enrolled patients is presented in Table 1.
As shown in Table 1, all 12 studies were conducted mostly in East Asia (n = 9), followed by Turkey and different continents. As for study design, the most common type was a retrospective cohort study (7 studies), followed by 3 prospective cohort studies and 2 RCTs. Nine studies compared the cholesterol levels of using TAF to other antiviral agents, and 3 studies reported results for the TAF-only group without a control group. There were 3 studies with treatment-naive patients, 5 studies with treatment-experienced patients, and the remaining 3 studies involved a mixed population. The treatment duration of TAF ranged from 6 months to 3 years.
Changes in lipid profile before and after using TAF
First, we analyzed the changes in lipid profiles before and after using TAF (Table 2). HDL-cholesterol increased slightly at 6 months (mean difference + 2.61 mg/dL, 95% CI 0.38–4.84) and at 12 months (mean difference + 2.49 mg/dL, 95% CI – 4.55–9.53) of treatment and decreased at 24 months (mean difference – 0.57 mg/dL, 95% CI – 7.98–6.84), but none of them were statistically significant. On the other hand, LDL-cholesterol, total cholesterol (TC), and triglyceride (TG) levels all significantly deteriorated after TAF treatment. The Δ in LDL-cholesterol level increased by 5.69 mg/dL (95% CI 1.82–9.55) compared to baseline at 6 months of treatment, and further increased to 7.10 mg/dL (95% CI 0.65–13.55) at the 12 months. The Δ in TC level significantly increased to 7.89 mg/dL (95% CI 4.92–10.86) at 6 months of treatment. The degree of TG elevation increased as the duration of TAF administration increased: Δ in TG; 9.25 mg/dL (95% CI 1.52–16.98) over 6 months, 13.80 mg/dL (95% CI 2.91–24.69) over 12 months, and 14.94 mg/dL (95% CI 5.87–24.00) over 24 months.
Comparing lipid profile changes between TAF and other antiviral agents (ETV or TDF)
Next, we examined how changes in lipid profiles differed when using TAF and other antiviral agents (Table 3). Other antiviral agents omitting TAF were entecavir (ETV) and TDF. TAF administration significantly increased all HDL-cholesterol, LDL-cholesterol, TC, and TG compared to when other antiviral agents were used. This aggravation of the lipid profile was observed from the 6th month of TAF administration and continued into the 24th month. Compared with other antiviral drugs, the LDL-cholesterol level was 8.71 mg/dL (95% CI 5.77–11.66) higher, the TC level was 18.34 mg/dL (95% CI 14.70–21.98) higher, and the TG level was 13.68 mg/dL (95% CI 7.63–19.73) higher in the TAF group at 6 months of treatment.
As a sub-analysis, we compared the lipid profile changes after TAF and TDF treatments (Table 4). Similar to the results in Table 3, deterioration of the overall lipid profile was observed in the TAF group. Compared with TDF, the LDL-cholesterol level was 14.52 mg/dL (95% CI 10.95–18.10) higher, the TC level was 23.72 mg/dL (95% CI 19.12–28.33) higher, and the TG level was 14.25 mg/dL (95% CI 12.64–15.86) higher in the TAF group.
Risk factors for cholesterol deterioration in patients using TAF
Finally, we performed a meta-regression analysis to find risk factors associated with cholesterol deterioration in patients with TAF. In our meta-analysis, 9 risk factors were taken into account: proportion of treatment-naïve, age, sex, body mass index, diabetes, hypertension, prior dyslipidemia, liver cirrhosis, and treatment duration (Table 5). First, the risk factors that significantly increased the TC level were treatment-experienced (β coefficient – 0.145, 95% CI – 0.183 to – 0.107, p < 0.001), male (β coefficient 0.348, 95% CI 0.199–0.497, p < 0.001), low body mass index (β coefficient – 3.236, 95% CI -6.371 to – 0.101, p = 0.043), previous diabetes (β coefficient 0.918, 95% CI 0.343–1.493, p = 0.001), hypertension (β coefficient 0.353, 95% CI 0.067–0.639, p = 0.015), and past history of dyslipidemia (β coefficient 0.661, 95% CI 0.364–0.958, p < 0.001). On the other hand, risk factors for increased LDL-cholesterol were treatment-experienced (β coefficient – 0.084, 95% CI – 0.132 to -0.036, p < 0.001), old age (β coefficient 0.449, 95% CI 0.122–0.775, p = 0.007), diabetes (β coefficient 1.338, 95% CI 0.752–1.924, p < 0.001), hypertension (β coefficient 0.365, 95% CI 0.111–0.618, p = 0.004), and pre-cirrhosis (β coefficient – 0.279, 95% CI – 0.476 to -0.082, p = 0.005).
