Abstract
Study post treatment improvement of Laryngopharyngeal Reflux Disease (LPRD) using non-invasive tools of Reflux symptom index (RSI), Reflux finding score (RFS) grading of videolaryngostroboscopy (VLS) and voice analysis. This study from December 2020 to April 2022 enrolled 100 adults with complaints suggestive of reflux symptoms and having Reflux Symptom Index (RSI) more than 13. All patients underwent VLS along with voice analysis. VLS findings were graded using Reflux Finding Score (RFS). Patients were advised for lifestyle modifications and proton pump inhibitors for 8 weeks when post treatment RSI, VLS and voice analyses were again documented. The age range was from 18 to 75 years. Males predominated. Lifestyle modification compliance was seen in 85% of the patients. We found a significant association (P = 0.001) for difference in pretreatment and posttreatment for both Reflux Symptom Index (RSI) parameters & Reflux Finding Score Index (RFS) parameters. Voice analysis pre and post treatment showed a significant association (P = 0.001) for fundamental frequency, jitter, shimmer, harmonic-to-noise ratio and maximum phonation time. The gold standard of diagnosis of LPRD is 24 h pH monitoring but has many false negatives and false positives due to intermittent reflux and inaccurate probe placement. This costly, time consuming and invasive procedure is not widely available amongst our speciality. Excellent visualisation of VLS allowed accurate RFS calculation. Voice analysis permitted early diagnosis of LPRD induced hoarseness before it became clinically significant. It also documented the treatment outcome. We conclude that an 8-weeks proton pump inhibitor treatment combined with lifestyle modification resulted in a significant improvement in the parameters of the non-invasive tools of RSI and RFS and voice analysis.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Laryngopharyngeal reflux disease (LPRD) is an inflammatory reaction of the mucous membranes of the pharynx, larynx, and other respiratory organs caused by stomach contents refluxing into the oesophagus. Laryngopharyngeal reflux disease (LPRD) is a relatively new clinical entity, which is being treated using various modalities, often without a confirmed diagnosis [1]. The gold standard of diagnosis of LPRD is 24 h pH monitoring but has many limitations. Intermittent reflux may not occur during the test period of 24 h. Even 3 episodes per week can be sufficient to generate LPR symptoms. These intermittent reflux episodes often lead to false negatives. False negatives or false positives also occur secondary to inaccurate the probe placement, movement or irritation. This costly, time consuming and invasive procedure is not widely available amongst our speciality.
The prevalence of LPRD in the Indian population is around 11% [2]. Reflux of stomach contents can be linked to LPRD in two ways [2]. It is caused mostly by direct exposure of the laryngopharyngeal mucosa to gastric contents. Second an indirect mechanism occurs when the reflux material interacts with the mucosa distal to the larynx, causing vagally mediated bronchoconstriction. Because it lacks both extrinsic and intrinsic epithelial defences (anti-reflux barrier), the larynx is more vulnerable to reflux injury than the oesophagus [3].
The symptoms of laryngopharyngeal reflux disease include chronic cough, frequent throat clearing, dysphagia, chronic throat irritation, foreign body sensation in the throat, hoarseness, excessive phlegm, heart burn, regurgitation of food and breathing difficulty [1]. 50–78% of LPRD patients have complaints of change in voice and 91% of elderly patients have voice disorders [4]. This can be diagnosed by subjective and objective voice assessment without using 24 h pH manometry. [4] Heartburn accounts for less than 40%, whereas oesophagitis involves only 25% patients [4]. Extra oesophageal complications such as emphysema, asthma or bronchitis can be caused by laryngopharyngeal reflux disease [5].
LPRD not only has a significant negative impact on patient quality of life but it can also predispose to many laryngeal diseases such as reflux laryngitis, granulomas, contact ulcers, vocal nodules, subglottic stenosis and carcinoma of larynx [6].
The risk factors for LPRD include excessive food intake, alcohol or tobacco use, pregnancy, malfunctioning or deformed oesophageal sphincter, obesity and reduced gastric motility [7].
Reflux Symptom Index (RSI) is a 9-item self-administered outcome instrument, that accurately documents the symptoms of patients with LPRD. This tool is highly reliable and reproducible [8]. An RSI value of > 13 has been considered to indicate LPRD [8]. The RSI values ranges from 0 to 45, where 45 shows the worst possible score [8].
