Abstract
Aims
Being an important prognostic predictor in carcinoma oral tongue, neck metastasis poses an adverse impact on prognosis.The management of neck is still controversial. Neck metastasis depends on features like tumor thickness, depth of invasion, lymphovascular invasion and perineural invasion. Thus by correlating these features with the level of nodal metastasis and by correlating clinical and pathological staging, a preoperative assumption for a more conservative neck dissection may be done.
Objectives
-
1.
To correlate clinical staging, pathological staging and depth of invasion (DOI) of tumor with cervical nodal metastasis, for a preoperative assumption of a more conservative neck dissection.
-
2.
To study the correlation of additional prognostic features like lymphovascular invasion, perineural invasion, positive resection margin, worst pattern of invasion, lymphocytic infiltration and presence of necrosis with that of cervical nodal metastasis.
Materials and Methods
The study was conducted on 24 patients of carcinoma oral tongue who underwent resection of the primary with an appropriate neck dissection and their clinical, imaging, and postoperative histopathological findings were correlated.
Results
We found a significant association of the CC (craniocaudal) dimension and radiologically determined DOI (depth of invasion) with the pN also significant association of clinical and radiological DOI with histological DOI. The probability of occult metastasis was found to be more when the MRI-DOI is > 5 mm. The sensitivity and specificity of cN staging were 66.67% and 73.33% respectively. The accuracy of cN was 70.8%.
Conclusion
In the present study a good sensitivity, specificity and accuracy of cN (clinical nodal stage) was found. Craniocaudal (CC) dimension and DOI of the primary tumor measured by MRI is a strong predictor of the disease extension and nodal metastasis. MRI-DOI > 5 mm warrants an elective neck dissection of level I-III. For tumors MRI DOI < 5 mm observation can be recommended with adherence to a strict follow-up.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Cancer is the second leading cause of death globally, of which 70% occurs in low and middle income countries. The oral carcinoma occurs in the sub sites of oral cavity that includes the mucosal lip, buccal mucosa, oral tongue (anterior two thirds), floor of mouth, upper and lower alveolus, hard palate and retromolar trigone.
In the Western world, oral cancer is relatively uncommon and the incidence in North America and Europe is 7.6% and 17.6% respectively and that in Asia it is 64.2%. Likewise the mortality is 2.9% and 13.6% in North America and Europe respectively but 73.3% in Asia. Oral cancer ranks 11th in the overall incidence for the most common cancer in Asia but 2nd in India and first among Indian males. The reason being, the predominant use of tobacco, alcohol and betel quid in this region [1, 2]
The Oral Squamous Cell Carcinoma spreads mostly by lymphatics. The absence of fascial planes between the intrinsic & extrinsic muscles enables tumors to easily penetrate and infiltrate among the various muscles. Tongue has shown higher risk of cervical nodal metastasis as compared to other subsite as a result of abundant lymphatics. Cervical nodal metastasis being an important feature poses an adverse impact on prognosis.
Early stage of carcinoma oral cavity is treated surgically, directed at controlling the primary tumor and regional neck metastases, by wide excision of primary site and elective neck dissection. Primary site excision and therapeutic neck dissection with additional CRT (chemoradiotherapy) is considered if patients have advanced cancers. Clinical staging by the corroboration of physica lexamination and imaging studies plays a vital role in proposing the treatment modality which includes surgery of primary ± neck dissection ± CRT.
In the management of neck, most school of thoughts are towards an elective neck dissection as an important component of carcinoma tongue management, due to the presence of occult metastasis, for N0 disease [3,4,5,6]. Contrary to that, other school believes that elective neck dissection done in early stage is more of an over treatment [7, 8]. The management of N1 & N2 disease is either by selective neck dissection or modified radical neck dissection and N3 by modified radical or radical neck dissection followed by adjuvant CRT. By finding the relation of tumor thickness, DOI and few other features with lymph nodal involvement the risk of neck metastasis can be predicted, thus contributing to a better therapeutic decision making.
