Abstract
Solitary fibrous tumors (SFTs) belonging to a distinct group of mesenchymal tumors, was originally described by Klemper and Rabin in the pleura in year 1931. However, it can also be extra-pleural in origin. With tongue being the most common site involved in this region, epiglottis, larynx, thyroid, external auditory canal, lacrimal sac, hypoglossal nerve, parotid gland, sublingual gland, Para pharyngeal space, nasopharynx, scalp, gingiva, orbit and infratemporal fossa as well as paranasal sinuses and nasal cavities can also get involved. But SFTs involving nasal cavities and nasopharynx are quite uncommon, accounting for < 0.1% of all Sino-nasal neoplasms. Until now there have only been 40 cases of nasal SFT reported in literature. We report the case of an extraserosa solitary fibrous tumor arising from the nasal cavity with extension to the sphenoid sinus, a much rarer presentation of its type. Our case report is one of its type, emphasizing the need conducting further studies on the nature and management of the disease.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Solitary fibrous tumors (SFTs) belonging to a distinct group of mesenchymal tumors, was originally described by Klemper and Rabin in the pleura in year 1931 [1]. However, it can also be extra-pleural in origin and 12–15% develops in head and neck region [2]. With tongue being the most common site involved in this region, epiglottis, larynx, thyroid, external auditory canal, lacrimal sac, hypoglossal nerve, parotid gland, sublingual gland, Para pharyngeal space, nasopharynx, scalp, gingiva, orbit and infratemporal fossa as well as paranasal sinuses and nasal cavities can also get involved [3]. But SFTs involving nasal cavities and nasopharynx are quite uncommon [4], accounting for < 0.1% of all Sino-nasal neoplasms [5]. Until now there have only been 40 cases of nasal SFT reported in literature.
We report the case of an extra-serosa solitary fibrous tumor arising from the nasal cavity with extension to the sphenoid sinus, a much rarer presentation of its type.
Case Details
A 63-year-old male, presented at otorhinolaryngology department of a tertiary care hospital, with progressive unilateral right-sided constant nasal obstruction and intermittent epistaxis for 2 years, now followed by headache and right orbital pain in the last 4 months, not associated with any ocular and neurologic signs. Nasal endoscopy revealed pale to slightly reddish smooth mass in the right nasal cavity extending up to the nasopharynx, occupying complete nasal cavity proper of the right side, and pushing the septum towards left side causing narrowing of left nasal cavity (Fig. 1).
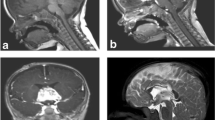
CT scan paranasal sinuses with IV contrast revealed a well-circumscribed avidly contrast enhancing soft tissue mass occupying the right nasal cavity, with opacity shown in right sided sphenoid and ethmoid sinuses abutting lamina papyracea and medial wall of right maxillary sinus laterally and nasal septum towards the left side. There was suspected erosion of anterior aspect of medial orbital wall near lacrimal sac. Posteriorly the mass was hanging into nasopharynx. No evidence of intra cranial extension of the mass lesion (Fig. 2).
CT scan paranasal sinuses (contrast enhanced: axial and sagittal sections) showing a well-circumscribed avidly contrast enhancing soft tissue mass occupying the right nasal cavity, with opacity abutting lamina papyracea and medial wall of right maxillary sinus laterally and nasal septum towards the left side. There was suspected erosion of anterior aspect of medial orbital wall near lacrimal sac. Posteriorly the mass was hanging into nasopharynx. No evidence of intra cranial or intra-orbital extension of the mass lesion
Intervention radiologist was taken on board due to moderate to high vascular nature of mass, and embolization prior to procedure was planned. Bilateral ECA and ICA angiograms showed abnormal tumor blush in expected location from right internal maxillary branch of right ECA predominantly (Fig. 3). Embolization was performed using 350–500 PVA particles.