Discussion
Through this meta-analysis, our study provided information about (i) changes in lipid profiles after TAF treatment, (ii) contrasting dyslipidemia conditions after the TAF and other antiviral treatments, and (iii) risk factors for TAF-induced cholesterol deterioration. As metabolic risk is associated with long-term mortality of CHB patients, we recognized the risk of dyslipidemia despite the clinical usefulness of TAF for renal and bone safety. Therefore, it is crucial to evaluate the risk of cholesterol deterioration when TAF is administered to patients with CHB.
Metabolic factors such as dyslipidemia can aggravate fibrosis and increase the risk of HCC in patients with CHB, so appropriate clinical attention is necessary [16, 17]. This is especially true, because the number of CHB patients with metabolic risks, for instance, fatty liver, is increasing. In line with this trend, the use of statin, a treatment for dyslipidemia, is gradually increasing in patients with CHB.
The effect of TAF on lipid profile has been reported mainly in HIV patients. TAF has been used since 2001 in patients with HIV, which is about 7 years earlier than it started being used in CHB patients. Based on the results of studies involving patients with HIV, the long-term effects of TAF use in patients with CHB B could be speculated in advance.
Similar to patients with HIV, TAF was excellent in terms of efficacy in HBV patients and had the advantage of improving bone and renal safety, but reports of aggravation of dyslipidemia still remained [18, 19]. When switching the HIV treatments from a TDF-containing regimen to a TAF-containing regimen, TC was reported to decrease by 36 mg/dL, and LDL-cholesterol by about 20 mg/dL [20]. This lipid profile deterioration was reported equally in both Eastern and Western countries irrespective of race and the deterioration persisted over the first 9–12 months after TAF administration [21]. Accordingly, in real-world practice, the lipid-lowering agent implementation increased by more than two times after switching from the TDF regimen to the TAF regimen (TDF 4.7%, TAF 11.9%) [22]. Since the lipid profile is closely related to CVD risk, there is also a result that the CVD risk increased from 20 to 31% after the TDF-to-TAF switch [23]. Among various lipid profiles, TAF was reported to increase TC or TG [21]; however, according to our study, it was related to the aggravation of all lipid profiles including LDL-cholesterol. In particular, the bigger probability of dyslipidemia exacerbation in patients with higher baseline TC or TG is consistent with our analysis [24].
While it has been uniformly reported that TAF aggravates dyslipidemia in HIV patients, the impact of TAF on the lipid profile in patients with CHB slightly differs across studies. So far, there are more reports that TAF deteriorates lipid profile than those that assert TAF is lipid-neutral. It has been reported that taking TAF for 6–12 months increased dyslipidemia in patients with CHB from 33 to 39%, and especially severe dyslipidemia from 1.4 to 5.8% [22]. In particular, compared to TDF, the risk of dyslipidemia using TAF is more emphasized. TDF had the effect of lowering TC by about 20 mg/dL or more in contrast to TAF [14] in agreement with our results. On that account, some suggested that TAF does not exacerbate lipid profile, but rather, TDF has a protective role [25]. In fact, the results of propensity score matching studies showed that the TAF treatment did not degenerate the lipid profile compared to non-infected control or inactive CHB, but worsened the lipid profile when compared to the TDF treatment [14]. In addition, the result that TDF was more advantageous in terms of lipid profile compared to ETV could be the basis for the lipid protective effect of TDF [26]. We observed the deterioration of the lipid profile in both situations, where we compared before and after the use of TAF and also compared TAF with other antiviral agents. Hence, it can be inferred that TAF alone worsens the lipid profile and that TDF, on the other hand, has a protective effect.