Videolaryngostroboscopy (VLS) is a sensitive tool in the diagnosis of LPRD in patients with voice complaints. On a videolaryngostroboscopy, LPRD signs include posterior commissure hypertrophy, laryngeal erythema, vocal fold edema, diffuse laryngeal edema, thick endolaryngeal mucous, ventricular obliteration, subglottic edema and granulations [9]. Like indirect laryngoscopy, during VLS the scope stays within oropharynx. This is a lesser invasive procedure than 24 h pH monitoring where the probe reaches stomach and reading can be erroneous in case of inaccurate probe placement [4].
Reflux Finding Score (RFS) is used in the diagnosis and monitoring of laryngopharyngeal reflux disease. It is an 8-item clinical severity rating scale based on endoscopic findings. The scale ranges from 0 to 26. Score increases with severity of the disease. An RFS value of > 7 indicates 95% probability of having LPRD10. In a study done by Belafsky et al. [10] the correlation coefficient for interobserver variability for reflux finding score was 0.90, which shows that this tool is highly reliable and reproducible.
Assessment of voice can be done both objectively and perceptually. Objective measures can be grouped into physiological measures, acoustic measures and aerodynamic measures [11]. Physiological evaluation can be done through instrumental techniques like, indirect laryngoscopy, videolaryngostroboscopy, flexible fiberoptic endoscopy, ultrahigh speed photography etc. Physiological evaluation procedures mainly help to view the laryngeal structure and assess organic pathologies which have resulted in a change in voice. Acoustic analysis involves assessing various vocal parameters objectively. Commonly assessed parameters include fundamental frequency, jitter, shimmer, harmonic to noise ratio, etc. [12]. Normal range of these acoustic parameters have been described in various studies and may vary between different software programs.
Many software programs such as Dr.Speech (Tiger DRS, Inc) [13], MDVP software of Visi-Pitch IV (KayPentax Inc., USA), [14] Computerized Speech Lab (CSL, Kay Elemetrics) [15], VAGHMI (Voice and Speech Systems, VSS, Bangalore) [16] are used for voice analysis. We used Dr. Speech Software in this study. The acoustic analysis parameters are hereby discussed.
Fundamental Frequency
(F0) is the frequency or the rate of vibration of vocal folds. It is the psychoacoustic co-relate of pitch. Unit of measurement of F0 is Hertz. Normal values of fundamental frequency in males ranges from 100–150 Hz while in females the corresponding range is 180–250 Hz. [17].
Maximum Phonation Time
Maximum phonation time refers to the maximum duration that a particular vowel sound can be sustained. Maximum phonation time in males varies between 25 and 35 s while in females it is between 15 and 25 s. [17].
Jitter / Frequency Perturbation
Jitter is the measure of instability of the vocal cord during sustained phonation. Frequency perturbation or jitter refers to the variation of fundamental frequency present in all speakers to some degree and detected when the subject is attempting to produce a steady, sustained vowel. The frequency variations are the result of instability of the vocal folds during vibration. Normal speakers have a small amount of frequency perturbations, which may vary according to age, sex and physical condition. Normal value of Jitter is < 1%[17].
Shimmer / Amplitude Perturbation
During sustained vibration, the vocal cords exhibit slight variation of amplitude from one cycle to the next. This is called amplitude perturbation or “shimmer”. Normal value of shimmer is < 2.85%[17].
Harmonic to Noise Ratio (HNR)
Voice is composed of periodic and random noise (aperiodic waves). Noise is a sound and is not a harmonic of fundamental note. If the noise component of voice increases and replaces the harmonic structure, the quality of hoarseness is perceived, and this is measured as the harmonic to noise ratio. Harmonicity is expressed in Db. If 99% of the energy of the signal is in the periodic part and 1% is noise, the HNR is 10 × log10(99/1) = 20 Db. [17].
Treatment for LPRD includes life style modifications such as multiple small meals, weight loss, avoidance of smoking, alcohol, and bedtime snacks. Caffeine, chocolate, carbonated beverages and high fat diet are also to be restricted. These changes have been found to be a major independent predictor of response to medical treatment. [18]
RSI is a questionnaire while VLS and Voice analysis are noninvasive procedures. In view of the various limitations of 24 h pH monitoring we these clinical scales of reflux symptom index (RSI), videolaryngostroboscopy and voice analysis as tools to assess post treatment improvement of LPRD. All patients were treated with proton pump inhibitors (PPI) and advised lifestyle modifications (LSM).
