Abstract
Chronic hepatitis B virus infection, a major cause of end-stage liver disease and hepatocellular carcinoma, is a worldwide health concern. While the past two decades have brought major advances in the availability of treatments to help delay or prevent these outcomes, treatment of chronic hepatitis B remains a serious challenge, not least due to the ability of the virus to remain in hepatocyte nuclei as a source of potential reactivation—hence the term chronic hepatitis B infection. This article reviews the current treatments available and suggests a framework for a rational approach to managing the disease.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Infection with hepatitis B virus (HBV) can result in end-stage liver disease and hepatocellular carcinoma, accounting for up to 1 million deaths per year [1]. Due to the ability of the HBV genome to be maintained in the nuclei of infected hepatocytes, infected patients have chronic hepatitis B (CHB) and are at life-long risk of disease reactivation. Thus patients should be regularly monitored to detect active disease as a number of treatment options for patients are available. Indeed, understanding the dynamic nature of chronic HBV infection is crucial in the management of HBV carriers and highlights the need for long-term monitoring [2]. However, many patients with CHB do not receive routine monitoring, treatment or follow-up. There are several possible reasons for this, including a lack of knowledge about the disease and the need for treatment, uncertainty about how to treat, or insufficient appreciation of the severity of the disease and its outcomes, both on the part of healthcare professionals and patients. In addition, in many parts of the world where HBV is endemic, there is lack of available resources to diagnose and adequately treat. The frequently protracted time course of the disease does not encourage the primary care physician to monitor the apparently ‘healthy’ asymptomatic carrier, or to seek referral to a liver specialist. Several evidence-based treatment guidelines have been devised for distinct geographical regions [3–6]. However, despite geographical differences in prevalence of infecting HBV genotype, the treatment strategy remains essentially the same.
The aim of this article is to briefly review the global burden of disease, the treatments and treatment guidelines currently available and, finally, to provide an evidence-based patient management rationale. It is our goal to provide guidance, applicable to all clinicians, to help them select the most appropriate course of patient management for individual patients. As physicians we try to provide patients with the best possible treatment strategy, given available resources, and educate our patients about these while taking account of their individual needs and preferences.
Burden of disease
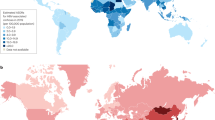
While prophylactic vaccination has significantly reduced the incidence of de novo HBV infections among populations where it has been introduced [7], CHB remains a serious global public health concern affecting 350 million people [8, 9]. Although the minority (only 15–40%) of infected individuals go on to develop cirrhosis, liver failure and hepatocellular carcinoma (HCC), this results in an estimated 0.5–1.2 million fatalities per year, ranking CHB as the tenth leading cause of death worldwide [8, 9]. The health hazards associated with this large pool of chronically infected individuals is reflected by the increased rates of HCC monitored in the USA (almost doubling during a 15 year period) despite the declining incidence in HBV infection [10]. A recent observational study of Taiwanese patients over 30 years of age, has identified elevated serum HBV DNA levels of ≥10,000 copies/ml (∼2000 IU/ml) as a strong risk predictor of HCC development independent of HBV ‘e’ antigen (HBeAg) status, serum alanine aminotransferase (ALT) level, and liver cirrhosis [11]. Perhaps unsurprisingly then, HCC incidence has increased throughout the world, ranking as the fifth most frequent cancer, causing 300,000–500,000 deaths per annum [12]. Global mortality estimates for 2002 suggested that 328,000 liver cancer deaths were due to CHB, approximately double the number caused by chronic hepatitis C [13]. In addition, a study investigating all cause mortality, excluding liver disease related death, suggested that age-adjusted death rates are 3–3.6 times higher in those carrying the HBV surface antigen (HBsAg) compared with uninfected individuals [14].
In endemic area, HBV is usually transmitted vertically to newborns (e.g. the Pacific and Asia) or horizontally in early childhood (e.g. sub-Saharan Africa), whereas in those areas of relatively low-occurrence (e.g. Western Europe and USA) horizontal infection is the norm among young adults due to sexual contact and needle sharing amongst injection drug-users [15]. Lack of universal vaccine coverage among endemically infected populations and increasing levels of migration into low-incidence countries provide ample opportunity for continued HBV spread. Serious consequences of CHB are noted in one third of those who acquire infection in early life. In contrast, patients who contracted the disease later in life are less likely to suffer serious sequelae (only ∼20% develop cirrhosis or HCC) since their disease has had a relatively shorter time to progress. Despite geographic differences in genotypes and in the prevalence of HBeAg-positive and -negative disease [16–20] (Table 1), clinicians worldwide are now more likely to encounter patients of all genotypes and both HBeAg-positive and -negative disease during their practice as a result of population migration, and consequently need to know how to treat all types of patient appropriately.