The mechanism of why TAF treatment has a less favorable effect on the lipid profile has not been precisely elucidated. From the results of the study, two hypotheses can be proposed. The first is that the use of TAF causes weight gain and affects the exacerbation of metabolic factors. In patients with HIV, a weight gain in the TAF regimen was observed immediately after switching to TAF according to research from both the East and West [27, 28]. Since weight gain can lead to exacerbation of dyslipidemia and metabolic disease, TAF use may be associated with exacerbation of dyslipidemia. However, only a few studies involving CHB patients report weight change, so it was difficult to analyze the link between the TAF treatment and weight gain. The second hypothesis is that TDF can improve the lipid profile, because it has a much higher plasma active ingredient tenofovir (TFV) [29, 30]. Moreover, in an in vitro study, TDF showed the effect of suppressing hepatocyte supernatant cholesterol by activating Peroxisome proliferator-activated receptor alpha (PPAR-α) [31]. Activation of PPAR-α-mediated signaling leads to activation of PPAR-α target genes, carnitine palmitoyltransferase 1, and CD36 [32]. Among them, hepatic CD36 uptakes oxidized low-density lipoproteins, high density lipoproteins, and free fatty acids, so the use of TDF may lead to lipid-protective results [33,34,35]. However, the mechanism has not yet been clearly identified in vivo or in humans, so further research is needed.
There is a lack of results on the long-term clinical impact of TAF on the worsening of the lipid profile which makes it hard to conclude whether it should be actively used. As it takes a long time to develop CVD, reports on the CVD risk associated with long-term use of TAF are also lacking. However, there is one study that showed the deterioration of the lipid profile after the TAF treatment was not observed in patients who were already taking a statin [36]. Statin use was recently shown to be associated with long-term prognoses, such as incidence of liver cirrhosis and HCC in patients with CHB [37,38,39]; thus, we can expect some articles about the TAF and statin combination in the future. Another way to find out the effect of long-term use of TAF on cholesterol level in patients with chronic hepatitis B is to refer to the results of long-term use of TAF in HIV patients. Previously, we mentioned that TAF use promotes dyslipidemia in HIV patients, but these were mostly short-term studies. In 2022, Gilbert et al. published data after using TAF for an average of 3.6 years in HIV patients [40]. In the long-term use group of TAF, total cholesterol, LDL-C, HDL-C, and TG changes tended to be rather low at − 2.5, − 0.1, − 0.6, and − 9 mmol/L, respectively [40]. Although there are still insufficient data on long-term use of TAF in hepatitis B patients, it is possible that a similar pattern will be observed in chronic hepatitis B patients.
Finally, in our study, we found that cholesterol deterioration by TAF was more severe in the group with risk factors. Although the risk factors for deterioration in total cholesterol and risk factors for deterioration in LDL-cholesterol were slightly different, the following three factors were common: treatment-experience, diabetes and hypertension. In the case of diabetes and hypertension, it is already well-known as a risk factor for dyslipidemia, and this applies equally to the group using TAF. On the other hand, the mechanism for why treatment-experienced patients' cholesterol is worsened by TAF is not yet known [41, 42]. Additional studies are needed in the long term, but careful clinical observation is needed when changing from TDF or entecavir to TAF.