Materials and Methods
The study was conducted at our institute for a period of 1.5 years from February 2019 to July 2020, after obtaining the ethical committee clearance. All patients above the age of 18 years, histologically proven to have carcinoma of the oral tongue with positive/negative clinical lymph nodes and previously untreated were included in the study. Patients not willing to give an informed consent; non squamous cell carcinoma; with distant metastasis; having had prior treatment by surgery/radiotherapy/chemotherapy and unfit to undergo general anesthesia were excluded from the study. After getting an informed consent, complete history was taken and a thorough clinical examination was performed with emphasis on site, size and extent of involvement of lymph nodes. All patients were subjected to MRI with contrast, where the details of primary tumor thickness, volume, DOI, levels and status of lymph nodes involved, were obtained. Surgery in the form of wide local excision/hemiglossectomy/near-total glossectomy with or without reconstruction of the primary and an appropriate neck dissection was done. Post-Operatively the specimens of the primary and neck dissection were labeled and sent for histopathologic examination. The histopathological assessment included:
(I) Primary tumor.
-
a.
Tumor size.
-
b.
Depth of Invasion (DOI).
-
c.
Histological subtype.
-
d.
Histological grade.
-
e.
Lymphovascular invasion.
-
f.
Perineural invasion.
-
g.
Lymphocytic infiltration into the surrounding tissue (peritumoral or intratumoral).
-
h.
Presence or absence of necrosis.
-
i.
Positive margin.
(II) LN status.
-
a.
No. of LNs resected.
-
b.
No. of LNs metastasized.
-
c.
Extranodal deposits.
The reports were then collected and assessed with the pre-operative findings.
Analysis
The study subjects were described according to their demographic variables in terms of mean and percentage. As data was not normally distributed Mann–Whitney U test was used to compare the variables. The relationship between two categorical variables are given by the chi-square test with P-value < 0.05 to be significant. Characteristic of cN diagnosis described by Sensitivity, Specificity, Positive predictive value (PPV) and Negative predictive value (NPV). The statistical package used was IBM SPSS version 23.
Results
The patients in the study group were mostly in the fifth decade of life. Only one patient presented at the age of 30 and one above the age of 70 years. The male female ratio was 2:1. 54% patients were presented at 3–6 months of onset of their symptoms. Almost all patients had the lesion on the lateral border of the tongue, most of which were in the mid-lateral region (58.33%).
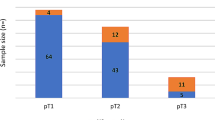
In the present study, T2 was the commonest T-stage in both clinical and histopathological staging. In clinical staging T3 were more than T1 whereas histopathologically T1 and T2 were more than T3. There was no T4 stage in either group. Majority of the patients had no identifiable neck nodes both clinically and histopathologically, followed by N1 and N2 (Table 1).
Among the cervical lymph nodes the most commonly involved was level I clinically whereas it was level II histopathologically (Table 2). Involvement of level IV and V were not seen both clinically and in histopathology.
There was a significant association of CC dimension with the lymphnodes with P-value <0.05[0.059] and Z-value - 1.886 (Table 3). Other two dimension, that is AP and TR had no significant association with the lymph nodes with P-value >0.05.
There was significant association between pathological depth of invasion and radiological depth of invasion with P-value <0.05 (Table 4).
The positive predictive value of clinical lymph node is 81.82% when the MRI-DOI is more than 5 mm and is only 66.67% when less than 5 mm (Table 5). The probability of occult metastasis is more when the MRI-DOI is >5 mm (stage II). The rate of occult metastasis among cN in the present study was found to be 21.43%.
There was significant association between pTNM staging and cTNM staging with P-Value <0.05 (Table 6).