Material and Methods
Place of Study
The present study was conducted in the Department of Otorhinolaryngology, in a tertiary care teaching hospital in Central India.
Study Design
Prospective, interventional study.
Study Duration
The duration was from December 2020 to April 2022.
Study Population
All the patients coming to the ENT OPD of the institution during the study period with complaints suggestive of reflux symptoms were given RSI questionnaire and those with a score of more than 13 were included in the study. Symptoms suggestive of reflux are cough, frequent throat clearing, dysphagia, foreign body sensation in throat, hoarseness, excessive phlegm in throat, regurgitation and heart burn.
Inclusion Criteria
-
Consenting adults
-
Patient with Reflux Symptom Index more than 13
Exclusion Criteria
-
Professional voice users or having history of vocal abuse
-
History of trauma or laryngeal surgery
-
Patient with neurological or mass lesions involving larynx
-
Where videolaryngostroboscopy could not be performed due to lack of patient cooperation or any other reason
Methodology
All the adult patients with complaints suggestive of reflux symptoms were given the Reflux Symptom Index questionnaire and were asked to fill the questionnaire properly. If the Reflux Symptom Index score was more than 13, the patient fulfilled the study criteria. Then they were meticulously explained about the study in their own language, including risks /benefits, procedure, compliance with medication & lifestyle modification and need for follow up. All the queries generated were clarified. Only those who provided a voluntary written informed consent were enrolled in the study.
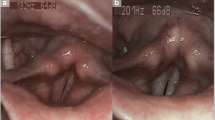
The enrolled patients underwent a detailed history and routine ENT examination, which was followed by Videolaryngostroboscopy (VLS). This was done using Storz make Pulser II model video stroboscope and Storz Telecam camera system (Fig. 1). Reflux Finding Score (RFS) was used to grade the VLS findings (Fig. 2). Then voice analysis was done using Dr. Speech software Version 5 (Dr Voice™ vocal assessment Tiger DRS, inc.) (Fig. 3). Fundamental frequency, jitter, shimmer, harmonic to noise ratio and maximum phonation time were the parameters documented in voice analysis.
These patients were advised for lifestyle modifications and proton pump inhibitors for 8 weeks. They underwent follow-up after 8 weeks. A non randomised dosage schedule of Rabeprazole 20 mg twice daily or Omeprazole 20 mg twice a day or Pantoprazole 40 mg twice a day were the proton pump inhibitors used in the present study.
At the 8 weeks follow-up RSI, videolaryngostroboscopy and voice analysis was performed again and the post treatment parameters noted. Patients were asked to report their compliance of lifestyle modifications as an affirmative or a negative response.
Data Collection Method
A customised proforma was designed for the specific requirement of the study. All relevant information was collected in this proforma.
Outcome Measures
Reflux symptom index, Reflux finding score and voice analysis were the outcome measures.
Follow-Up
All the enrolled patients were followed-up after 8 weeks.
Tools Used in the Present Study.
We had used Reflux Symptoms Index (RSI) (Table 1) and Reflux Finding Score (RFS) (Table 1) and Voice analysis which are pre-validated and have been used by other studies.