Treatment goals and treatment options
The ultimate goal of treatment for CHB is improvement in long-term survival with decreased progression of liver disease to cirrhosis and liver failure or HCC. This goal has many steps, including suppression of viral replication, decrease of HBV DNA, loss of HBeAg, acquisition of anti-HBe and ultimately loss of HBsAg and acquisition of anti-HBs. Data from multiple studies have shown that success in all of the aforementioned steps has led to better survival and decrease in HCC incidence. However, viral eradication is unlikely due the pool of cccDNA residing in the nuclei of infected hepatocytes, so remission of disease is a reasonable goal. Immunological control of CHB (through the development of anti-HBs antibodies, i.e. seroconversion) is a similar state to that achieved in those who effectively control HBV replication following acute infection and do not progress to the chronic stage (so called past infection). Loss of HBsAg is associated with improved survival [21]. In patients with HBeAg-positive CHB, immunological control is also indicated by HBeAg seroconversion (ie. loss of HBeAg from serum and development of anti-HBe antibodies). HBeAg seroconversion is indicative of a durable clinical response and is associated with improved clinical outcome [22, 23]. As a result, HBeAg seroconversion, or HBeAg loss, is often used as a marker of treatment response in clinical trials. Sustained reduction in HBV viral load, with corresponding ALT normalisation (≤30 IU/l for men and <20 IU/l for women) and histological stabilisation or improvement, are considered important treatment objectives in HBeAg-negative CHB in which HBeAg loss cannot be used as a marker. Currently there are up to seven approved agents for the treatment of CHB, and these fall into two categories: (i) immunomodulatory therapies, i.e. conventional interferon (IFN) alfa and pegylated interferon (PEG-IFN) alfa-2a (ii) antiviral agents (nucleos(t)ide analogues): lamivudine, adefovir, entecavir, telbivudine and clevudine (in Korea).
Immunomodulatory therapy
Interferon has both antiviral and immunomodulatory properties. The aim of treatment with IFN is to induce a sustained response to treatment following a finite period of therapy. Conventional IFN has been largely superseded by PEG-IFN due to its improved administration schedule (once weekly versus thrice weekly injection).
Conventional interferon
In patients with HBeAg-positive CHB, a meta-analysis of 15 trials of 12–24 weeks IFN treatment resulted in an HBeAg seroconversion rate of 18% and virological response with reduction in HBV DNA to ≤100,000 copies/ml (∼20,000 IU/ml) in 37% of patients compared with 17% of those untreated [6, 24]. Rates of HBsAg loss have been reported in 5–10% of European patients during 1 year of treatment, increasing to 11–25% among sustained responders over a 5-year follow-up period [20, 23, 25, 26]. Long-term follow-up of a group of HBeAg-positive patients who responded to IFN suggested that the remissions induced are of long duration and were followed in most cases by loss of HBsAg and lack of evidence of HBV replication [27]. Until recently, most data on the efficacy of IFN had come from European studies, however, a recent study of Taiwanese patients treated with a finite course of IFN therapy and followed up for a median of 6.8 years showed that, compared to untreated controls with persistent HBeAg positivity, HBeAg seroconversion in untreated and IFN-treated patients resulted in a significantly lower incidence of liver cirrhosis and cancer [28]. This further supports the use of HBeAg seroconversion as a measure of treatment efficacy for HBeAg-positive CHB. As with HBeAg-positive CHB, sustained response to IFN therapy in patients with HBeAg-negative CHB is associated with improved clinical outcome and increasing likelihood of HBsAg loss. While IFN treatment in patients with HBeAg-negative CHB appears to be less durable than that in HBeAg-positive patients, with relapse rates of 40% [29], improved response has been observed in patients treated for >1 year.
Pegylated interferon
Due to its improved pharmacokinetic profile and results of large multicentre trials [30, 31], conventional IFN has recently been dropped from treatment recommendations for CHB management in the USA, in favour of the pegylated form [6]. A trial of PEG-IFN showed benefit over conventional IFN in patients with HBeAg-positive CHB following treatment for 24 weeks [32]. Trials investigated the efficacy of PEG-IFN, with and without the addition of lamivudine, in comparison with lamivudine. In patients with HBeAg-positive disease, a 48-week course of PEG-IFN treatment produced significantly greater rates of seroconversion, suppression of HBV DNA replication and ALT normalisation compared with lamivudine, as measured 24 weeks post-treatment. Despite providing greater on-treatment HBV DNA suppression, the addition of lamivudine to PEG-IFN did not produce any advantage in term of response rate 24 weeks post-treatment compared with PEG-IFN monotherapy. A total of 8 patients in each of the two PEG-IFN treatment arms achieved HBsAg seroconversion 6 months post-treatment cessation, an HBsAg seroconversion rate of 3% vs. 0% for those treated with lamivudine alone. Longer-term follow-up of 172 patients treated with PEG-IFN monotherapy in the original study, of whom 69 (40%) had HBeAg-seroconversion 6 months post-treatment, revealed that the response was sustained in 91% of this group, and that an additional 15% of patients developed a late serological response 6–12 months after ending therapy [33]. Multivariate analysis indicated that response to PEG-IFN was associated with higher baseline ALT and lower HBV-DNA and HBeAg level, but not with gender, age, race or body weight. Genotype A infection was associated with a better response (52%) compared to genotypes B (30%), C (31%) and D (22%). Long-term sustained HBeAg-seroconversion was associated with substantial HBV DNA reduction and ALT normalisation, with 72% of patients having HBV DNA levels <10,000 copies/ml (∼2,000 IU/ml) and 82% having normal ALT 1 year post-treatment. Studies of pegylated interferon alfa-2b with or without lamivudine for 1 year found that 35% of subjects had lost HBeAg at follow up; that there was no benefit from the addition of lamivudine; and that genotype A subjects had a better response [34].