Of the 10 necks found clinically positive, 6 were true positive while 4 were false positive. Out of the 14 neck found clinically negative, 11 patients were true negative while 3 patients were false negative. The sensitivity of clinical examination was found to be 66.67%, specificity was found to be 73.33%, positive predictive value 60% and negative predictive value 78.5% (Table 7). Accuracy of clinical examination was 70.8%.
There was significant association between LVI and nodal metastasis with P-value < 0.05. Two patients who had lymphovascular invasion had pathological nodal metastasis.
There was no significant association between the resected margin and locoregional recurrence with P-value > 0.05.
Discussion
The majority of patients with carcinoma of the oral tongue present with stage I/II disease. It mostly spreads by lymphatics and is the important prognostic factor. Nodal involvement guides the treatment of oral carcinoma and neck dissection. The incorporation of the feature of depth of invasion in the new 8th edition AJCC staging system helps in knowing the extent of the primary as well as the probability of occult metastasis, which helps us in planning a more conservative type of neck dissection if possible. In-depth, post-operative pathological assessment about the DOI, resected margin, LVI (lymphovascular invasion) and PNI (perineurial invasion) helps us in assessing the outcome and prognosis and in planning subsequent treatment.
Distribution of Patients by cTNM and pTNM Stage
In the present study, most patients 79.17% had cT2 stage, followed by T3 (12.5%) and T1 (8.33%). This is similar to the study done by Krishnamurthy et al., where they found an increased percentage of early stage tongue carcinoma [9]. This is contrast to the base of tongue carcinoma probably due to the early symptomatology in case of anterior tongue carcinoma. Of the 24 patients, 14(58.33%) of the patients were clinically node negative. 7(29.17%) patients were in cN1 and 3(12.5%) patients were in cN2 stage.
Out of the 24 patients, most of the patients 13(54.17%) were staged as pT2 post-operatively, followed by pT1- 9(37.5%) patients and pT3-2(8.33%) patients. 15(62.5%) patients had no pathological cervical nodal metastasis. 6(25%) patients were in pN1 stage, 2(8.33%) patients were in pN2 stage and 1(4.17%) patient was in pN3 stage. Level II lymph nodes were the most common followed by level I and III.
Association of Tumor Thickness (AP*TR*CC) and Tumor Volume with pN
The tumor thickness is the greatest dimensions along the anteroposterior (AP), transverse (TR) and craniocaudal (CC) planes obtained by pre-operative CE-MRI. Tumor volume was then estimated based on these measurements of maximum tumor diameter in the 3 planes. Jayasankaran et al. in his study has showed that only CC dimension has significant correlation with pathological nodal involvement with P < 0.03 [10]. The present study showed a similar association with the CC dimension and the pN, with P-value < 0.05. Study done by Hu et al. shows tumor thickness was useful in predicting lymph node metastasis while tumor volume did not [11] which is similar to the present study. This is probably because the maximum resistance for tumor growth is in the vertical plane and so logically an aggressive tumor has to be the one with higher vertical involvement.
The Association of Clinical, Radiological and Pathological Depth of Invasion with pN
The 8th edition of AJCC guidelines of cancer staging has incorporated depth of invasion as a criterion which seems to be an important predictor of tumor invasiveness and lymph node metastasis [12]. It is measured clinically by palpation, in radiology (MRI) by finding the horizon of the adjacent normal mucosa and the line drawn perpendicular to the deepest point of the tumor and pathologically with micrometers. As physical examination often under-estimates the cancer burden, imaging was considered for assessment. Vidiri et al. in their study recommends measurement of MRI-DOI in pretreatment assessment as it showed good correlation with histopathological-DOI [13]. Huopainen et al. showed similar correlation [14]. In the present study we found significant association of pathological DOI with clinical and radiological DOI with P-value < 0.05. Also the radiological and pathological DOI had significant association with pN with P-value < 0.05. Xu C et al. showed that the optimal cutoff value of MRI-determined DOI was 7.5 mm for predicting neck lymph node metastasis, with a sensitivity of 86.9% [15]. In the present study we grouped patients according to the AJCC cut off points of < 5 mm, > 5 to < 10 mm and > 10 mm and our study shows a positive predictive value of cN of 81.82% when the radiological-DOI is more than 5 mm. The probability of occult metastasis was found to be more when the radiological-DOI is > 5 mm, which shows that radiology serves as a great tool to predict nodal metastasis pre-operatively.