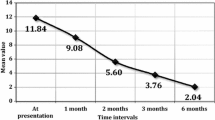
Results
We had included 100 patients suffering from laryngopharyngeal reflux disease (LPRD). Majority of the patients were in the age group 41–60 years with a mean age of 44.14 ± 12.56 years. The age ranged from 18 to 75 years. Males were more compared to the females (Table 2). Lifestyle modification compliance was seen in 85% of the patients. Rabeprazole 20 mg was given as BD dose in 45 (45%) patients, Omeprazole 20 mg was given as BD dose in 42 (42%) patients and Pantoprazole 40 mg as BD dose in 13 (13%) patients. Both the Reflux Symptom Index (Table 3) and Reflux Finding Scores (Table 3) showed a significant improvement at the 8-week follow-up. Throat clearing, foreign body sensation and posterior commissure hypertrophy were the most common symptoms seen. The comparisons of pretreatment and posttreatment Reflux Symptom Index (RFI) parameters was done. We found a significant association for hoarseness (P = 0.001), throat clearing (P = 0.001), postnasal discharge (P = 0.001), difficulty in swallowing (P = 0.001), coughing after food / lying down (P = 0.001), breathing difficulty (P = 0.001), annoying cough (P = 0.001), foreign body sensation (P = 0.001) and heart burn (P = 0.001). The comparisons of pretreatment and posttreatment Reflux Finding Score Index (RFS) parameters was done. We found a significant association for erythema (P = 0.001), vocal fold edema (P = 0.001), posterior commissure hypertrophy (P = 0.005), thick endolaryngeal mucus (P = 0.004), while no significant association was seen for granulation (P = 0.075). All the patients on medical therapy irrespective of life style modifications improved both in RSI and RFS after treatment. In our study, we found a statistically significant improvement in both RSI and RFS in patients who were compliant (Table 4) and also those who were not compliant with lifestyle modifications (Table 4). Moreover the mean improvement in RSI & RFS parameters was more in patients who complied with lifestyle modifications. Post treatment improvement in voice analysis showed a significant association (P = 0.001) for fundamental frequency (Table 5), jitter (Table 5), shimmer (Table 5), harmonic-to-noise ratio (Table 5) and maximum phonation time (Table 5). All 100 patients had taken PPI but only 85 had followed lifestyle modifications. Significant association (P = 0.001) was seen between lifestyle modification and posttreatment fundamental frequency (Table 6), posttreatment shimmer (Table 6) and post treatment harmonic-to-noise ratio (Table 6). There was no significant association between lifestyle modification and posttreatment jitter (Table 6) (P = 0.391) and posttreatment maximum phonation time (Table 6) (P = 0.248).
15 patients did not follow life style modifications. Out of these, in 10 patients voice analysis parameters had deteriorated at follow up.
Discussion
In the present study, we had included 100 consenting patients with complaints suggestive of reflux symptoms and having Reflux Symptom Index more than 13.
RSI scoring, VLS and voice analysis was done in each patient at presentation and 8 weeks post therapy.
Majority of the patients were in the age group 41–60 years with a mean age of 44.14 ± 12.56 years. The youngest patient was 18 years old and the oldest patient was 75 years old. The mean age of the patients in the Belafksy et al. (2001) [10] cohort was 50 ± 12 years, which is slightly higher than our study mean age.
Our study showed a male predominance with a male: female ratio of 1.32: 1. Similarly in the study done by Kaushik et al. [19] male predominance noted with a male to female ratio 1.28:1. In contrast Patigaroo et al. [20] had more females with a male to female ratio of 1:1.32. While in contrast with Patigaroo’s study our study findings concur with Kaushik’s observation.
A statistically significant improvements in mean RSI and RFS were seen after 2 months of treatment. Rabeprazole, Omeprazole and Pantoprazole were the proton pump inhibitors used in the present study. The selection of proton pump inhibitors was as per the individual choice of the treating consultant and the groups so formed was not randomised. Rabeprazole was most commonly administered. Bhargava et al. [21] study demonstrated highest improvement in laryngeal symptoms and laryngeal findings after treatment for 3 months with Omeprazole 20 mg BD. Lam et al. [22] in their study compared Rabeprazole (20 mg, BD) and placebo for 12 weeks in the treatment of laryngopharyngeal reflux. They found statistically significant improvement in RSI scores in treatment group, while there was no significant improvement in RFS scores in the treatment group, compared to the placebo group. They concluded that Rabeprazole significantly improves the reflux symptoms. Belafsky et al. [10] in their study also showed a significant improvement in mean RFI and RFS score after the treatment in patients with LPRD. This improvement is seen at 2 months, 4 months, and 6 months of treatment. We documented a single follow up at 2 months. Unlike Lam who had only improvement in RSI scores, our study showed improvement of both RSI & RFS scores like Belafskys study.
RSI
Our study registered pretreatment throat clearing in 91%, foreign body sensation in 91%, heart burn in 79% patients, hoarseness in 69% patients, postnasal discharge in 59%, coughing after food / lying down in 58%, difficulty in swallowing in 43%, annoying cough in 29% and breathing difficulty in 26%. Throat clearing and foreign body sensation were the most common symptoms. In their study of RSI, Mishra et al. [2] noted the most common symptom to be heartburn(44.5%) followed by frequent clearing of throat (38.8%) and sticky sensation in throat (32%).