In HBeAg-negative CHB, PEG-IFN was superior to lamivudine monotherapy with statistically significantly higher post-treatment response rates, both as monotherapy and when used in combination with lamivudine in treatment naïve patients [30]. As with treatment of HBeAg-positive disease, the addition of lamivudine to PEG-IFN did not improve response rate 24 weeks post-treatment compared with monotherapy. Longer-term follow-up of patients originally treated with PEG-IFN monotherapy (n = 116) and with the combination with lamivudine (n = 114) has demonstrated that the responses are sustained up to 2 years post-treatment in approximately two-thirds of patients who had an initial response [35]. Treatment of HBeAg-negative patients with PEG-IFN also induced HBsAg seroconversion, which was maintained over 2 years of follow-up.
Nucleos(t)ide analogues: lamivudine, adefovir, telbivudine, entecavir and clevudine
The nucleos(t)ide analogues lamivudine and adefovir, originally developed for treatment of HIV, display potent antiviral activity against HBV replication. Entecavir, telbivudine and clevudine, the most recently licensed antivirals for HBV, have no anti-HIV activity. All five agents have similar modes of action, functioning as obligate HBV DNA chain terminators and are administered orally with few or no side effects, thus promoting good patient compliance. However, they also have their limitations. They usually require longer-term therapy because of their antiviral mode of action; once stopped, viral rebound is common. In addition, long-term use is associated with the development of viral strains resistant to their action, which increases over time. For lamivudine this reaches approximately 70% following 5 years of uninterrupted treatment [36–41]. Viral resistance may not be benign, with concomitant rebound in HBV DNA and ALT levels toward pre-treatment values; in some cases severe ALT flares and rapid decompensation have been observed [37, 42]. Because of these limitations, lamivudine is not recommended as first-line therapy CHB in recently published US treatment guidelines [6].
Development of resistance to adefovir is less pronounced and slower to emerge than for lamivudine, reaching levels of 18% and 29% by 4 and 5 years of treatment, respectively, in patients with HBeAg-negative CHB [43, 44]. Treatment of patients with HBeAg-negative CHB with adefovir induced ALT normalisation in 72% of patients and HBV DNA suppression to <1,000 copies/ml (∼200 IU/ml) in 51% compared with 29% and 0% of placebo-treated controls at 1 year [45]. At 2 and 5 years, HBV DNA suppression was 71% and 67%, with ALT normalisation of 73% and 69%, respectively [43, 46]. Liver histology improved in 75–80% after 5 years of adefovir therapy [46].
Entecavir has been demonstrated to be superior to lamivudine in suppressing HBV DNA and improving liver histology for both HBeAg-positive and -negative forms of the disease in treatment-naïve patients [47, 48] but showed no difference in rates of HBeAg or HBsAg loss or seroconversion when compared with lamivudine treatment for the same period [47]. Telbivudine also induces greater suppression of HBV DNA than lamivudine in patients with both HBeAg-positive and -negative disease, with 60% and 88% of individuals experiencing HBV DNA loss to undetectable levels after 2 years, compared with 40% and 71% of those treated with lamivudine, respectively. Telbivudine treatment was also associated with fewer flares and lower rates of resistance (2–3% vs. 7–8%) compared with lamivudine but demonstrated no significant difference in HBeAg loss or seroconversion [49, 50]. Telbivudine has also been demonstrated to be superior to adefovir in suppressing HBV DNA but again no difference in the rates of HBeAg loss were detected [50, 51]. Clevudine is a new nucleoside analogue, so far approved for use only in Korea. There is little information on efficacy beyond short-term treatment [52, 53]. The emergence of resistance to entecavir has not been noted in patients receiving up to 96 weeks of continuous therapy with entecavir in NA-naïve patients [54]. Pre-existing lamivudine mutations appear to be necessary for clinical resistance to entecavir to develop [55], developing in 9% of patients after 96 weeks [54].
Higher baseline and on-therapy HBV DNA levels are risk factors for the development of resistance nucleos(t)ide analogues. When following an antiviral treatment strategy, consideration of combination or add-on of further nucleos(t)ide analogues may be considered but is associated with additional costs. Combination therapy with two nucleos(t)ide analogue drugs has been suggested and has been shown to decrease the risk of resistance [56]. However, there was no difference in control of HBV whether sequential or combination therapy was used, although viral resistance was lower with combination therapy. In addition, there is a higher incidence of viral resistance in patients with Lam-resistant HBV strains who received ADV, entecavir or telbivudine monotherapy [57–59]. Current data suggest that, although immunological control can be achieved in some patients following treatment with nucleos(t)ide analogues, in many patients the host is unable to mount an effective immune response despite adequate suppression of viral replication. Interferon, which has immunomodulatory as well as antiviral activity, appears to achieve this more effectively, although only in one third of subjects and the mechanism is, as yet, not fully elucidated.
Current treatment guidelines
Currently available guidelines provide valuable insights into each type of therapy but they generally leave open the choice of antiviral treatment with nucleos(t)ide analogues or immunomodulatory therapy with conventional IFN or PEG-IFN as preferred first-line treatment. Choices of therapy depend on chance of response, severity of disease and patients and provider preference.
Treatment recommendations
European guidelines recommend IFN as an initial first-line treatment, with lamivudine or adefovir only if IFN is ineffective, poorly tolerated or contraindicated [3]. All three treatments are recommended as appropriate by the AASLD [4] and APASL [5], whereas more recently, lamivudine has been dropped in favour of entecavir and PEG-IFN has been specifically recommended in an algorithm strictly designed for treatment of patients in the USA [6]. In addition, elevated ALT accompanied by HBV DNA >10,000 copies/ml or 2,000 IU/ml (rather than >100,000 copies/ml or >20,000 IU/ml) have also recently been recommended for treatment in patients with HBeAg-negative disease [6]. The latest AASLD guidelines now include telbivudine as a treatment option but due to the high rate of resistance development and cross-reactivity with resistance mutations conferring resistance to lamivudine, this drug must be used with caution as monotherapy in the treatment of CHB [4].