The Association of Clinical with Pathological Stage and Characteristic of cN Diagnosis
There was significant association between cTNM and pTNM with a P-value < 0.05, in the present study. In view of neck dissection cN stage’s sensitivity and specificity has been assessed. Physical examination is the mainstay of staging the neck and is sometimes inaccurate. Palpability of node depends upon its location and consistency. In a neck of average size, approximately 0.5 cm in the superficial areas and l cm in the deeper areas can be palpated. Persons with short neck or muscular neck pose difficulty in accurate examination of the neck. Hence radiology (in our case CE-MRI) is employed to improve the neck assessment preoperatively [16]. The study done by Woolgar et al. in 136 neck dissections had a sensitivity and specificity rates of 55% and 78%, respectively [17]. The present study had similar sensitivity and specificity of cN staging of 66.67%, and 73.33% respectively. The positive predictive value was 60% and negative predictive value was 78.5%. The accuracy of cN was 70.8%.
Associations of Prognostic Features
Other than the T, N and M stages for assessing prognosis, additional prognostic factors recommended by AJCC is degree of differentiation, extranodal extension (ENE), resected margin, worst pattern of invasion(WPOI), lymphovascular invasion (LVI) and perineural invasion (PNI) [12]. Viswanatha et al. says LVI and PNI are good predictors of nodal metastasis and are soft indicators for considering adjuvant / concurrent RT [18]. In the present study, we found a significant association of ENE, resected margin and LVI with pN with a P-value < 0.05. No significance was seen of degree of differentiation and pattern of invasion with pN with P-value > 0.05. And no patient had PNI. Other parameters like lymphocytic infiltration and presence of necrosis also had significant association with pN with P-value < 0.05. PNI, LVI, ENE, positive margin, lymphocytic infiltration have been associated with the risk of local recurrences and lymph node metastasis. The presence of these gives significant prognostic value which influences treatment decisions, recurrence and distant metastasis.
Management of Neck
The management of the neck in larger primary tumors is usually straightforward except when the neck is accessed for microvascular or pedicle flap reconstruction of the primary site. However if the probability of neck metastases is low, neck dissection simply acts as an overtreatment, where the morbidity of the neck procedure only offers a decrease in quality of life and functional deficits.
The cN1 & cN2 diseases are treated either by selective neck dissection or modified radical neck dissection and N3 by modified radical or radical neck dissection followed by adjuvant CRT.In view of occult metastasis which increases the incidence of distant metastasis; ease of neck dissection during primary surgery; low morbidity and mortality of SND; decreased detection of early conversion of neck nodes during follow up and prognosticate the disease with pN status, END is preferred for cN0 diseases. Many RCTs and meta-analysis has described the decrease in loco-regional recurrence, disease free survival rates and good prognosis in END. D’Cruzet al in a RCT of a total of 596 patients suggests that END at the time of resection of the primary tumor confers an overall survival benefit in patients with early-stage, clinically node-negative oral squamous-cell carcinoma [3]. In a systematic review and meta-analysis done by Abu-Ghanem et al., the findings suggest that END in cN0 neck significantly reduces the rate of regional nodal recurrence and improves disease-specific survival [4]. Similar conclusions were seen in few other meta-analysis [5, 6]
On the other hand with a careful clinical follow-up combined with imaging to detect early conversion from N0 to N1; removal of barrier to the spread of disease by END which has a detrimental immunological effect; causing a scarred and hypoxic field that reduce the effect of radiation; and the associated surgical morbidity, END is considered a overtreatment for cN0 disease. In a retrospective analysis done by Flach et al.in patients with early stage oral cancer and cN0 neck a 'wait and scan' policy using strict surveillance is justified as survival is not negatively influenced, avoiding unnecessary neck dissection and its accompanying morbidity [7]. Yuen AP et al.in their study says observation may be an acceptable alternative to END if strict adherence to a cancer surveillance protocol is followed [8].