In our study the comparisons of pretreatment and posttreatment Reflux Symptom Index (RSI) parameters were done. Improvement in foreign body sensation was seen in 89% patients, postnasal discharge in 79.7% patients, heart burn in 68.4% patients, throat clearing in 67% patients, hoarseness in 60.9% patients, difficulty in swallowing in 53.5%, annoying cough in 51.7% breathing difficulty in 46.2% patients and patients coughing after food / lying down in 43.1% patients. Overall, all the parameters of RFI showed statistically significant improvement after treatment (all P values = 0.001).
RFS
Pretreatment posterior commissure hypertrophy was seen in 92%, erythema in 18% patients, vocal fold edema in 11%, granulation in 11%, thick endolaryngeal mucus in 8% and diffuse laryngeal edema in 1%. Posterior commissure hypertrophy was the most common sign seen in our study.
The comparisons of pretreatment and posttreatment Reflux Finding Score Index (RFS) parameters was done. We found a significant association for erythema (P = 0.001), vocal fold edema (P = 0.001), posterior commissure hypertrophy (P = 0.005), thick endolaryngeal mucus (P = 0.004), while no statistically significant association was seen for granulation (P = 0.075).
In our study no patient had subglottic edema or ventricular obliteration either pre or post therapy. Post therapy vocal fold edema improvement was seen in 10 out of 11 (90.9%) patients. 1 patient had diffuse laryngeal edema before treatment, which resolved after treatment. Posttreatment posterior commissure hypertrophy improvement was seen in 45 out of 92 (48.9%) patients. Improvement in thick endolaryngeal mucus was seen in 7 out of 8 (87.5%) patients. Similarly erythema improvement was seen in 13 out of 18 (72.2%) patients. Granulation improvement was seen in 10 out of 11 (90.9%) patients.
Osman et al. [23] in their study found erythema in 88.52% and breathing difficulties in 34.43% to be the most common symptoms. Partial ventricular obliteration, mild vocal cord edema, mild laryngeal edema and persistence of granuloma were still detected 6 months post regular acid suppression therapy. In our study, the incidence of both erythema and breathing difficulty was less in comparison to the findings of Osman. We did not find any case of ventricular obliteration. While in all patients post treatment RFS score was decreased but still in some patients the individual RFS parameters of erythema, vocal cord edema, posterior commissure hypertrophy, granulation, thick endolaryngeal mucus persisted.
A study done by Lechien et al. [24] showed a significant improvement in RSI, RFS, VHI, jitter and shimmer parameters after 3 months of treatment (P < 0.05), which supports our study findings. In our study we also found much improvement in harmonic-to-noise ratio. In almost all cases, patients having pre-treatment normal voice parameters continued with normal voice parameters post treatment.
In our study, we found a statistically significant improvement in both RSI and RFS in patients who were compliant as well as those were not compliant with lifestyle modifications. However, the mean improvement in these two parameters was more in patients who complied with lifestyle modifications. A study done by Nanda et al. [25] showed a significant improvement in the reflux symptoms in the study group which followed lifestyle modification, compared to those who did not follow lifestyle modification (P < 0.05). They concluded lifestyle modification along with proton pump inhibitor treatment can be an effective treatment in patients with laryngopharyngeal reflux disease. We also found improvement in RSI and RFS parameters who followed proper lifestyle modification.
In a study done by Jin et al. [26], laryngopharyngeal reflux patients were treated medically for 5 months. RSI and RFS were documented at pretreatment and at the 2nd, 4th, 8th, 12th, 16th and 20th week posttreatment. Posttreatment analysis showed a significant improvement in jitter, shimmer and harmonic-to-noise ratio after 1–2 months and this improvement persisted to 3–4 months after treatment. In our study LPRD patients were treated with lifestyle modifications and drugs for 2 months. RSI and RFS were documented at pretreatment and 8th week posttreatment. Posttreatment analysis showed a significant improvement in jitter, shimmer and harmonic-to-noise ratio in all patients.
Conclusions
The gold standard of diagnosis of LPRD is 24 h pH monitoring but has many false negatives and false positives due to intermittent reflux and inaccurate probe placement. This costly, time consuming and invasive procedure is not widely available amongst our speciality.