Efficacy in various categories
Duration of treatment
For the treatment of patients with HBeAg-positive CHB, IFN treatment was recommended for 4–6 months [3, 5], but more recently therapy for up to 1 year has been suggested, as has the preferred use of PEG-IFN [4, 6]. Nucleos(t)ide analogues should be given for at least 1 year, and continued for an additional 6–12 months following HBeAg seroconversion [3–5], or until HBV DNA reaches stable undetectable levels [6].
The optimal duration of treatment in patients with HBeAg-negative CHB remains unclear, but is generally regarded as being longer than that for HBeAg-positive CHB. The decision to stop treatment should be based on a stable clinical response and the severity of underlying liver disease. Treatment with nucleos(t)ide analogues may be lifelong, whereas the use of conventional IFN or PEG-IFN is for 1 year [4–6].
To summarise, current treatment guidelines were not devised with the intention of providing hard and fast rules to assist clinicians in deciding which treatment strategy may be most appropriate for an individual patient. Indeed, in a number of patients either treatment approach may be appropriate, and the final decision is made by patient and physician preference.
Towards a unified treatment management strategy
Much evidence has accrued for the efficacy of continuous nucleot(s)ide therapy, providing highly effective HBV suppression, ALT normalisation and improvement in liver histology. On the other hand, HBsAg seroconversion is rarely observed and, compared to IFN-based treatment, sustained, off-therapy response is less common, especially in HBeAg-negative CHB where cessation is more often followed by relapse [31, 43].
Clearly we now have a number of agents at our disposal to treat CHB, and newer nucleos(t)ide analogues are in development [52, 53]. However, we need to use these agents wisely and in patients where they are most likely to bring benefit. Both immunomodulatory and nucleos(t)ide analogues agents have their pros and cons (Table 2) and both find application in patient management—but the treatment strategy chosen must be one that considers all relevant factors for each individual patient and balances the potential benefits versus risks. Such factors include: patient age, severity of liver disease, other co-morbidities if relevant, preference and anticipated treatment duration. While nucleos(t)ide analogues are the only available treatment for a patient with decompensated cirrhosis (for whom IFN-based therapy would be contraindicated), a course of PEG-IFN may be the most appropriate first-line treatment strategy in a young patient in order to give them a one in three overall chance of sustained response. If seroconversion is not achieved with PEG-IFN, longer-term treatment with nucleos(t)ide analogues could be a fall back strategy. Patients who opt for a finite course of PEG-IFN must be made aware of the side effects they are likely to encounter while those choosing nucleos(t)ide analogue therapy must be made aware of the necessity for longer-term treatment as well as the risk of resistance development and its consequences.
Expense is a major consideration when selecting treatments and it is an unfortunate fact that not all patients have access to equivalent treatments. In many Asian and sub Saharan countries, despite the high rate of resistance development, lamivudine is frequently prescribed as a result of the cost savings compared to other nucleos(t)ide analogues or IFN-based therapy. However, the higher initial cost of IFN-based treatments [6] may be considerably offset against the sustained off-treatment responses that have been observed, when compared with continuous on-treatment therapy with nucleos(t)ide analogues, wherein costs of potential combination therapy regimens may approach that of IFNs. While a recent analysis suggested that, entecavir may be the most cost-effective strategy for HBeAg-positive patients over a 5-year perspective, its higher cost being offset by decreased progression of disease, long-term efficacy and low-resistance rate remain unproven [59]. Moreover, projection over a longer time span improved the cost-effectiveness of an IFN regimen, suggesting potential cost benefit particularly in younger individuals [27]. The growing number of antiviral drugs both approved for use and in development may allow for effective management of CHB with either ‘add-on therapy’ or drug switching. However, with only the single viral target of the HBV DNA polymerase, the potential for development of cross-resistance becomes a real practical problem. Hence careful planning of any nucleos(t)ide analogue-based regimen should be an essential element in CHB patient management, which will also require regular monitoring for sustained HBV DNA suppression and viral rebound and resistance. If HBV DNA does not decrease within 12–24 weeks of initiation of therapy, clinicians should add or change therapy as long-term viral suppression and HBeAg loss and seroconversion is uncommon and there is an increased risk of resistance [44, 59].
Disease stage is a key factor in determining treatment strategy (Fig. 1). Among those patients with CHB with early cirrhosis who are immunocompetent and lack any other serious illness, treatment should be aimed to achieve sustained remission. On the other hand, for those patients with advanced cirrhosis and decompensation, who may be immunodeficient or have other serious disease, then treatment should be aimed at achieving maintained remission. Importantly, effective treatment with either approach, providing either sustained or maintained response, can achieve disease remission and thus prolong life. A basic algorithm to improve clinical outcomes is proposed in Fig. 2. In appropriately selected patients, immunomodulatory therapy of finite duration with PEG-IFN or conventional IFN should be the first-line treatment of choice. For those who do not achieve sustained remission, treatment of longer duration with nucleos(t)ide analogues should be instigated as second choice. However, nucleos(t)ide analogue therapy may be the treatment of choice for certain patient groups, such as the immunocompromised [60], those beginning chemotherapy [61], or pregnant with high HBV viral loads (>1,000 million copies/ml or ∼200 million IU/ml) [62] or those unwilling to take IFN therapy. While genotype appears to influence the rate of response to IFN therapies, with patients infected with HBV genotype A responding best, the infecting genotype has not yet been shown to have an effect on response to nucleos(t)ide analogues. Thus genotype may play a role in selecting first line therapy in areas where genotype A or D are prevalent but does not influence therapeutic decision where genotype B and C are common.
