Abstract
This paper aims to assess correlation of site, size and duration of tympanic membrane perforation with hearing loss using pure tone audiogram and surgical outcome in terms of above parameters. The present study was conducted on 100 patients in Department of ENT and HNS, SMGS Hospital, Government Medical College Jammu during a time period of November 2018 to October 2019. All the patients with age 15–60 years who presented with tympanic membrane (pars tensa) perforation were included in the study. According to the size of perforation, mean pure tone threshold in group I was 20.87 ± 3.86 dB, in group II was 26.45 ± 6.08 dB and in group III was 32.6 ± 5.56 dB. The difference in hearing threshold between all the three groups was significant statistically. In terms of site, group E had maximum hearing threshold (34.67 ± 4.20 dB), followed by group B (32.71 ± 5.88 dB). Group A had the lowest hearing threshold of 24.99 ± 6.21 dB. The difference between hearing thresholds of group B perforations and group A perforations was statistically significant (p < 0.05). However, the difference between group E and group B was insignificant. This study has shown significant correlation between the size and the site of the perforation to the degree of hearing loss. The bigger the perforation, the greater the hearing loss. The central perforations were associated with more hearing loss than posterior perforations, thus refuting the hypothesis that site and size of a tympanic membrane perforation does not affect the degree of conductive hearing loss. This study did not show any correlation between duration of disease and degree of hearing loss. Surgical and audiometric results obtained in this study can be accepted as satisfactory and as expected by the literature.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Chronic otitis media is defined as a permanent abnormality of pars tensa or pars flaccida, most likely as a result of earlier acute otitis media, negative middle ear pressure or otitis media with effusion [1].
COM often presents with hearing loss. For understanding hearing loss, we need to understand the mechanics of sound transmission in diseased middle ears. It has been an area of constant research among otologists and has been studied in cats by Wever and Lawrence [2] and Payne and Githler [3] and on human temporal bones by Voss et al. [4] and Mehta et al. [5].
Tympanic membrane is a membranous partition separating the external auditory meatus from the tympanic cavity, measuring 9–10 mm vertically and 8–9 mm horizontally [6]. It has two parts- pars tensa and pars flaccida. Both the pars tensa and pars flaccida comprise of three layers. There is an outer epithelial layer, middle fibrous layer, and inner mucosal layer [7]. Apart from conduction of sound across the middle ear, tympanic membrane also has a protective role on middle ear cleft and round window niche. Intact tympanic membrane protects middle ear cleft from infections and shields round window from direct sound waves which is referred as round window baffle [8].
Tympanic membrane perforation represents a hole in the eardrum, establishing a communication between the middle and external ear. Perforation is caused by variety of causes, the most common being trauma (barotrauma, temporal bone fracture), infections (acute otitis media, chronic otitis media, tuberculosis) and iatrogenic.
Tympanic membrane perforation leads to varying degrees of conductive hearing loss. A perforation of tympanic membrane decreases the surface area of tympanic membrane available for sound transmission and allows sound to fall directly on middle ear. As a result, the pressure gradient between the inner and outer surfaces of the tympanic membrane virtually becomes insignificant. The effectiveness with which the tympanic membrane transmits the sound waves to the ossicular chain is thus hampered [9].
Loss of hearing is a national health problem with significant physical and psychosocial implications. So it is important to diagnose and treat tympanic membrane perforation as early as possible as untreated tympanic membrane perforation leads to ongoing destructive changes in the middle ear, thus adding to further hearing loss [10].
Type I tympanoplasty is one of the most commonly performed procedures in otology. Various factors influence the success rate of this procedure such as age, site of perforation, condition of the middle ear mucosa, status of the contralateral ear, number of otorrhoea per year, grafting material, surgical techniques, and associated pathologies like adenotonsillitis and sinusitis.
Considering the high incidence of COM in our country and conflicting reports of various studies on degree of hearing loss caused by perforations of various sizes and location, this study was undertaken as an effort to validate the above facts. The present study has also been done to find out the graft uptake rates in tympanoplasty type I, to compare the hearing gain achieved after tympanoplasty type I and to look for complications during the follow-up period.
Materials and Methods
The present prospective study was conducted in Department of ENT and Head Neck surgery, SMGS Hospital, Government Medical College Jammu, which is tertiary care centre, for a period of 1 year from Nov. 2018 to Oct. 2019 after seeking permission from institutional ethics committee. The study included 100 patients of either sexes, aged between 15–60 years.
Inclusion criteria:
All patients with inactive mucosal type of COM.
Exclusion criteria:
-
Age below 15 years and above 60 years of age.
-
Patients having sensorineural or mixed hearing loss.
-
Patients with atticoantral disease, attic/posterosuperior marginal perforation or cholesteatoma.
-
Patients found to have ossicular destruction intraoperatively.
-
Patients not willing to participate.
-
Patient having myringosclerosis.