RSI is a questionnaire while VLS and Voice analysis are non-invasive procedures. The present study was undertaken to compare Laryngopharyngeal Reflux Disease (LPRD) pre and posttreatment using non invasive tools of reflux symptom index(RSI), videolaryngostroboscopy and voice analysis.
We have graded features of LPRD by RFS. Our study shows that videolaryngostroboscopy is an excellent modality for the assessment of laryngopharyngeal reflux disease (LPRD). It allows exceptional visualization for grading of RFS parameters. Abnormal parameters in voice analysis helps in early diagnosis of hoarseness associated with LPRD patients even before it becomes clinically significant. Voice analysis also documents the treatment outcome. We conclude that an 8-week proton pump inhibitor treatment combined with lifestyle modification resulted in a significant improvement as detected in RSI and RFS and voice analysis parameters.
Availability of Data and Materials
Data collected from medical records department and data transparency maintained.
Code Availability
Not applicable.
References
Campagnolo AM, Priston J, Thoen RH, Medeiros T, Assunção AR (2014) Laryngopharyngeal reflux: diagnosis, treatment, and latest research. Int Arch Otorhinolaryngol 18(2):184–191. https://doi.org/10.1055/s-0033-1352504. (PMID25992088, PMCIDPMC4297018)
Mishra P, Agrawal D, Chauhan K, Kaushik M (2020) Prevalence of laryngopharyngeal reflux disease in Indian population. Indian J Otolaryngol Head Neck Surg 20:1–5. https://doi.org/10.1007/s12070-020-01882-1
Durazzo M, Lupi G, Cicerchia F, Ferro A, Barutta F, Beccuti G et al (2020) Extra-esophageal presentation of gastroesophageal reflux disease: 2020 update. J Clin Med 9(8):2559. https://doi.org/10.3390/jcm9082559. (PMID32784573, PMCIDPMC7465150)
Lechien JR, Huet K, Khalife M, Fourneau AF, Delvaux V, Piccaluga M, Harmegnies B, Saussez S (2016) Impact of laryngopharyngeal reflux on subjective and objective voice assessments: a prospective study. J Otolaryngol-Head & Surg 45(1):1–9
Gaude GS (2009) Pulmonary manifestations of gastroesophageal reflux disease. Ann Thorac Med 4(3):115–123. https://doi.org/10.4103/1817-1737.53347. (PMID: 19641641; PMCID: PMC2714564)
Mishra P, Agrawal D, Artham P (2020) Screening test for LPRD: history versus video laryngoscopy. Indian J Otolaryngol Head Neck Surg 72(4):422–427. https://doi.org/10.1007/s12070-020-01828-7. (PMID33088769, PMCIDPMC754479)
Argyrou A, Legaki E, Koutserimpas C, Gazouli M, Papaconstantinou I, Gkiokas G, Karamanolis G (2018) Risk factors for gastroesophageal reflux disease and analysis of genetic contributors. World J Clin Cases 6(8):176–182. https://doi.org/10.12998/wjcc.v6.i8.176. (PMID:30148145; PMCID:PMC6107529)
Belafsky PC, Postma GN, Koufman JA (2002) Validity and reliability of the reflux symptom index (RSI). J Voice 16(2):274–277. https://doi.org/10.1016/s0892-1997(02)00097-8. (PMID: 12150380)
Jetté ME, Gaumnitz EA, Birchall MA, Welham NV, Thibeault SL (2014) Correlation between Reflux and multichannel intraluminal impedance pH monitoring in untreated volunteers. Laryngoscope 124(10):2345–2351. https://doi.org/10.1002/lary.24737. (PMID 24782404)
Belafsky PC, Postma GN, Koufman JA (2001) The validity and reliability of the reflux finding score (RFS). Laryngoscope 111(8):1313–1317. https://doi.org/10.1097/00005537-200108000-00001. (PMID 11568561)
Mehta DD, Hillman RE (2008) Voice assessment: updates on perceptual, acoustic, aerodynamic, and endoscopic imaging methods. Curr Opin Otolaryngol Head Neck Surg 16(3):211–215. https://doi.org/10.1097/MOO.0b013e3282fe96ce. (PMID 18475073, PMCIDPMC3775647)
Naufel de Felippe AC, Grillo MH, Grechi TH. Standardization of acoustic measures for normal voice patterns. Braz J Otorhinolaryngol. 2006;72(5):659–64. doi: https://doi.org/10.1016/s1808-8694(15)31023-5, PMID 17221059.
