Abstract
To analyse the patients with foreign body oesophagus in relation to the clinico-radiological and socio-economic profile. The present prospective study was conducted on 100 consecutive patients of all age groups who underwent oesophagoscopy for suspected foreign body ingestion in a tertiary care hospital. The most common age group affected was 0–5 years. The median age was 5 ± 14.37 years. There was preponderance in males as compared to females, male to female ratio was 2.23:1. Majority (70%) of the patients, both males and females, belonged to rural areas. Lower socio-economic group was more commonly affected (54%). The most commonly reported symptom was foreign body sensation (55%) followed by vomiting (54%) and difficulty in swallowing (51%). Foreign body ingestion was witnessed in only 19% cases by the family members. The mean time between ingestion of the foreign body and admission to the hospital was found to be 4.5 h. The majority (97%) of foreign bodies were radio-opaque. The most common site of lodgement was just below the cricopharynx (89%). The most common foreign body retrieved in our series were coins (65%). The majority of foreign bodies (68%) were retrieved in 20–40 min after induction of general anaesthesia. In 99% of the patients we did not encounter any complications. The majority (93%) of the patient’s parents/relatives had curiosity to have a glimpse of the foreign body till they actually saw the retrieved foreign body. Foreign body lodgement is more common among children of lower socio-economic strata more so in rural areas. Rigid oesophagoscopy is a safe and effective procedure for removal of the foreign body. Early intervention makes it easier to extract the foreign body without complications.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
A foreign body (FB) is an endogenous or exogenous substance, incongruous with the anatomy of the site where it is found. Chevalier Jackson defined a foreign body as “an object or a substance that is foreign to its location” [1]. Foreign body in the esophagus is an everyday occurrence and a common emergency presentation, if left untreated, the patient may develop ischemia, oesophageal ulceration and perforation [2]. Foreign body ingestion can affect persons of any age, but vast majority of these accidents occur in children aged 6 months to 3 years [3]. Advances in endoscopic and anaesthetic techniques have dramatically increased safety in their removal. Various studies have been published on different aspects of foreign body esophagus. In view of foreign body oesophagus being a common emergency, the present prospective study was planned to study the clinico-radiological and socio-economic profile in patients with foreign body oesophagus as most of such studies in literature are retrospective.
Material and Methods
The present prospective study was conducted in the Department of Otorhinolaryngology, Pt. B.D. Sharma PGIMS, Rohtak (Haryana). The study was conducted on 100 consecutive patients of all age groups who were admitted with a history of foreign body ingestion. A detailed history including the time of onset of symptoms like difficulty in swallowing, vomiting, foreign body sensation, pain, fever, and respiratory distress were taken with a special emphasis on definitive (witnessed) history of the foreign body ingestion. The time gap between ingestion and reporting in hospital was noted. Clinical examination including the general condition and vitals was carried out. A detailed examination of the ear, nose, throat, and chest was performed. Preoperative X-ray soft tissue neck, X-ray chest, X-ray abdomen and pelvis were taken as routine procedure. CT scan was done, wherever required. Rigid oesophagoscopy was carried out under general anesthesia in all the cases after taking written informed consent. The records of all the parameters were maintained, tabulated and analysed.
Results
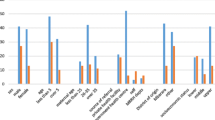
The most common age group affected was 0–5 years (Table 1). The youngest patient was 13 months of age and the eldest was 70 years old. The males outnumbered females with a male:female ratio of 2.23:1. Majority (70%) of the patients, both males and females, belonged to rural areas. Lower socio-economic group was more commonly (54%) affected. The most common symptom was foreign body sensation (55%) followed by vomiting (54%) and difficulty in swallowing (51%). Other uncommon symptoms were throat pain (9%), complaint of FB ingestion (3%), epigastric pain (2%), decreased oral intake (2%), drooling of saliva (1%) and foreign body sensation with frothing (1%) (Table 2).