As well as deciding how to treat patients clinicians must also consider whether treatment is absolutely necessary, especially if resources are limited. Monitoring of patients, especially those with HBeAg-positive CHB without evidence of jaundice, every 3–6 months is important—they may not be in need of immediate treatment, since spontaneous HBeAg seroconversion can occur at a rate of ∼10% of patients per year. Current recommendations for therapy of chronic hepatitis B are summarised in Table 3 and modified from AASLD, EASL, APASL and expert treatment guidelines [3–6]. However, defining strict indications for initiating CHB treatment is problematic, due to the frequently fluctuating nature of the disease, e.g. HBV DNA <1,000 copies/ml (∼200 IU/ml) may indicate inactive disease, whereas >100,000 copies/ml (∼20,000 IU/ml) indicates active infection, but this level of HBV DNA accompanied by normal ALT and histology may indicate an immunotolerant state in a young person. Persistently elevated ALT levels, defined as ≥2 × upper limit of normal (ULN) with HBV DNA >100,000 copies/ml (∼20,000 IU/ml) are accepted as strong evidence to start treatment [3–6]. Elevated ALT levels plus HBV DNA levels of 10,000–100,000 copies/ml (∼2,000–20,000 IU/ml) have more recently been suggested as indication for treatment, but preliminary liver biopsy to establish moderate to severe inflammation or fibrosis is recommended before initiating therapy on a case-by-case basis [1, 6, 63].
Timing of treatment can influence the likelihood of response; high-baseline levels of ALT are known to be predictive of response to treatment both with IFN-based and nucleos(t)ide analogue therapy [64, 65]. Similarly, low-baseline HBV DNA levels have also been associated with an improved rate of response to IFN-based therapy. A ‘watch and wait’ strategy may be preferable to initiating immediate treatment, particularly in young patients who may have many years of therapy ahead of them.
An important factor to remember when counselling patients in need of anti-HBV therapy is the likelihood of requirement for long-term therapy if nucleos(t)ide analogues are initiated. Currently there are no evidence-based recommendations regarding when to stop nucleos(t)ide analogue therapy should HBeAg seroconversion occur, although reports suggest that 6–12 months appears prudent. It is also worth bearing in mind that HBeAg loss, used as a measure of treatment success in many trials of nucleos(t)ide analogues is not as stringent an outcome as HBeAg seroconversion, which requires not only HBeAg loss but also development of anti-HBe antibody. Although add-on use of nucleos(t)ide analogues may be necessary and beneficial in patients in whom nucleos(t)ide analogue-resistant virus has developed, some experts suggest that de novo use of nucleos(t)ide analogues in combination should be used. A study by Yim et al. [66] found that mutations conferring resistance to multiple antiviral agents co-locate on the same viral genome, suggesting that combination therapy directed against mutants resistant to each treatment may not be adequate in suppressing multi-drug resistant HBV; they conclude that de novo combination therapy may be required to prevent the emergence of multi-drug resistant mutants. Combination therapy with two nucleos(t)ide analogue drugs (lamivudine and tenofovir) has been suggested and has been shown to decrease the risk of resistance to lamivudine [56], however, tenofovir is currently licensed only for treatment of HIV infection and not for CHB. Choice of combination will be important; for example, a Phase II study of lamivudine in combination with telbivudine showed that the combination was less effective than lamivudine alone, suggesting an antagonistic effect [67]. Further studies are required to elucidate the long-term effects of resistance development.
In conclusion, we propose a unified treatment strategy for the management of patients with CHB in order to make best possible use of the resources currently available. Education, both of physicians and patients, is a key factor in combating CHB. Effective treatments for the management of CHB are available; the basic algorithm for their use suggested here should be regarded as an initial framework for further development.
Abbreviations
- ALT:
-
Alanine aminotransferase
- CHB:
-
Chronic hepatitis B infection
- HBV:
-
Hepatitis B virus
- HBeAg:
-
Hepatitis B e antigen
- HBsAg:
-
Hepatitis surface antigen
References
Hui CK, Lau GK. Current issues and future directions in treatment. Semin Liver Dis 2006;26(2):192–7.
Yim HJ, Lok AS. Natural history of chronic hepatitis B virus infection: what we knew in 1981 and what we know in 2005. Hepatology 2006;43 2 Suppl 1:S173–81.
The EASL Jury. EASL consensus conference on hepatitis B. J Hepatol 2003;38:533–40.
Lok ASF, McMahon BJ. Chronic hepatitis B. Hepatology 2007;45:507–39.
Liaw Y-F, Leung N, Guan R, Lau GKK, Merican I, McCaughan G, Gane E, Kao J-H, Omata M for the Asian-Pacific consensus update working party on chronic hepatitis B. Asian-Pacific consensus statement on the management of chronic hepatitis B: a 2005 update. Liver Int 2005;25:472–89.
Keeffe EB, Dieterich DT, Han S-H, Jacobson IM, Martin P, Schiff ER, Tobias H, Wright TL. A treatment algorithm for the management of chronic hepatitis B virus in the United States: an update. Clin Gastroenterol Hepatol 2006;4:936–62.
Lavanchy D. Hepatitis B virus epidemiology, disease burden, treatment and current and emerging prevention and control measures. J Virol Hepat 2004;11:97–107.