This study has several limitations. First, there may have been selection bias, because only the studies that accurately presented cholesterol levels were selected. Second, since the follow-up period did not exceed 24 months, it was challenging to provide information on how long the change in lipid profile lasts after the TAF treatment. Third, many of the selected studies were conducted in East Asia. When initially searching for studies, we included all studies without restrictions on medication duration, ethnicity, or country. There have been TAF studies targeting Caucasian patients, but cholesterol was not presented as an outcome in most Western studies. Even when information on cholesterol was presented, it was often presented only with the proportion of patients whose cholesterol worsened, for example, with an LDL-C of 300 mg/dL or more, rather than with an exact value [43]. These studies were excluded, because they were difficult to integrate into meta-analysis, and as a result, most of the studies in which cholesterol levels were well-presented were East Asian studies, even though there was no restriction on race. It is possible that Western researchers have paid little clinical attention to cholesterol changes caused by TAF. Last, short-term studies within 3 years of taking TAF were mainly selected. As mentioned earlier, we did not place any restrictions on the duration of medication and did not intentionally exclude longer term studies. However, since TAF was approved by the U.S. Food and Drug Administration in November 2016 and marketed in earnest after 2017 or 2018, the number of studies on long-term use itself was small, so it seems that short-term studies were selected.
In conclusion, a significant deterioration in lipid profile, which may have clinical implications, was observed when TAF was administered for more than 6 months to CHB patients. Therefore, it seems that the lipid-negative effect of TAF should be fully considered when selecting antiviral agents to care for CHB patients at risk of CVD. In addition, clinicians should pay attention to lipid management and educate patients on appropriate lifestyle modification when using TAF.
Availability of data and materials
The data sets generated during and/or analysed during the current study are available from the corresponding author on reasonable request.
References
Lau G, Marcellin P, Peters M. Chronic hepatitis B: a global health problem requiring coherent worldwide treatment strategies. Hepatol Int. 2007;1:316–325
Ringelhan M, McKeating JA, Protzer U. Viral hepatitis and liver cancer. Philos Trans R Soc Lond B Biol Sci. 2017;372:20160274
Collaborators GBDHB. Global, regional, and national burden of hepatitis B, 1990–2019: a systematic analysis for the global burden of disease study 2019. Lancet Gastroenterol Hepatol. 2022;7:796–829
2022 KLCA-NCC Korea practice guidelines for the management of hepatocellular carcinoma. J Korean Liver Cancer Stud Group 2022;0.
Renne SL, Tommaso LD. A clinical and pathological update on hepatocellular carcinoma. J Liver Cancer. 2022;22:14–22
Korean Association for the Study of the L. KASL clinical practice guidelines for management of chronic hepatitis B. Clin Mol Hepatol. 2022;28:276–331
Meireles LC, Marinho RT, Van Damme P. Three decades of hepatitis B control with vaccination. World J Hepatol. 2015;7:2127–2132
Oh H, Jun DW, Lee IH, Ahn HJ, Kim BO, Jung S, et al. Increasing comorbidities in a South Korea insured population-based cohort of patients with chronic hepatitis B. Aliment Pharmacol Ther. 2020;52:371–381
Terrault NA, Lok ASF, McMahon BJ, Chang KM, Hwang JP, Jonas MM, et al. Update on prevention, diagnosis, and treatment of chronic hepatitis B: AASLD 2018 hepatitis B guidance. Hepatology. 2018;67:1560–1599