FB ingestion was witnessed in only 19% cases by the family members. The mean time between ingestion of foreign body and admission to hospital was found to be 4.5 h. In all the patients, X-rays were done. CT Scan was done in only 3% of the patients of FB oesophagus. The majority (97%) of the foreign bodies were radio-opaque. Some of the X-ray pictures of unusual foreign bodies are shown in Figs. 1 and 2. The most common site (89%) of lodgement was just below the cricopharynx, other uncommon sites are depicted in Table 3. The most common FB retrieved in our series were coins (65%) although a wide variety of FBs retreived were encountered (Table 4) (Fig. 3).
The majority (68%) of foreign bodies were removed in 20–40 min. In 99% of the cases, we did not encounter any post-oesophagoscopy complication. In 1 patient, mediastinitis occurred as an immediate postoperative complication which was managed conservatively with medications. The majority (93%) of the patient’s parents/relatives had curiosity to have a glimpse of the FB till they actually saw the retrieved foreign body.
Discussion
Foreign bodies in the oesophagus are commonly encountered in emergency otolaryngology practice. In the present study, foreign body ingestion occurred most commonly in children between 0 and5 years of age, which is in agreement with other studies [4, 5].
The tendency of children at this age to put anything and everything they can put their hands on in their mouth combined with incomplete teething and immature neural mechanisms which co-ordinate aspiration and ingestion, and the habit of playing and laughing at the time of eating makes children susceptible to foreign body ingestion [6, 7]. In our study 69% of FB ingestion occurred in males. It is in accordance with the study by Sharma et al. in which male predominance was noticed in 59.4% of cases [8]. Male predominance may be attributed to their more aggressive & exploring nature.
Majority (70%) of the patients with FB ingestion belonged to rural areas. Socio-economic analysis showed that 54% patients belonged to lower socio-economic group. Higher incidence in children from lower socio-economic background may be because of the fact that they are usually left unattended by their parents due to their work commitments and children are usually left alone at home by assigning the duty to the elder sibling to take care of the younger one. Hjern et al. did not observe any difference between urban and rural patients in their analysis of 2895 Swedish toddlers with a history of foreign bodies [9]. This may be due to the fact that in Sweden even the rural population has good socio-economic status.
Patients may present with a wide range of symptoms and signs depending upon the age, nature of FB, anatomical site of lodgement and duration of time since ingestion. Foreign body sensation, vomiting, dysphagia, drooling of saliva, retrosternal pain and respiratory symptoms are the most common presenting symptoms [10]. In the present study foreign body sensation was the most common symptom in 55% followed by vomiting in 54% and difficulty in swallowing in 51% of the patients.
A witnessed history of FB ingestion is extremely important for quick and sure diagnosis. Louie et al. published a study of 225 cases with majority of patients having witnessed history of FB ingestion [11]. In our study witnessed history was found in only 19% cases. This may be due to the fact that in India many children are left unattended due to parents exigency of work.
In the present study, 70% of the patients presented within the first 8 h after ingestion of FB. The mean time between ingestion of FB and admission to the hospital was found to be 4.5 h. The shorter time to diagnose FB ingestion in children was partly due to parental alertness. One possible reason for delayed presentation is that the parents are not aware of the significance of signs and symptoms [12]. Treatment by local quacks, patients from far off places and no definitive history of FB ingestion were also the reasons for delayed presentation to the hospital. Some patients with ingested FBs do not go to the hospital for help but stay home for observation. They ingest food especially bananas to dislodge the FB, which prolongs the time from ingestion to effective treatment as was also observed in the present study. However, this causes greater harm and a larger economic burden for the patients. So, parental education and public awareness may help in reducing the incidence, morbidity and mortality in cases of FB ingestion. Our results are consistent with study done by Sinha et al. in which 75.7% patients presented within 24 h of FB ingestion [13].