WHO. The world health report. Geneva, Switzerland: World Health Organization; 1997.
WHO. Hepatitis B WHO fact sheet (Revised Oct 2000). WHO web site. http://www.who.int/mediacentre/factsheets.fs204/en/print.html.
El-Serag HB, Mason AC. Rising incidence in HCC in the US. N Engl J Med 1999;340:745–70.
Chen C-J, Yang H-I, Su J, Jen C-L, You S-L, et al. Risk of HCC across a biological gradient of serum HBV DNA level. JAMA 2006;295:65–73.
Parkin DM, Ferlay J, Pisani P. Estimating the world cancer burden: Globocan 2000. Int J Cancer 2001;92:153–6.
Perz JF, Armstrong GL, Farrington LA, Hutin YJ, Bell BP. The contributions of hepatitis B virus and hepatitis C virus infections to cirrhosis and primary liver cancer worldwide. J Hepatol 2006;45:529–38.
Chen G, Lin W, Shen F, Iloeje UH, London WT. Chronic hepatitis B infection and mortality from non-liver causes: results from the Haimen cohort study. Intl J Epidemiol 2005;34:132–7.
Lok AS, Heathcote EJ, Hoofnagle JH. Management of hepatitis B: 2000 – summary of a workshop. Gastroenterology 2001;120:1828–53.
Allain JP. Epidemiology of hepatitis B virus and genotype. J Clin Virol 2006;36 Suppl 1:S12–7.
Chu CJ, Keeffe EB, Han SH, et al. Hepatitis B virus genotypes in the United States: results of a nationwide study. Gastroenterology 2003;125(2):444–51.
França HC, González JE, Silvina Munné M, Brandão LH, Gouvea VS, Sablon E, Bart OM. Vanderborght strong association between genotype F and hepatitis B virus (HBV) e antigen-negative variants among HBV-infected Argentinean blood donors. J Clin Microbiol 2004;42(11):5015–21.
Funk ML, Rosenberg DM, Lok ASF. World-wide epidemiology of HBeAg-negative chronic hepatitis B and associated precore and core promoter variants. J Viral Hepat 2002;9:52–61.
Mohamed R, Desmond P, Suh DJ, Amarapurkar D, Gane E, Guangbi Y, Hou JL, Jafri W, Lai CL, Lee CH, Lee SD, Lim SG, Guan R, Phiet PH, Piratvisuth T, Sollano J, Wu JC. Practical difficulties in the management of hepatitis B in the Asia-Pacific region. J Gastroenterol Hepatol 2004;19(9):958–69.
Fattovich G, Giustina G, Sanchez-Tapias J, Quero C, Mas A, Olivotto PG, Solinas A, Almasio P, Hadziyannis S, Degos F, de Moura MC, Krogsgaard K, Pantalena M, Realdi G, Corrocher R, Schalm SW. Delayed clearance of serum HBsAg in compensated cirrhosis B: relation to interferon alpha therapy and disease prognosis. European concerted action on viral hepatitis (EUROHEP). Am J Gastroenterol 1998;93(6):896–900.
Fattovich G, Rugge M, Brollo L, Pontisso P, Noventa F, Guido M, Alberti A, et al. Clinical, virologic and histologic outcome following seroconversion from HBeAg to anti-HBe in chronic hepatitis type B. Hepatology 1986;6:167–72.
Niederau C, Heintges T, Lange S, Goldmann G, Niederau CM, Mohr L, Haussinger D. Long-term follow-up of HBeAg-positive patients treated with interferon alfa for chronic hepatitis B. N Engl J Med 1996;334:1422–7.
Wong DKH, Cheung AM, O’Rourke K, et al. Effect of alpha interferon treatment in patients with hepatitis B e antigen-positive chronic hepatitis B. Ann Intern Med 1993;119:312–23.
Lok ASF, Lai CL, Wu PC, et al. Long-term follow-up in a randomised trial of recombinant alpha2-interferon in Chinese patients with chronic hepatitis B infection. Lancet 1988;2:298–302.
Bortolotti F, Jara P, Barbera C, et al. Long term effect of alpha interferon in children with chronic hepatitis B. Gut 2000;46:715–8.
Korenman J, Baker B, Waggoner J, Everhart JE, Di Bisceglie AM, Hoofnagle JH. Long-term remission of chronic hepatitis B after alpha-interferon therapy. Ann Intern Med 1991;114(8):629–34.
Lin SM, Yu ML, Lee CM, Chien RN, Sheen IS, Chu CM, Liaw YF. Interferon therapy in HBeAg positive chronic hepatitis reduces progression to cirrhosis and hepatocellular carcinoma. J Hepatol 2007;46(1):45–52.
Hadziyannis SJ. Hepatitis B e antigen negative chronic hepatitis B: from clinical recognition to pathogenesis and treatment. Viral Hep Rev 1995;1:7–36.
Marcellin P, Lau GK, Bonino F, et al. Peginterferon alfa-2a alone, lamivudine alone, and the two in combination in patients with HBeAg-negative chronic hepatitis B. N Engl J Med 2004;351:1206–17.
Lau GK, Piratvisuth YT, Luo KX, et al. Peginterferon alfa-2a, lamivudine and the combination for HBeAg-positive chronic hepatitis B. N Engl J Med 2005;352:2682–95.