Intra-operatively, the tumor was seen to involve right nasal cavity along with the sphenoid sinus while eroding the right lamina papyracea. The lesion was smooth and firm in consistency without infiltrating borders. The tumor appeared to originate from right spheno-ethmoidal recess penetrating into the sphenoid sinus via its ostium. It was separated from maxillary osteo-meatal complex, medial and lateral wall of the right-sided nasal cavity. Tumor was completely excised in multiple irregular fragments and sent for histopathology (Fig. 4). Post-operatively, there were no complications.
Microscopic sections show an ill-defined spindle cell lesion beneath the surface epithelium comprising of haphazardly oriented short spindle cells in a densely collagenous background. Admixed dilated vasculature is also appreciated. These are dilated vascular spaces resembling horns, the so called staghorn vasculature. On higher magnification, these spindle cells show small, oval, elongated nuclei with vesicular chromatin and elongated eosinophilic cytoplasm merging with the cytoplasm of the adjacent spindle cells. These tumor cells were diffusely positive for immunohistochemically stains STAT-6 while focally positive for CD34. Other spindle cell markers including S100, ASMA and Beta Catenin were negative, leading the diagnosis to solitary fibrous tumor (Fig. 5).
Microscopic sections show an ill-defined spindle cell lesion beneath the surface epithelium comprising of haphazardly oriented short spindle cells. Admixed dilated vasculature is also appreciated, the so called staghorn vasculature. On higher magnification, these tumor cells were diffusely positive for immunohistochemically stains STAT-6 while focally positive for CD34. Other spindle cell markers including S100, ASMA and Beta Catenin were negative, leading the diagnosis to solitary fibrous tumor
Discussion
SFT is a rare apathetic tumor [4] mostly benign but sometimes malignant, with very few reports on this condition. Tumors of this type comprises of 2% of soft tissue tumors, usually pleural in origin. Of all reported cases, 12–15% were located in the head and neck region [2]. Meanwhile, less than 5% arising in sino-nasal region [6]. In accordance with our study, SFT arising from the spheno-ethmoidal recess, penetrating into the sphenoid sinus are seldom to report, so far only one case has been reported in literature.
SFTs are derived from mesenchymal fibroblast-like cells, generally involve adults in fourth and fifth decade of life with no sex predilection [4]. Extra-pleural SFTs are mostly benign in nature. None of the SFT arising in the sino-nasal region have been reported to be malignant however hyper cellularity, necrosis, greater than 4 mitoses/10 HPFs and nuclear atypia were seen in up to five reported cases of extra-plural region [2]. With only two reported cases of solitary fibrous tumors in the nasal cavity, it's impossible to assess their malignant potential. Its recurrence is dependent on the excision of the lesion and if the tumor is excised completely and the tumor not involving the anatomical sites which are difficult to approach then the rate of recurrence is close to negligible [7].
In contrast 23% of SFTs arising in pleura showed more aggressive behavior, exhibiting local infiltration, intrathoracic spread, local recurrence or distant metastasis [8].
The most prominent clinical feature displayed by nasal-SFT is nasal obstruction commonly unilateral. Other symptoms could be epistaxis and nasal discharge, hyposmia, epiphora, proptosis, and headache [4]. Endoscopically, it appears as smooth, red, encapsulated fibrous unilateral nasal mass [3].
Histopathologically, it mainly comprises of cytologically plain spindle cells [4] organized without an obvious pattern [2]. Characteristically, tumor cells are parted by thick bands of collagen representing foci of keloid-like hyalinization [7]. Moreover, they exhibit significant vascularity showing a haemangiopericytoma-like vascular pattern, with which they are constantly being confused [7]. The tumor cells usually stain positive for CD34, vimentin and not by S-100 protein. It is known that CD34 marker is strongly sensitive [7] however not entirely specific for SFT as expressed in various other spindle cell malignancies [2].
Imaging is an important means in the diagnosis of SFTs. Enhanced head and neck CT and MRI are the ideal imaging modalities. SFTs show marked enhancement on giving IV contrast considering their high vascularity [9]. In our case, CT scan was preferred to clearly identify the extent of the disease.
