Abstract
A retrospective study was conducted at a tertiary ENT care hospital with following aims, methodology and results: (1) To know the incidence of tympanosclerosis. (2) To classify tympanosclerosis surgically as well as histologically. (3) To know the long term hearing outcome of Tympanosclerosis surgery. It is a retrospective study at an ENT Hospital Centre in eastern India. Hospital ethical board clearance was duly obtained. All cases of tympanosclerosis were documented with special reference to surgical procedure, areas of involvement and postoperative hearing outcome. In this study, 90 cases of tympanosclerosis was found in 1880 cases of tympanomastoidectomies in 8 years and had been divided into (1) Myringosclerosis (60 cases, 66.6%), (2) Ossicular Tympanosclerosis without involvement of footplate (23 cases, 25.6%), (3) Ossicular Tympanosclerosis with involvement of footplate (7 cases, 7.8%). Treatment options included osssicular mobilization keeping ossicular integrity and mobility, Total or partial ossicular prosthesis after removal of incus & stapes suprastructure, stapedectomy with Long malleus-footplate piston. Overall good hearing outcome (i.e., postoperative air–bone gap less than 20 dB) was noticed in 85.5% of cases of Tympanosclerosis. Removal of tympanosclerosis with keeping the osssicular chain intact is the key to success; results are not favourable if footplate is totally fixed with disease.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Tympanosclerosis accounts for 4–5% of all cases of chronic otitis media. Myringosclerosis, i.e., Tympanosclerosis of lamina propia of pars tensa is the most common variant whereas footplate Tympanosclerosis is the most difficult to deal. Removal of all TS tissues without compromising ossicular integrity and mobility remain the main key for treatment.
Materials and Methods
This was a retrospective study done at ENT tertiary care hospital in eastern India. All cases of tympanosclerosis were documented in respect to clinical grade of tympanosclerosis, surgical procedure used, histopthological type and postoperative hearing outcome.
Operative Procedure
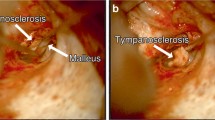
To diagnose a case of TS high level of suspicion is needed especially in cases of small central perforation with disproportionately high ABG, sometimes TS plaques are also seen at malleus handle region. Otoendoscopy before surgery is also helpful to diagnose TS preoperatively (Fig. 1—showing different types of tympanosclerosis in preoperative Otoendoscopy).
In case of myringosclerosis we remove the TS patch before elevating tympanomeatal flap. In such cases, we have to remove TS patch along with the tympanic membrane over it, thus creating a larger perforation. Then we proceed like a usual underlay tympanoplasty. In case of very small isolated TS patch not extending upto the annulus, we do not remove it.
In cases of ossicular Tympanosclerosis we follow the principle of removing all TS plaque preserving all ossicles followed by covering all ossicles with very thin silastic sheet lest they touch the bony boundaries of attic or middle ear (Fig. 2—Hand drawing of surgical algorithm of tympanosclerosis). We have found that there is very little amount of ossicular necrosis after removal of TS plaques. It is also noticed that preservation of incus and stapes suprastructure of paramount importance for future hearing results. We have also confirmed that if removed meticulously, there is no or little chance of refixation of the ossicles. Keeping these principles in mind, we follow these steps-
Postaural approach—conchotomy at the level of spine of Henle––elevation of tympanomeatal flap—entering the middle ear––wide canalplasty—drilling of posterosuperior quadrant (Fig. 3a)—drilling of scutum lateral and anterior to head of Malleus—removal of hard/moderately hard TS plaques anterior to head of Malleus––specially anterior malleolar fold region—drilling continues superior to malleus-incus assembly—removal of hard TS plaques between the superior surface of malleus-incus and roof of attic (Fig. 3b)—small right angles pick is very useful for this procedure––Removal of TS plaque from posterior isthmus region, sometimes stapedius has to be sacrificed to remove TS plaques from sinus tympani. Tympanosclerosis is formed in the same layers of middle ear mucosal folds. So we have to keep the mucosal folds architecture in our mind that helps us to remove this pathology easily. Drilling in the posterior notch of Rivinus region should be done very carefully as second genu of facial nerve is very close to this area. Removal of TS plaque should be done first at the region of fissula ante fenestrum and over the horizontal facial nerve, then we should focus on medial incudal fold and interosseus fold region, then proceed by cutting the stapedius (after removal of TS plaque from posterior incudal fold and plica stapedialis region), curetting pyramidal process then removal proceeds to sinus tympani region (Fig. 3c). Lastly, removal of TS done from beneath the short process (incudal ligament region). This part has to be done slowly and meticulously as the second genu of facial nerve is very near to incudal ligament. After complete removal, ossicles are attached to medial wall of middle ear only by tensor tympani and incudal ligament. Now all ossicles are covered by thin silastic sheet to prevent post-operative adhesion and fibrosis (Fig. 3e). Attic is reconstructed with crushed periosteum (harvested from cortical mastoid bone). In case of extensive TS, we prefer periosteum over cartilage for reconstruction of attic as chance of post-operative adhesion with drilled raw bone is more with cartilage. At the end type I tympanoplasty with graft placed lateral to the ossicles (Fig. 3a–e—Operative pictures of different stages of tympanosclerosis surgery).