Cooksley WG, Piratvisuth T, Lee SD, Mahachai V, Chao YC, Tanwandee T, Chutaputti A, Chang WY, Zahm FE, Pluck N. Peginterferon alpha-2a (40 kDa): an advance in the treatment of hepatitis B e antigen-positive chronic hepatitis B. J Viral Hepat 2003;10(4):298–305.
Lau GK, Piratvisuth T, Luo KX, Marcellin P, Thongsawat S, Cooksley G, Gane E, Fried MW, Popescu M, Wu J. Durability of response and occurrence of late response to peginterferon-alpha-2a (40 KD) [PEGASYS] one year post-treatment inpatients with HBeAg-positive chronic hepatitis B. J Hepatol 2006;44 Suppl 2:S23 (Abstract 50).
Janssen HL, van Zonneveld M, Senturk H, Zeuzem S, Akarca US, Cakaloglu Y, Simon C, So TM, Gerken G, de Man RA, Niesters HG, Zondervan P, Hansen B, Schalm SW, HBV 99-01 Study Group, Rotterdam Foundation for Liver Research. Pegylated interferon alfa-2b alone or in combination with lamivudine for HBeAg-positive chronic hepatitis B: a randomised trial. Lancet 2005;365(9454):123–9.
Marcellin P, Bonino F, Lau GK, Farci P, Yurdaydin C, Piratvisuth T, Jin R, Gurel S, Hadziyannis S, Lu Z-M, Popescu M. The majority of patients with HBeAg-negative chronic hepatitis B treated with peginterferon-alpha-2a (40 KD) [PEGASYS] sustain response 2 years post-treatment. J Hepatol 2006;44 Suppl 2:S274 (Abstract 743).
Liaw YF. Results of lamivudine in Asian trials. Proceedings of EASL international consensus conference on hepatitis B: 2002. J Hepatol 2003;39:S111–5.
Lok AS, Lai CL, Leung N, Yao GB, Cui ZY, Schiff ER, Dienstag JL, et al. Long-term safety of lamivudine treatment in patients with chronic hepatitis B. Gastroenterology 2003;125:1714–22.
Tassopoulos NC, Volpes R, Pastore G, Heathcote J, Buti M, Goldin RD, Hawley S, et al. Efficacy of lamivudine in patients with hepatitis B e antigen-negative/hepatitis B virus DNA-positive (precore mutant) chronic hepatitis B. Lamivudine Precore Mutant Study Group. Hepatology 1999;29:889–96.
Santantonio T, Mazzola M, Iacovazzi T, Miglietta A, Guastadisegni A, Pastore G. Long-term follow-up of patients with anti-HBe/HBV DNA-positive chronic hepatitis B treated for 12 months with lamivudine. J Hepatol 2000;32:300–6.
Rizzetto M, Marzano A, Lagget M. Treatment of hepatitis B e antigen-negative chronic hepatitis B with lamivudine. J Hepatol 2003;39:S168–71.
Lampertico P, Vigano M, Iavarone M, Lunghi G, Romeo R, Colucci G, Morabito A, Del Nino E, Columbo M. The long-term outcome of HBeAg-negative patients with cirrhosis treated with lamivudine monotherapy: a five-year prospective cohort study. J Hepatol 2004; Abstract 44.
Liaw Y. Management of YMDD mutations during lamivudine therapy in patients with chronic hepatitis B. J Gastroenterol Hepatol 2002;17:S333–7.
Hadziyannis SJ, Tassopoulos NC, Heathcote EJ, Chang TT, Kitis G, Rizzetto M, Marcellin P, Lim SG, Goodman Z, Ma J, Brosgart CL, Borroto-Esoda K, Arterburn S, Chuck SL, Adefovir Dipivoxil 438 Study Group. Long-term therapy with adefovir dipivoxil for HBeAg-negative chronic hepatitis B for up to 5 years. Gastroenterology 2006;131(6):1743–51.
Locarnini S, Qi X, Arterburn S, Snow A, Brosgart CL, Currie G, Wulfsohn M, Miller M, Xiong S. Incidence and predictors of emergence of HBV mutations associated with adefovir resistance during 4 years of adefovir therapy for patients with chronic hepatitis B. 40th EASL Meeting, 2005, Paris, France. Oral # 36.
Hadziyannis SJ, Tassopoulos NC, Heathcote EJ, et al. Adefovir dipivoxil for the treatment of HBeAg-negative chronic hepatitis B. N Engl J Med 2003;348:800–7.
Hadziyannis S, Tassopoulos NC, Chang TT, et al. Long-term adefovir dipivoxil treatment induces regression of liver fibrosis in patients with HBeAg-negative chronic hepatitis B: results after 5 years of therapy. Hepatology 2005;42 Suppl 1:754A.
Chang TT, Gish RG, de Man R, et al. A comparison of entecavir and lamivudine for HBeAg-positive chronic hepatitis B. N Engl J Med 2006;354:1001–10.
Lai CL, Shouval D, Lok AS, et al. Entecavir versus lamivudine for patients with HBeAg-negative chronic hepatitis B. N Engl J Med 2006;354:1011–20.
Bzowej N, Lai C, Gane L, et al. Phase III comparison of telbivudine vs lamivudine in patients with chronic hepatitis B: efficacy, safety, and predictors of response at 1 year [Abstract]. Gastroenterology 2006;130 Suppl 2:A765–6.
Jones R, Nelson M. Novel anti-hepatitis B agents: a focus on telbivudine. Int J Clin Pract 2006;60(10):1295–9.