The definitive treatment for SFT is total excision of the mass so as to lower the chances of recurrence [2]. Disease existing in anatomical sites difficult to approach for complete resection such as periorbital region and nasopharynx, or having a malignant component within has a high possibility of local recurrence [7], requiring vigilant and long-term follow-up. The role of adjuvant therapy, chemotherapy or radiotherapy, still remains unestablished and is usually not suggested due to lower possibility of recurrence in non-malignant cases [7].
Conclusion
Extra-pulmonary solitary fibrous tumor is rare and un-explored pathology with sino-nasal region being the most uncommon. Our case report is one of its type, emphasizing the need conducting further studies on the nature and management of the disease.
Data Availability
Not applicable as it’s a case report.
References
Klemperer P, Rabin CB (1931) Primary neoplasms of the pleura. A report of five cases. Arch Pathol 11:385–412. https://doi.org/10.1002/ajim.4700220103
Thomas LS, Latorre AR, Arias VL, Acosta BJ, Francia AL (2022) Solitary fibrous tumor involving the nasal cavity and paranasal sinuses with intracranial and dural compromise: a case report and literature review. Int J Otorhinolaryngol Clin 14(2):71–75
Janjua A, Sklar M, MacMillan C, Vescan A, Witterick IJ (2011) Endoscopic resection of solitary fibrous tumors of the nose and paranasal sinuses. Skull Base 21:129–34
Wu H, Hu X, Xiang W, Liu N, Fang S, Xu T, Qi Y, Zheng L, Cai W, Wu C, Yu H (2022) A large solitary fibrous tumor of the nasal cavity and paranasal sinuses involving the anterior frontal fossa: a case report and review of the literature. Ear Nose Throat J 17:01455613221113809
Kakkar A, Sakthivel P, Rajeshwari M, Kairo A, Sharma MC (2020) Recurrent sinonasal CD34-negative malignant solitary fibrous tumor diagnosed on STAT6 immunohistochemistry and NAB2-STAT6 fusion. Head Neck Pathol 14:250–256
Peng Z, Wang Y, Wang Y, Li Q, Fang Y, Fan R, Zhang H, Jiang W (2022) Hemangiopericytoma/solitary fibrous tumor of the cranial base: A case series and literature review. BMC surgery 22(1):1–9
Khribi M, Wassim K, Abir M, Sriha B, Bellakhdhar M, Abdelkefi M (2022) Solitary fibrous tumor of nasal cavity: a case report and review of literature. Int J Surg Case Rep 93:106950
Mathew GA, Ashish G, Tyagi AK, Chandrashekharan R, Paul RR (2015) Solitary fibrous tumor of nasal cavity: a case report. Iran J Otorhinolaryngol 27(81):307
Yang BT, Song ZL, Wang YZ, Dong JY, Wang ZC (2013) Solitary fibrous tumor of the sino nasal cavity: CT and MR imaging findings. Am J Neuroradiol 34(6):1248–1251
Acknowledgements
None to declare.
Funding
This study was not funded by any authority.
Author information
Authors and Affiliations
Contributions
FJ: Data collection and writing of manuscript; YA: Data collection and writing of manuscript; MW: literature search, overall supervision; SA: writing of manuscript, and submission; MZ: Substantial contribution in manuscript; AQ: Substantial contribution in manuscript.
Corresponding author
Ethics declarations
Conflict of interest
All authors declare that there is no conflict of interest.
Ethical Approval
Not applicable.
Informed Consent
Consent form was taken and duly signed by the participant of the case report.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Jabbar, F., Afzal, Y., Wasif, M. et al. Solitary Fibrous Tumor of Nasal Cavity: A Case Report. Indian J Otolaryngol Head Neck Surg 76, 2910–2914 (2024). https://doi.org/10.1007/s12070-024-04538-6
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12070-024-04538-6