The most common FBs (92%) retrieved in the present study were inorganic in nature like coins, battery cell, steel back cover of wrist watch etc. In the present study we found coins in 65% patients, followed by battery cell in 13% of cases, similar to study by Sharma et al. [10]. The curiosity of children towards the coins is well known and this explains why coins are the predominant FB in the paediatric age group. Most (86%) of the foreign bodies found in the present study were round (coins 65%, battery cell 13%, locket 3%, button 2%, metallic washer 2%, and steel cover of wrist watch 1%) and in only 4% cases, pointed FBs were found. Others (10%) were irregular like chicken bolus, fruit seed, artificial tooth etc. It was observed that round FBs were the easiest to retrieve. It is similar to a study done by Singh et al. in which 81% of FBs were round, 13% pointed and 6% irregular. Type of FBs ingested differ among countries according to their feeding habits, cultures, festivals, and socio economic status [4].
The most common site of lodgement of FB (89%) was just below the cricopharynx in the present study. In a study conducted by Shivakumar et al. the majority of the FBs (83.5%) were impacted at the cricopharyngeal sphincter [14]. This is comparable with the present study.
Radiography plays a critical role in the diagnosis and management of ingested FBs, especially in paediatric population. Lin et al. observed that diagnosis of FB ingestion is based on three important elements: eye witness, X-ray and upper GI endoscopy [15]. Several studies showed that use of radiograph is a useful tool in the diagnosis of FB ingestions but radiolucent substance can be missed by this method [16,17,18]. Luk et al. showed that CT scan is 96% specific in diagnosis of FB even in negative upper GI endoscopy cases [19]. Prompt radiologic recognition of FB is necessary for adequate treatment, as some ingested objects need emergent/urgent retrieval i.e. batteries, magnets, sharp and larger impacted objects. Quickly identifying the radiographic signs of impaction is also crucial, as many FBs are radiolucent [20]. In the present study CT scan was required only in 3 out of 100 patients. In all other 97 patients X-ray chest and soft tissue neck was sufficient. So radiography remained the modality of choice in diagnosing ingested FBs.
Upon diagnosis, early oesophagoscopy is mandatory as earlier the oesophagoscopy is done, the lesser are the complications. Biancari et al. and Palta et al. found that delays from ingestion to presentation and intervention may account for the relatively high rates of surgery, perforation, and mortality [21, 22].
In the present study oesophagoscopy was done in all 100 patients and maximum number of FBs were removed within 20–40 min after induction of anesthesia i.e. 68%. In 7 patients FB could not be retrieved as it had passed down into the stomach. In our study all the patients were discharged on the next day after oesophagoscopy, except one patient who had post-oesophagoscopy complication. The patient developed mediastinits after ingestion of chicken bone and was managed conservatively.
FBs oesophagus are a serious condition that may prove fatal if not treated properly. Accurate diagnosis and urgent management make it easier to remove them and decrease the complications risk. Rigid oesophagoscopy remains the gold standard for extracting FBs from oesophagus. Early reporting to the hospital on the part of patient and earliest intervention by otolaryngologist makes it easier to remove the foreign body and obviates the possible complications.
References
Jackson C, Jackson CL (1936) Diseases of the air and food passages of foreign body origin. WB Saunders Company, Philadelphia
Song Kee LMW, Topazian M (2015) Gastrointestinal endoscopy. In: Kasper DL, Fauci AS, Hauser SL, Longo DL, Jameson JL, Loscalzo J (eds) Harrison’s principles of internal medicine, 19th edn. McGraw-Hill, NewYork, pp 1880–1900
Uyemura MC (2005) Foreign body ingestion in children. Am Fam Physicians 72:287–291
Singh RB, Dubey RK, Pandey V, Kumar V, Sharma SP, Annavi B (2014) Foreign bodies in digestive tract of children: a tertiary care hospital experience. Int J Med Public Health 4:463–466