a Surgical photograph of removal of TS plaque from sinus tympani after posterosuperior quadrant drillout. b After removal of all TS plaque, whole osssicular chain is visible. c Stapes release-after removal of necrosed incus, TS plaques are removed all around stapes (AC-Anterior crura, PC-Posterior crura), d Titanium partial prosthesis over stapes head (TF-Temporalis fascia, TMF-Tempanomeatal flap, GF-Gelfoam). e After complete removal of TS plaques, ossicles are covered with thin silastic sheet to prevent granulation formation in future
Post-operative usual care should be taken with antibiotics, decongestants, analgesics. These patients are advised to practice Valsalva manuveur extensively from second week onwards. Histopathological grading was done (Fig. 4) and documented. Routine audiogram was done after 3 months and after 1 year for documentation and follow up.
Different histopathological Grades of tympanosclerosis. a (Grade I)—Fibroblasts and collagen fibers were equally abundant in typical loose connective tissue, few calcium crystals seen. b (Grade II)—Large bundles of collagen fibers, proliferation of fibroblasts noted. c (Grade III)—Round shaped condroblast-like cells located in lacunae with intense calcification noted
Results
In this study, 90 cases of tympanosclerosis was found in 1880 cases of tympanomastoidectomies in 8 years. It was divided into.
-
(1)
Myringosclerosis (60 cases, 66.6%),
-
(2)
Ossicular Tympanosclerosis without involvement of footplate (23 cases, 25.6%),
-
(3)
Ossicular Tympanosclerosis with involvement of footplate (7 cases, 7.8%).
Treatment options included—removal of myringosclerosis, osssicular mobilization keeping ossicular integrity and mobility, Total or partial ossicular prosthesis after removal of incus & stapes suprastructure, stapedectomy with Long malleus-footplate piston.
Hearing test was done at 3 months and 1 year after surgery and tabulated. It was observed removal of tympanosclerosis with mobilization of ossicles keeping the integrity of it provides excellent short term and long term hearing results. Whenever footplate is involved results are inferior. Overall good hearing outcome (i.e., postoperative air–bone gap less than 20 dB) was noticed in 85.5% of cases of Tympanosclerosis (Table 1).
Discussion
Tympanosclerosis is the deposition of acellular hyaline in the submucosal layer of middle ear cleft and lamina propia of tympanic membrane. Microscopically, fibroblasts are seen to accumulate cytosolic matrix vesicles rich in calcium. These vesicles are adhered to cell membrane and released extracellularly after fibroblast cell death. Dystrophic calcification of degenerated collagen fibres after some mucosal injury is the main causative factor. So TS is caused by repeated mucosal insults like recurrent AOM, COM, grommet insertion. Jaisinghani [1] found it in 35% of temporal bones with COM. Tos & Stangerup [2] found it more associated with grommet insertion. Hypercalcemia and autoimmune injury are few probable associations of this disease. While estimating the gene expression level of COL 1A1, COL2A1, COL3A1, Col4A1 and osteopontin (SPP1) from the tympanic membrane of tympanosclerosis patients found that gene expression is decreased for COL1A1; increased for COL2A1, COL4A1 and osteopontin and correlate with clinical staging of tympanosclerosis.