Heathcote E, Chan H, Cho M, et al. A randomized trial of telbivudine (LdT) vs. adefovir for HBeAg-positive chronic hepatitis B: results of the primary week 24 analysis [Abstract]. Gastroenterology 2006;130 Suppl 2:A765.
Marcellin P, Mommeja-Marin H, Sacks SL, Lau GK, Sereni D, Bronowicki JP, Conway B, Trepo C, Blum MR, Yoo BC, Mondou E, Sorbel J, Snow A, Rousseau F, Lee HS. A phase II dose-escalating trial of clevudine in patients with chronic hepatitis B. Hepatology 2004;40(1):140–8.
Hui CK, Lau GK. Clevudine for the treatment of chronic hepatitis B virus infection. Expert Opin Investig Drugs 2005;14(10):1277–84.
Colonno RJ, Rose R, Baldick CJ, Levine S, Pokornowski K, Yu CF, Walsh A, Fang J, Hsu M, Mazzucco C, Eggers B, Zhang S, Plym M, Klesczewski K, Tenney DJ. Entecavir resistance is rare in nucleoside naive patients with hepatitis B. Hepatology 2006;44(6):1656–65.
Tenney DJ, Levine SM, Rose RE, et al. Clinical emergence of entecavir resistant hepatitis B virus requires additional substitutions in virus already resistant to Lamivudine. Antimicrob Agents Chemother 2004;48:3498–507.
van Boemmel F, Mauss S, Shuermann D, et al. No evidence for tenefovir resistance in patients with lamivudine-resistant HBV infection during long-term treatment for up to 5 years. Hepatol 2006;44(4):549A.
Lim SG, Krastev Z, Ng TM, et al. Randomized, double-blind study of emtricitabine (FTC) plus clevudine versus FTC alone in treatment of chronic hepatitis B. Antimicrob Agents Chemother 2006;50:1642–8.
Lee YS, Suh DJ, Lim YS, Jung SW, Kim KM, Lee HC, Chung YH, Lee YS, Yoo W, Kim SO. Increased risk of adefovir resistance in patients with lamivudine-resistantchronic hepatitis B after 48 weeks of adefovir dipivoxil monotherapy. Hepatology 2006;43(6):1385–91.
Dan Y, Wai C, Lim S. Modeling for the most cost-effective treatment strategy for eAg positive chronic hepatitis B. Hepatology 2006 (Abstract).
Shibolet O, Ilan Y, Gillis S, Hubert A, Shouval D, Safadi R. Lamivudine therapy for prevention of immunosuppressive-induced hepatitis B virus reactivation in hepatitis B surface antigen carriers. Blood 2002;100:391–6.
Yeo W, Chan PK, Ho WM, et al. Lamivudine for the prevention of hepatitis B virus reactivation in hepatitis B s-antigen seropositive cancer patients undergoing cytotoxic chemotherapy. J Clin Oncol 2004;22:927–34.
van Zonneveld M, van Nunen AB, Niesters HG, de Man RA, Schalm SW, Janssen HL. Lamivudine treatment during pregnancy to prevent perinatal transmission of hepatitis B virus infection. J Viral Hepat 2003;10:294–7.
McMahon BJ. Selecting appropriate management strategies for chronic hepatitis B: who to treat. Am J Gastroenterol 2006;101 Suppl 1:S7–12.
Perrillo RP. Acute flares in chronic hepatitis B: the natural and unnatural history of an immunologically mediated liver disease. Gastroenterology 2001;120(4):1009–22.
Perrillo RP, Lai CL, Liaw YF, Dienstag JL, Schiff ER, Schalm SW, Heathcote EJ, Brown NA, Atkins M, Woessner M, Gardner SD. Predictors of HBeAg loss after lamivudine treatment for chronic hepatitis B. Hepatology 2002;36(1):186–94.
Yim HJ, Hussain M, Liu Y, Wong SN, Fung SK, Lok AS. Evolution of multi-drug resistant hepatitis B virus during sequential therapy. Hepatology 2006;44(3):703–12.
Lai CL, Leung N, Teo EK, Tong M, Wong F, Hann HW, Han S, Poynard T, Myers M, Chao G, Lloyd D, Brown NA, Telbivudine Phase II Investigator Group. A 1-year trial of telbivudine, lamivudine, and the combination in patients with hepatitis B e antigen-positive chronic hepatitis B. Gastroenterology 2005;129(2):528–36.
Author information
Authors and Affiliations
Corresponding author
Additional information
See related article: DOI 10.1007/s12072-007-9005-6
Dr. Peters reports receiving consulting or lecture fees from Idenix, Hoffman La Roche, Gilead Sciences; grant support from Achillion Pharmaceuticals and serving on the data safety monitoring board for Glaxo Smith Kline. Dr. Lau reports receiving consulting or lecture fees from Hoffman La Roche and Novaritis; grant support from Hoffman La Roche, Novarits, Bukwang and Gilead Sciences. Dr. Marcellin reports receiving consulting or lecture fees from BMS, Coley Pharma, Gilead, GSK, HGS, Idenix-Novartis, Roche, Schering Plough, Valeant and Vertex and grant support from BMS, Gilead, GSK, HGS, Idenix-Novartis, Roche, Schering Plough, Valeant and Vertex.
Rights and permissions
About this article
Cite this article
Lau, G., Marcellin, P. & Peters, M. Chronic hepatitis B: a global health problem requiring coherent worldwide treatment strategies. Hep Intl 1, 316–325 (2007). https://doi.org/10.1007/s12072-007-9006-5
Received:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12072-007-9006-5