The probability of occult as well as overt metastasis was found to be more when the MRI-DOI is > 5 mm. The positive predictive value of cN was 81.82% when the MRI-DOI is more than 5 mm. A retrospective study done by Brendan Liu et al.has showed the cut-off of 5 mm of DOI best predicted nodal disease [19]. In view of significant association between MRI-DOI, P-DOI and pN and a 70.8% accuracy of cN in our study, we suggest an END for a MRI-DOI > 5 mm. The CC dimension in MRI is to be considered for tumor staging as it is significantly associated with pN.
There still seems to be a debate of the extent of neck dissection to be performed. Tumors of the tongue initially metastasize to levels I and II, lateral tongue tumors frequently metastasizes directly to level II nodes. The echelon nodes for oral cavity are: levels I, II, III & occasionally level IV. Level V LN is rarely reported [20]. Woolgar et al.in their study says that the pattern of metastatic spread in tongue tumors has skip lesions and peppering that which indicates that level IV nodes must be included in staging and therapeutic neck dissections in tongue cancer [21]. In a retrospective study done by Paolo et al., documented a 7.4% instances of skip metastasis justifying the inclusion of level IV in neck dissection of N0 tongue cancers [22]. Whereas few studies shows that skip metastasis is very rare in T1 and T2 tumors and so inclusion of level IV is not mandatory [23, 24]. In the present study the most common involved node was level II followed by I and III and we did not come across skip metastasis or level IV node involvement. So in view of the above result of our study and the predictable pattern of lymph node metastasis we suggest a ND I-III for a tumor with MRI-DOI > 5 mm. For patients with MRI DOI < 5 mm with a strict follow up along with imaging surveillance we can opt for observation. But patient’s preference (weighing oncological outcome over morbidity and quality of life), follow-up, costs and institutional resource ought to be considered for optimizing treatment.
Conclusion
Cancer treatment is a complex multidisciplinary pursuit. Treatment is surgical resection of the primary tongue cancer with clear margins and the involved and at-risk cervical lymphatic basins (I-III). While overtreatment can result in functional and cosmetic defects, undertreatment can result in cancer recurrence.
In our study we saw a good sensitivity, specificity and accuracy of cN. Craniocaudal (CC) dimension of the tumor and DOI measured by MRI is a strong predictor of the disease extension and nodal metastasis. MRI-DOI > 5 mm warrants an elective neck dissection of levels I-III. For tumors MRI DOI < 5 mm observation can be recommended with adherence to a strict follow-up. Treatment should be optimized considering factors like personal preference of the patient, follow-up and institutional resource.
Other pathological parameters like positive resected margin, LVI, PNI, WPOI, lymphocytic infiltration and presence of necrosis are to be considered as a soft indicator for post-operative adjuvant therapy.
Regular follow-up visits should be emphasized for disease surveillance and management of treatment-related side effects. Thus the disease control can be achieved better and morbidity can be decreased.