Dr. Speech. Tiger DRS, Inc [software] [cited 20.6.2021]. Available from: http://www.drspeech.com/product.
Visi-Pitch IV [cited 2.6.2021]. Available from: http://aimtech.ru/en/catalog/99.
Computerized speech lab CSL [cited 2.6.2021]. Available from: https://www.pentaxmedical.com/pentax/en/99/1/Computerized-Speech-Lab-CSL.
VAGMI [cited 2.6.2021]. Available from: https://www.vagmionline.com/.
Batıoğlu-Karaaltın A, Develioğlu ÖN, Tarhan Ö, Külekçi M (2016) The importance of voice analysis in evaluating the effectiveness of reflux treatment. Kulak Burun Bogaz Ihtis Derg 26(4):207–212. https://doi.org/10.5606/kbbihtisas.2016.80688. (PMID 27405075)
Kahrilas PJ, Shaheen NJ, Vaezi MF et al (2008) American Gastroenterological Association Medical Position Statement on the management of gastroesophageal reflux disease. Gastroenterology 135(4):1383–1391. https://doi.org/10.1053/j.gastro.2008.08.045. (PMID 18789939)
Kaushik MR, Kole AS, Gupta N, Dhoot S, Dehadaray A (2018) Evaluation of various laryngeal pathologies: videolaryngoscopy versus videolaryngostroboscopy. Indian J Otolaryngol Head Neck Surg 70(2):244–248. https://doi.org/10.1007/s12070-017-1115-4. (PMID 29977849, PMCID PMC6015562)
Patigaroo SA, Dar NH, Shafi OM, Qazi SM (2018) Treating laryngopharyngeal reflux with proton-pump inhibitors-An observational study. Int J Med Sci Public Health 8(2):150–155. https://doi.org/10.5455/ijmsph.2019.1132822122018
Bhargava A, Faiz SM, Srivastava MR, Shakeel M, Singh NJ (2019) Role of proton pump inhibitors in laryngopharyngeal reflux: clinical evaluation in a North Indian population. Indian J Otolaryngol Head Neck Surg 71(3):371–377. https://doi.org/10.1007/s12070-018-1493-2. (PMID 31559206, PMCIDPM)
Lam PK, Ng ML, Cheung TK, Wong BY, Tan VP, Fong DY et al (2010) Rabeprazole is effective in treating laryngopharyngeal reflux in a randomized placebo-controlled trial. Clin Gastroenterol Hepatol 8(9):770–776. https://doi.org/10.1016/j.cgh.2010.03.009. (PMID20303417)
Osman AH, Abd Elrhman HN, Shafy AM (2019) The efficacy of PPI in the treatment of laryngopharyngeal reflux. J Gastroenterol Hepatol Research 8(1):2800–2806. https://doi.org/10.17554/j.issn.2224-3992.2019.07.803
Lechien JR, Finck C, Huet K, Fourneau AF, Khalife M, Delvaux V et al (2020) Voice Quality as therapeutic outcome in laryngopharyngeal reflux disease: a prospective cohort study. J Voice 34(1):112–120. https://doi.org/10.1016/j.jvoice.2018.08.018. (PMID30220528)
Nanda MS (2016) Role of adjuvant lifestyle modifications in patients with laryngopharyngeal reflux disease in hilly areas. Int J Sci Study 3(10):114–118
Jin BJ, Lee YS, Jeong SW, Jeong JH, Lee SH, Tae K (2008) Change of acoustic parameters before and after treatment in laryngopharyngeal reflux patients. Laryngoscope 18(5):938–941. https://doi.org/10.1097/MLG.0b013e3181651c3a
Funding
Not applicable.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors hereby declare that there are no potential conflicts of interest with respect to research and publication of this article.
Ethical Approval
Done.
Human and Animal Rights
Not applicable.
Informed consent
Taken.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Suda, A., Sikdar, A., Nivsarkar, S. et al. Reflux Symptom Index (RSI), Videolaryngostroboscopy and Voice Analysis: A Triad of Non-Invasive Tools to Study Treatment Outcomes of Laryngopharyngeal Reflux Disease (LPRD). Indian J Otolaryngol Head Neck Surg 76, 250–261 (2024). https://doi.org/10.1007/s12070-023-04136-y
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12070-023-04136-y