Regarding its classification, it had been traditionally classified as Myringosclerosis, Attic disease and Diffuse disease. But in our study we found that involvement of footplate of stapes is a very important prognostic factor and we felt that this should be incorporated in the classification. So we classified TS as (1) Myringosclerosis (only lamina propia of tympanic membrane). (2) Ossicular TS without footplate involvement (mainly attic, posterior isthmus region), (3) Ossicular TS with footplate fixation.
A good amount of suspicion is necessary to diagnose TS before surgery. Like in Obstetrics as they say “You have to be ectopic minded to diagnose ectopic”—one has to be Tympanosclerosis minded to diagnose Tympanosclerosis. Unusual large air bone gap (ABG) disproportionate to the size of perforation, presence of TS near malleus or over promontory may raise the suspicion for TS. The main concept of TS surgery is removal of TS with preservation of normal ossicular continuity. Very minimal ossicular damage (mainly in long process of incus) was noticed after removal TS. Most difficult part is removal of TS from footplate area. We named it as “Stapes Release”. We follow the direction of different mucosal folds related to stapes and its footplate. Slowly we have to removed TS layer by layer form stapes-promontory; stapes-facial nerve junction. Release of annular ligament is very important to mobilise the footplate. But in rare cases it is not possible to remove TS from footplate, then we drilled out footplate with skeeter and thinned out the footplate. After seeing blue lining, we put a Teflon piston from incus to fenestra (if incus is present) or a long Malleus to fenestra assembly (if incus is absent) with thin vein graft interposition.
Vincent [3] in his landmark study showed that stapedectomy with reconstruction resulted in reduction of air bone gap to less than 20 dB in 70% and within 10 dB in 39% of patients. Whereas Gormley [4] reported only 7% patients had less than 20 dB ABG after stapedectomy in patients with footplate TS. He even reported 5% dead ear after surgery. Garon EV [5] showed ossicular fixation in 53.3% of TS patients and 4.6% of patients required stapedoplasty. They also concluded that refixation was noticed in 17.3% of patients. In a study by Cherunshrich, [6] single stage tympanomastoidectomy with total/ partial prosthesis or long malleus-fenestra piston after stapedectomy showed 71% good hearing outcome.
Tuefert KB [7] in his landmark study on long term hearing result in TS patients showed that hearing outcome was almost equal in short term and long term follow up. Almost 65% patients had good results. Gormley PK [4] demonstrated different prosthesis/pistons for assembly between neotympanum and endolymph and found no significant difference between them. In this study 3 patients landed in dead ear including one immediate hearing loss. In Yetiser S [8] study different methods of stapedectomy with TOP, stapes mobilization & POP, ossicular mobilization were employed for TS patients and showed better outcome in patients with stapedectomy with POP/TOP than mobilization. Celik H [9] in his study showed better result with total stapedectomy in oval window TS patients.
In our series, we found that removal of TS from ossicular chain in certain predetermined fashion resulted in better result. Long term follow up showed sustained good result thus negating the concept of reappearance of TS. The trick remains to maintain the ossicular integrity mainly the long process of incus and stapes suprastructure. It was noticed that layers of acellular hyaline is deposited in the same mucosal layers of middle ear mucosal folds, thus during removal of TS the orientation of mucosal folds should be kept in mind. We follow certain fixed steps while removing TS from middle ear. Removal is done from fissula ante fenestrum, horizontal facial nerve, interosseus membrane, anterior malleolar fold. Superior malleolar-incudal fold region, posterior and medial incudal fold, posterior mesotympanum, sometimes stapedius is cut, pyramidal process is curetted to remove TS from facial recess sinus tympani area. Lastly, TS is removed beneath the incudal ligament. In cases of extensive TS, after total removal of TS from ossicles, only tensor tympani and incudal ligament hold the complete ossicular chain. Thin silastic sheet was placed around the ossicles and between ossicles and attic walls, attic and posterosuperior quadrant was reconstructed with crushed periosteum and underlay type I tympanoplasty was performed.