References
Ferlay J, Ervik M, Lam F, Colombet M, Mery L, Piñeros M, Znaor A, Soerjomataram I, Bray F (2018). Global cancer observatory: cancer today. Lyon, france: international agency for research on cancer. https://gco.iarc.fr/today/data/factsheets/cancers/1-Lip-oral-cavity-fact-sheet.pdf
GLOBOCAN (2018) https://gco.iarc.fr/today/data/factsheets/populations/356-india-fact-sheets.pdf
Dcruz AK, Vaish R, Kapre N et al (2015) Head and neck disease management group elective versus therapeutic neck dissection in node-negative oral cancer. N Engl J Med. 373(6):521–9
Abu-Ghanem S, Yehuda M, Carmel Neiderman N, Leshno M, Abergel A, Gutfeld O, Fliss D (2016) Elective neck dissection vs observation in early-stage squamous cell carcinoma of the oral tongue with no clinically apparent lymph node metastasis in the neck: a systematic review and meta-analysis. JAMA Otolaryngol-Head Neck Surg. https://doi.org/10.1001/jamaoto.2016.1281
Ding Z, Xiao T, Huang J, Yuan Y, Ye Q, Xuan M, Xie H, Wang X (2019) Elective neck dissection versus observation in squamous cell carcinoma of oral cavity with clinically N0 neck: a systematic review and meta-analysis of prospective studies. J Oral Maxillofac Surg 77(1):184–194. https://doi.org/10.1016/j.joms.2018.08.007. (Epub 2018 Aug 22 PMID: 30218654)
Fasunla AJ, Greene BH, Timmesfeld N, Wiegand S, Werner JA, Sesterhenn AM (2011) A meta-analysis of the randomized controlled trials on elective neck dissection versus therapeutic neck dissection in oral cavity cancers with clinically node-negative neck. Oral Oncol. 47(5):320–4. https://doi.org/10.1016/j.oraloncology.2011.03.009
Flach GB, Tenhagen M, de Bree R, Brakenhoff RH, van der Waal I, Bloemena E, Kuik DJ, Castelijns JA, Leemans CR (2013) Outcome of patients with early stage oral cancer managed by an observation strategy towards the N0 neck using ultrasound guided fine needle aspiration cytology: No survival difference as compared to elective neck dissection. Oral Oncol 49(2):157–164. https://doi.org/10.1016/j.oraloncology.2012.08.006. (Epub 2012 Sep 8 PMID: 22967965)
Yuen AP, Ho CM, Chow TL, Tang LC, Cheung WY, Ng RW, Wei WI, Kong CK, Book KS, Yuen WC, Lam AK, Yuen NW, Trendell-Smith NJ, Chan YW, Wong BY, Li GK, Ho AC, Ho WK, Wong SY, Yao TJ (2009) Prospective randomized study of selective neck dissection versus observation for N0 neck of early tongue carcinoma. Head Neck 31(6):765–772. https://doi.org/10.1002/hed.21033. (PMID: 19408291)
Krishnamurthy A, Ramshankar V (2013) Early stage oral tongue cancer among non-tobacco users–an increasing trend observed in a South Indian patient population presenting at a single centre. Asian Pac J Cancer Prev 14(9):5061–5065. https://doi.org/10.7314/apjcp.2013.14.9.5061. (PMID: 24175776)
Jayasankaran SC, Chelakkot PG, Karippaliyil M, Thankappan K, Iyer S, Moorthy S (2017) Magnetic resonance imaging: A predictor of pathological tumor dimensions in carcinoma of anterior twothirds of tongue – A prospective evaluation. Indian J Cancer 54:508–513
Hu H, Cheng K-L, Xu X-Q, Wu F-Y, Tyan Y-S, Tsai C-H, Shen C-Y (2015) Predicting the prognosis of oral tongue carcinoma using a simple quantitative measurement based on preoperative MR imaging: tumor thickness versus tumor volume. Am J Neuroradiol 36(7):1338–1342. https://doi.org/10.3174/ajnr.A4278
Amin MB, Edge SB, Greene FL et al (eds) (2017) AJCC cancer staging manual, 8th edn. Springer, New York