Hamilton JK, Polter DE (1993) Gastrointestinal foreign bodies. In: Sliesenger MH, Fordtran JS (eds) Gastrointestinal disease: pathophysiology, diagnosis and management. W.B. Saunders Co., Philadelphia
Goel HC, Yadav SPS, Kohli GS, Singh J (1989) Oesophageal foreign bodies. Otolaryngology 18:49–52
Asif M, Haroon T, Khan Z, Muhammad R, Malik S, Khan F (2013) Foreign body oesophagus: types and site of impaction. Gomal J Med Sci 11:163–166
Rodríguez H, Passali GC, Gregori D, Chinski A, Tiscornia C, Botto H et al (2012) Management of foreign bodies in the airway and oesophagus. Int J Pediatr Otorhinolaryngol 76:84–91
Hjern A, Ringback-Wietoft G, Anderson R (2001) Socio-demographic risk factors for home-type injuries in Swedish infants and toddlers. Acta Paediatr 90:61–68
Sharma B, Raina S, Sharma N, Sharma R, Grover N, Sood A et al (2016) Endoscopic management of foreign bodies from the upper gastrointestinal tract in the hills of Himachal Pradesh, India: a 5-year tertiary care experience. J Dig Endosc 7:144–147
Louie JP, Alpern ER, Windreich RM (2005) Witnessed and unwitnessed esophageal foreign bodies in children. Pediatr Emerg Care 21:582–585
Singh G, Sharma S, Khurade S, Gooptu S (2014) Ingested foreign bodies in children: a report of two cases. J Fam Med Prim Care 3:452–455
Sinha S, Kumar S, Anshumita A (2016) Upper gastrointestinal tract foreign body in children in India. Int Surg J 3:2046–2049
Shivakumar AM, Naik AS, Prashanth KB, Hongal GF, Chaturvedy G (2006) Foreign bodies in upper digestive tract. Indian J Otolaryngol Head Neck Surg 58:63–68
Lin CH, Chen AC, Tsai JD, Wei SH, Hsueh KC, Lin WC (2007) Endoscopic removal of foreign bodies in children. Kaohsiung J Med Sci 23:447–452
Shinhar SY, Strabbing RJ, Madgy DN (2003) Esophagoscopy for removal of foreign bodies in the pediatric population. Int J Pediatr Otorhinolaryngol 67:977–979
Orji FT, Akpeh JO, Okolugbo NE (2012) Management of esophageal foreign bodies: experience in a developing country. World J Surg 36:1083–1088
Wai Pak M, Chung Lee W, Kwok Fung H, Van Hasselt CA (2001) A prospective study of foreign body ingestion in 311 children. Int J Paediatr Otorhinolaryngol 58:37–45
Luk WH, Fan WC, Chan RY, Chan SW, Tse KH, Chan JC (2009) Foreign body ingestion: comparison of diagnostic accuracy of computed tomography versus endoscopy. J Laryngol Otol 123:535–540
Plowman RS, Dance L, Barnes C, Jorgensen SA, Towbin AJ, Towbin R (2018) A radiolucent esophageal foreign body: diagnosis, management and potential complications. Appl Radiol 47:28–29
Biancari F, D’Andrea V, Paone R, Di Marco C, Savino G, Koivukangas V et al (2013) Current treatment and outcome of esophageal perforations in adults: systematic review and meta-analysis of 75 studies. World J Surg 37:1051–1059
Palta R, Sahota A, Bemarki A, Salama P, Simpson N, Laine L (2009) Foreign body ingestion: characteristics and outcomes in a lower socioeconomic population with predominantly intentional ingestion. Gastrointest Endosc 69:426–433
Acknowledgements
Dr. Savita Saini, Senior professor and head, Departmment of anaesthesiology, PGIMS, Rohtak, Haryana.
Author information
Authors and Affiliations
Contributions
VK: Manuscript review, Final Approval. SPSY: Manuscript review, Final Approval. RR: Definition of intellectual content, Manuscript editing. HM: Data acquisition, Definition of intellectual content, Manuscript editing. AM: Definition of intellectual content, Literature search.
Corresponding author
Ethics declarations
Conflict of interest
The authors declare “No conflict of interest”.
Informed Consent
Informed and written consent was taken at the time of surgery and before the submission of case report.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Kalra, V., Yadav, S.P.S., Ranga, R. et al. Epidemiological, Clinical and Radiological Profile of Patients with Foreign Body Oesophagus: A Prospective Study. Indian J Otolaryngol Head Neck Surg 74, 443–448 (2022). https://doi.org/10.1007/s12070-021-02553-5
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12070-021-02553-5