Lee BT, Chang M, Lim C, Bae HS, Fong TL. Bone and renal safety profile at 72 weeks after switching to tenofovir alafenamide in chronic hepatitis B patients. JGH Open. 2021;5:258–263
Lagoutte-Renosi J, Flammang M, Chirouze C, Beck-Wirth G, Bozon F, Brunel AS, et al. Real-life impact on lipid profile of a switch from tenofovir disoproxil fumarate to tenofovir alafenamide in HIV-infected patients. Curr HIV Res. 2021;19:84–89
Plum PE, Maes N, Sauvage AS, Frippiat F, Meuris C, Uurlings F, et al. Impact of switch from tenofovir disoproxil fumarate-based regimens to tenofovir alafenamide-based regimens on lipid profile, weight gain and cardiovascular risk score in people living with HIV. BMC Infect Dis. 2021;21:910
Buti M, Gane E, Seto WK, Chan HL, Chuang WL, Stepanova T, et al. Tenofovir alafenamide versus tenofovir disoproxil fumarate for the treatment of patients with HBeAg-negative chronic hepatitis B virus infection: a randomised, double-blind, phase 3, non-inferiority trial. Lancet Gastroenterol Hepatol. 2016;1:196–206
Jeong J, Shin JW, Jung SW, Park EJ, Park NH. Tenofovir alafenamide treatment may not worsen the lipid profile of chronic hepatitis B patients: A propensity score-matched analysis. Clin Mol Hepatol. 2022;28:254–264
Kim SY, Park JE, Lee YJ, Seo HJ, Sheen SS, Hahn S, et al. Testing a tool for assessing the risk of bias for nonrandomized studies showed moderate reliability and promising validity. J Clin Epidemiol. 2013;66:408–414
Cai S, Ou Z, Liu D, Liu L, Liu Y, Wu X, et al. Risk factors associated with liver steatosis and fibrosis in chronic hepatitis B patient with component of metabolic syndrome. United European Gastroenterol J. 2018;6:558–566
Cho Y, Cho EJ, Yoo JJ, Chang Y, Chung GE, Jeong SM, et al. Association between lipid profiles and the incidence of hepatocellular carcinoma: a nationwide population-based study. Cancers (Basel). 2021;13:1599
Wang H, Lu X, Yang X, Xu N. The efficacy and safety of tenofovir alafenamide versus tenofovir disoproxil fumarate in antiretroviral regimens for HIV-1 therapy: meta-analysis. Medicine (Baltimore). 2016;95: e5146
Pilkington V, Hughes SL, Pepperrell T, McCann K, Gotham D, Pozniak AL, et al. Tenofovir alafenamide vs tenofovir disoproxil fumarate: an updated meta-analysis of 14 894 patients across 14 trials. AIDS. 2020;34:2259–2268
Cid-Silva P, Fernandez-Bargiela N, Margusino-Framinan L, Balboa-Barreiro V, Mena-De-Cea A, Lopez-Calvo S, et al. Treatment with tenofovir alafenamide fumarate worsens the lipid profile of HIV-infected patients versus treatment with tenofovir disoproxil fumarate, each coformulated with elvitegravir, cobicistat, and emtricitabine. Basic Clin Pharmacol Toxicol. 2019;124:479–490
Mallon PWG, Brunet L, Fusco JS, Prajapati G, Beyer A, Fusco GP, et al. Lipid changes after switch from TDF to TAF in the OPERA cohort: LDL cholesterol and triglycerides. Open Forum Infect Dis. 2022;9:ofab621
Suzuki K, Suda G, Yamamoto Y, Abiko S, Kinoshita K, Miyamoto S, et al. Effect of switching from tenofovir disoproxil fumarate to tenofovir alafenamide on lipid profiles in patients with hepatitis B. PLoS ONE. 2022;17: e0261760
Brunet L, Mallon P, Fusco JS, Wohlfeiler MB, Prajapati G, Beyer A, et al. Switch from tenofovir disoproxil fumarate to tenofovir alafenamide in people living with HIV: lipid changes and statin underutilization. Clin Drug Investig. 2021;41:955–965
Zhang Y, Li Z, Luo Q, Xu W, Wang L, Zhu S, et al. Changes in blood lipids in patients with chronic hepatitis B after 48 weeks of tenofovir alafenamide treatment: A prospective real-world clinical study. Antivir Ther. 2022;27:13596535221082400
Lin HY, Tseng TC. Dyslipidemia in chronic hepatitis B patients on tenofovir alafenamide: facts and puzzles. Clin Mol Hepatol. 2022;28:181–182