Vidiri A, Panfili M, Boellis A et al (2020) The role of MRI-derived depth of invasion in staging oral tongue squamous cell carcinoma: inter-reader and radiological–pathological agreement. Acta Radiol 61(3):344–352. https://doi.org/10.1177/0284185119862946
Huopainen P, LauriJouhi JH, Apajalahti S (2020) MRI correlates to histopathological data in oral tongue squamous cell carcinoma diagnostics. Acta Odontol Scand. https://doi.org/10.1080/00016357.2020.1789736
Xu C, Yuan J, Kang L, Zhang X, Wang L, Chen X, Yao Q, Li H (2020) Significance of depth of invasion determined by MRI in cT1N0 tongue squamous cell carcinoma. Sci Rep 10(1):4695. https://doi.org/10.1038/s41598-020-61474-5.PMID:32170092;PMCID:PMC7070144
Nithya C, Pandey M, Naik B, Ahamed IM (2003) Patterns of cervical metastasis from carcinoma of the oral tongue. World J Surg Oncol. 1(1):10. https://doi.org/10.1186/1477-7819-1-10
Woolgar JA, Beirne JC, Vaughan ED, Lewis-Jones HG, Scott J, Brown JS (1995) Correlation of histopathologic findings with clinical and radiologic assessments of cervical lymph-node metastases in oral cancer. Int J Oral Maxillofac Surg. 24(1 Pt 1):30–7. https://doi.org/10.1016/s0901-5027(05)80853-7
Viswanatha SC, Hedne N, Hasan S (2018) Correlation between histological grading LVI and PNI of carcinoma oral tongue to lymph node metastasis. Int J Otorhinolaryngol Head Neck Surg 5(1):159–164. https://doi.org/10.18203/issn.2454-5929.ijohns20185306
Liu B, Amaratunga R, Veness M et al (2020) Tumor depth of invasion versus tumor thickness in guiding regional nodal treatment in early oral tongue squamous cell carcinoma. Oral Surg Oral Med Oral Pathol Oral Radiol 129(1):45–50. https://doi.org/10.1016/j.oooo.2019.08.002
Parikh DG, Chheda YP, Shah SV, Patel AM, Sharma MR (2013) Significance of level v lymph node dissection in clinically node positive oral cavity squamous cell carcinoma and evaluation of potential risk factors for level v lymph node metastasis. Indian J Surg Oncol 4(3):275–279. https://doi.org/10.1007/s13193-013-0241-z
Woolgar JA (1999) Histological distribution of cervical lymph node metastases from intraoral/oropharyngeal squamous cell carcinomas. Br J Oral Maxillofac Surg 37:175–180
Cariati P (2018) Almudena cabello serrano, jose fernandez solis, ildefonso martinez lara, distribution of cervical metastasis in tongue cancer: are occult metastases predictable? A retrospective study of 117 oral tongue carcinomas. J Cranio-Maxillofacial Surg 46(1):155–161
Dogan E, Cetinayak O, Sarioglu S, Erdag T, Ikiz A (2014) Patterns of cervical lymph node metastases in oral tongue squamous cell carcinoma: Implications for elective and therapeutic neck dissection. J Laryngol Otol. 128:1–6. https://doi.org/10.1017/S0022215114000267
Balasubramanian D, Thankappan K, Battoo A, Rajapurkar M, Kuriakose M, Iyer S (2012) Isolated Skip Nodal Metastasis Is Rare in T1 and T2 Oral Tongue Squamous Cell Carcinoma. Otolaryngol-Head Neck Surg Official J Am Academy Otolaryngol-Head Neck Surg. 147:275–7. https://doi.org/10.1177/0194599812439664
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflicts of interest
There are no conflicts of interest.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Kubendiran, N.M., Sen, S. & Saha, S. A Clinicopathological Evaluation of the Correlation of Carcinoma Oral Tongue (Anterior Two Thirds) with Cervical Nodal Metastasis to Assess the Level of Neck Dissection: A Hospital Based Prospective Study. Indian J Otolaryngol Head Neck Surg 75, 80–87 (2023). https://doi.org/10.1007/s12070-023-03523-9
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12070-023-03523-9