In our study, we found that stapedectomy with TOP/malleus-fenestra long piston did not provide good hearing results. Removing TS with maintaining ossicular integrity and mobility gave < 20 dB air–bone gap in 89.8% of patients in short term (3 months) and 87.5% in long term (1 year).
Future Scope of Study
Aetiology of tympanosclerosis remains unclear. Cytokines play a very important role in development of tympanosclerosis. TNF—alpha gene expression level was measured by real time PCR with specific hydrolysed probes (TaqMan) from different tympanosclerotic tissues from middle ear. It was found that gene expression level for TNF—alpha was correlated with clinical classification of tympanosclerosis [10]. This could lead to anti-inflammatory medications for tympanosclerosis.
While estimating the gene expression level of COL 1A1, COL2A1, COL3A1, Col4A1 and osteopntin (SPP1) from the tympanic membrane of tympanosclerosis patients found that gene expression is decreased for COL1A1; increased for COL2A1, COL4A1 and osteopontin and correlate with clinical staging of Tympanosclerosis [11]. In future, treatment may be aimed to modulate these gene expressions and regulation of the degradation of their protein products could be used as a new medical approach to tympanosclerosis.
Conclusion
Tympanosclerosis is an important cause of conductive hearing loss and hinders better hearing result after tympanomastoid surgery. Removal of it without hampering the osssicular integrity is the best treatment option and it provides excellent hearing outcome. The surgical technique described in this article can be used as roadmap for removal of tympanosclerosis in stepwise manner.
References
Jaisinghani VJ, Paparella MM, Scachern PA, Le CT (1999) Tympanic membrane/middle ear pathologic correlates in chronic otitis media. Laryngoscope 109:712–716
Tos M, Stangerup SE (1989) Hearing loss in tympanosclerosis caused by grommets. Arch Otolaryngol Head Neck Surg 115:931–935
Vincent R, Oates J, Sperling NM (2002) Stapedotomy for tympanosclerotic stapes fixation: is it safe and efficient? A review of 68 cases. Otol Neurotol. 23(6):866–72
Gormley PK (1987) Stapedectomy in tympanosclerosis. A report of 67 cases. Am J Otol 8(2):123–30
Garov EV, Sidorina NG, Zagorskaya EE, Sudarev PA, Meparishvili AS (2017) The prevalence of tympanosclerosis and the effectiveness of its surgical treatment. Vestn Otorinolaringol 82(2):4–10
Chernushevich II, Anikin IA, Agazaryan AG, Korneyenkov AA, Zakharova GP, Astashchenko SV (2019) Single-stage open tympanoplasty in the form of tympanosclerosis with fixation of the stapes. Vestn Otorinolaringol. 84(2):23–28
Teufert KB, De La Cruz A (2002) Tympanosclerosis: long-term hearing results after ossicular reconstruction. Otolaryngol Head Neck Surg 126(3):264–72
Yetiser S, Hidir Y, Karatas E, Karapinar U (2007) Management of tympanosclerosis with ossicular fixation: review and presentation of long-term results of 30 new cases. J Otolaryngol. 36(5):303–8
Celik H, AslanFelek S, Islam A, Safak MA, Arslan N, Gocmen H (2008) Analysis of long-term hearing after tympanosclerosis with total/partial stapedectomy and prosthesis used. Acta Otolaryngol. 128(12):1308–13
Minoskowski T et al (2012) Assessment of Tumor Necrosis Factor alpha gene expression profile in selected structures of middle ear in patients with tympanosclerosis. Otolaryngol Plo 66(4 Suppl):20–4
Sakowicz-Burkiewicz M et al (2017) Gene expression profile of collagen types, osteopontin in the tympanic membrane of patients with tympanosclerosis. Adv Clin Exp Med 26(6):961–966
Author information
Authors and Affiliations
Corresponding author
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Ghosh, A. Monograph on Tympanosclerosis-Clinico-Pathological Corelation and Surgical Outcome: A Retrospective Study. Indian J Otolaryngol Head Neck Surg 74 (Suppl 3), 4059–4064 (2022). https://doi.org/10.1007/s12070-021-02805-4
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12070-021-02805-4