Shaheen AA, AlMattooq M, Yazdanfar S, Burak KW, Swain MG, Congly SE, et al. Tenofovir disoproxil fumarate significantly decreases serum lipoprotein levels compared with entecavir nucleos(t)ide analogue therapy in chronic hepatitis B carriers. Aliment Pharmacol Ther. 2017;46:599–604
Mallon PW, Brunet L, Hsu RK, Fusco JS, Mounzer KC, Prajapati G, et al. Weight gain before and after switch from TDF to TAF in a U.S. cohort study. J Int AIDS Soc. 2021;24: e25702
Kuo PH, Sun HY, Chuang YC, Wu PY, Liu WC, Hung CC. Weight gain and dyslipidemia among virally suppressed HIV-positive patients switching to co-formulated elvitegravir/cobicistat/emtricitabine/tenofovir alafenamide. Int J Infect Dis. 2020;92:71–77
Lampertico P, Buti M, Fung S, Ahn SH, Chuang WL, Tak WY, et al. Switching from tenofovir disoproxil fumarate to tenofovir alafenamide in virologically suppressed patients with chronic hepatitis B: a randomised, double-blind, phase 3, multicentre non-inferiority study. Lancet Gastroenterol Hepatol. 2020;5:441–453
Mills A, Arribas JR, Andrade-Villanueva J, DiPerri G, Van Lunzen J, Koenig E, et al. Switching from tenofovir disoproxil fumarate to tenofovir alafenamide in antiretroviral regimens for virologically suppressed adults with HIV-1 infection: a randomised, active-controlled, multicentre, open-label, phase 3, non-inferiority study. Lancet Infect Dis. 2016;16:43–52
Suzuki K, Suda G, Yamamoto Y, Furuya K, Baba M, Nakamura A, et al. Tenofovir-disoproxil-fumarate modulates lipid metabolism via hepatic CD36/PPAR-alpha activation in hepatitis B virus infection. J Gastroenterol. 2021;56:168–180
Silverstein RL, Febbraio M. CD36, a scavenger receptor involved in immunity, metabolism, angiogenesis, and behavior. Sci Signal. 2009;2:re3
Koonen DP, Jacobs RL, Febbraio M, Young ME, Soltys CL, Ong H, et al. Increased hepatic CD36 expression contributes to dyslipidemia associated with diet-induced obesity. Diabetes. 2007;56:2863–2871
Luangrath V, Brodeur MR, Rhainds D, Brissette L. Mouse CD36 has opposite effects on LDL and oxidized LDL metabolism in vivo. Arterioscler Thromb Vasc Biol. 2008;28:1290–1295
Brundert M, Heeren J, Merkel M, Carambia A, Herkel J, Groitl P, et al. Scavenger receptor CD36 mediates uptake of high density lipoproteins in mice and by cultured cells. J Lipid Res. 2011;52:745–758
Lacey A, Savinelli S, Barco EA, Macken A, Cotter AG, Sheehan G, et al. Investigating the effect of antiretroviral switch to tenofovir alafenamide on lipid profiles in people living with HIV. AIDS. 2020;34:1161–1170
Wang Y, Xiong J, Niu M, Chen X, Gao L, Wu Q, et al. Statins and the risk of cirrhosis in hepatitis B or C patients: a systematic review and dose-response meta-analysis of observational studies. Oncotarget. 2017;8:59666–59676
Goh MJ, Sinn DH, Kim S, Woo SY, Cho H, Kang W, et al. Statin use and the risk of hepatocellular carcinoma in patients with chronic hepatitis B. Hepatology. 2020;71:2023–2032
Li X, Sheng L, Liu L, Hu Y, Chen Y, Lou L. Statin and the risk of hepatocellular carcinoma in patients with hepatitis B virus or hepatitis C virus infection: a meta-analysis. BMC Gastroenterol. 2020;20:98
Gilbert JM, Vest K, Kish TD. Long-term evaluation of changes in kidney function after switching from tenofovir disoproxil fumarate to tenofovir alafenamide in patients living with HIV. Pharmacy (Basel). 2022;10:164
van den Berg E, Kloppenborg RP, Kessels RP, Kappelle LJ, Biessels GJ. Type 2 diabetes mellitus, hypertension, dyslipidemia and obesity: a systematic comparison of their impact on cognition. Biochim Biophys Acta. 2009;1792:470–481
Halpern A, Mancini MC, Magalhaes ME, Fisberg M, Radominski R, Bertolami MC, et al. Metabolic syndrome, dyslipidemia, hypertension and type 2 diabetes in youth: from diagnosis to treatment. Diabetol Metab Syndr. 2010;2:55
Chan HL, Fung S, Seto WK, Chuang WL, Chen CY, Kim HJ, et al. Tenofovir alafenamide versus tenofovir disoproxil fumarate for the treatment of HBeAg-positive chronic hepatitis B virus infection: a randomised, double-blind, phase 3, non-inferiority trial. Lancet Gastroenterol Hepatol. 2016;1:185–195
Lim J, Choi WM, Shim JH, Lee D, Kim KM, Lim YS, et al. Efficacy and safety of tenofovir alafenamide versus tenofovir disoproxil fumarate in treatment-naïve chronic hepatitis B. Liver Int. 2022;42:1517–1527
Li J, Hu C, Chen Y, Zhang R, Fu S, Zhou M, et al. Short-term and long-term safety and efficacy of tenofovir alafenamide, tenofovir disoproxil fumarate and entecavir treatment of acute-on-chronic liver failure associated with hepatitis B. BMC Infect Dis. 2021;21:567
Hosaka T, Suzuki F, Kobayashi M, Fujiyama S, Kawamura Y, Sezaki H, et al. Renal safety and biochemical changes for 2 years after switching to tenofovir alafenamide from long-term other nucleotide analog treatment in patients with chronic hepatitis B. Hepatol Res. 2022;52:153–164
Akdemir Kalkan I, Karasahin O, Sarigul F, Altunisik Toplu S, Aladag M, Akgul F, et al. Comparison of tenofovir alafenamide and entecavir therapy in patients with chronic hepatitis B initially treated with tenofovir disoproxil. Retrosp Obs Surv. 2021;21: e118721
Karasahin O, Kalkan IA, Dal T, Toplu SA, Harputoğlu M, Mete AO, et al. Real-life data for tenofovir alafenamide fumarate treatment of hepatitis B: the pythagoras cohort. Hepat Mon. 2021;21:1–9
Ogawa E, Nakamuta M, Koyanagi T, Ooho A, Furusyo N, Kajiwara E, et al. Switching to tenofovir alafenamide for nucleos(t)ide analogue-experienced patients with chronic hepatitis B: week 144 results from a real-world, multi-centre cohort study. Aliment Pharmacol Ther. 2022;56:713–722
Jeong S, Shin HP, Kim HI. Real-world single-center comparison of the safety and efficacy of entecavir, tenofovir disoproxil fumarate, and tenofovir alafenamide in patients with chronic hepatitis B. Intervirology. 2022;65:94–103
Byun KS, Choi J, Kim JH, Lee YS, Lee HC, Kim YJ, et al. Tenofovir alafenamide for drug-resistant hepatitis B: A randomized trial for switching from tenofovir disoproxil fumarate. Clin Gastroenterol Hepatol. 2022;20:427-437.e425
Agarwal K, Brunetto M, Seto WK, Lim YS, Fung S, Marcellin P, et al. weeks treatment of tenofovir alafenamide vs tenofovir disoproxil fumarate for hepatitis B virus infection. J Hepatol. 2018;68:672–681
Acknowledgements
We would like to thank Jae-Young Kim in Research Factory Inc. (rfactory.kr) for consulting the statistical analysis
Funding
This work was supported by the Soonchunhyang University Research Fund.
Author information
Authors and Affiliations
Contributions
Study concept and design: J-JY; provision of study materials or patients: J-JY, E-AJ; collection and assembly of data: SGK, YSK; data analysis and interpretation: EGH, J-JY; manuscript writing: EGH; final approval of manuscript: all authors.
Corresponding author
Ethics declarations
Conflict of interest
The authors (Eui Gwon Hwang, Eun-Ae Jung, Jeong-Ju Yoo, Sang Gyune Kim, Young Seok Kim) have no relevant financial or non-financial interests to disclose.
Ethical approval and consent to participate
Ethics approval was waived from the Institutional Review Board and our study conformed to the ethical guidelines of the World Medical Association Declaration of Helsinki.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Hwang, E.G., Jung, EA., Yoo, JJ. et al. Risk of dyslipidemia in chronic hepatitis B patients taking tenofovir alafenamide: a systematic review and meta-analysis. Hepatol Int 17, 860–869 (2023). https://doi.org/10.1007/s12072-023-10528-7
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12072-023-10528-7