Informed consent was obtained. Detailed history of the patient was taken. After systemic examination, detailed examination of ear, nose and throat was done. Ear examination was done using Bull’s eye lamp, Otoscope and microscope/Otoendoscope. Tuning fork test using (256, 512, 1024 Hz tuning forks) were done. The tympanic membrane was divided into five segments anterosuperior, posterosuperior, anteroinferior, posteroinferior and central for the localization of the site of perforation.
Site of perforation was assessed using Otoscope and Otomicroscope. To estimate size of perforation a 1 mm thin wire loop was used. Readings were taken under microscope. Two diameters were taken for each perforation, one maximum vertical and one maximum horizontal and area was calculated as:
where π is the 3.14159 constant, R1 is the radius along the vertical axis, R2 is the radius along the horizontal axis.
Depending upon the area, perforations were divided into three groups:
Group I = Small perforation: (0–9 mm2).
Group II = Medium sized perforation: (9–30 mm2).
Group III = Large perforation: (> 30 mm2).
[The average surface area of intact tympanic membrane were taken as 64.3 mm2.]
The type, degree and frequency of hearing loss were determined by pure tone audiometry using audiometer (Elkon 3N3 multi diagnostic) in acoustically controlled room.
Data was collected in the constructed proforma to evaluate effect of site, size and duration of perforation on the degree of hearing loss. After proper pre-anesthetic workup, all patients were taken up for surgery (Type-I Tympanoplasty) under general anesthesia/local anesthesia. Temporalis fascia graft was used for Tympanic membrane repair.
Follow Up
Otoscopy/Otoendoscopic examination was done to look for graft uptake and Pure Tone Audiometry was done at 1 month and 3 months after surgery to evaluate the hearing outcome after surgery.
Results
In our study, maximum patients were in age group 21–30 (33%) 0.10 patients were in the age group 51–60 (10%). Mean age in our study of 100 patients was (31.34 ± 12.58). There were 64 females (64%) and 36 males (36%).

Size
In our study, out of total 100 patients, 53 patients (53%) belonged to group II (9–30 mm2) followed by 37 patients (37%) in group III (> 30 mm2). Group I (0–9 mm2) had only 10 patients (10%).

The mean hearing threshold in group I (0–9 mm2) was 20.87 ± 3.86 and in group II (9–30 mm2) mean threshold was 26.45 ± 6.08. In group III (> 30 mm2) hearing threshold was 32.6 ± 5.56.
Perforation according to size | Pre op. AC threshold (dB) [Mean ± SD] |
|---|---|
Group I (0–9mm2) | 20.87 ± 3.86 |
Group II (9–30 mm2) | 26.45 ± 6.08 |
Group III (> 30 mm2) | 32.6 ± 5.56 |
The mean preoperative air-bone gap in group I (0–9 mm2) was 12.13 ± 2.73 and in group II (9–30 mm2) mean air-bone gap was 14.78 ± 4.48. In group III (> 30 mm2) air-bone gap was 17.92 ± 4.56.
Perforation according to size | Pre op. AB gap (dB) [Mean ± SD] |
|---|---|
Group I (0–9mm2) | 12.13 ± 2.73 |
Group II (9–30 mm2) | 14.78 ± 4.48 |
Group III (> 30 mm2) | 17.92 ± 4.56 |
Site
In our study, all Perforations were divided into five groups, group A, B, C, D and E.
Group A: A.S, A.I, A.S + A.I.
Group B: P.S, P.I, P.S + P.I.
Group C: P.S + A.S.
Group D: P.I + A.I.
Group E: Perforation involving any three or all four quadrants.
In our study, maximum perforations (31%) belonged to group B followed by group A (26%). Group D and group E had equal number of perforations (20%) each. 3% patients belonged to group C. Mean preoperative hearing loss (AC threshold) of group A was 24.99 ± 6.21 dB and of group B was 32.71 ± 2.55 dB. Group C had mean preoperative hearing loss (AC threshold) of 31.03 ± 3.66 dB and group D had mean preoperative hearing loss (AC threshold) of 29.74 ± 5.64 dB. Group E had the maximum hearing loss of 34.67 ± 4.20 dB.
Site | Pre op. AC threshold (dB) Mean ± SD |
|---|---|
Anterior (group A) | 24.99 ± 6.21 |
Posterior (group B) | 32.71 ± 2.55 |
Superior (group C) | 31.03 ± 3.66 |
Inferior (group D) | 29.74 ± 5.64 |
Central (group E) | 34.67 ± 4.20 |
The difference of hearing threshold between all groups was statistically significant (p < 0.05) except between group B and group C which was statistically insignificant (p > 0.05).
Group A | Group B | Group C | Group D | Group E | |
|---|---|---|---|---|---|
Group A | S | S | S | S | |
Group B | NS | S | S | ||
Group C | S | S | |||
Group D | S | ||||
Group E |
Mean preoperative air-bone gap (AB gap) of group A was 14.12 ± 4.92 dB and of group B was 18.77 ± 4.34 dB. Group C had mean preoperative air-bone gap (AB gap) of 15.33 ± 2.08 dB and group D had mean preoperative air-bone gap (AB gap) of 15.36 ± 5.63 dB. Group E had the maximum air-bone gap of 19.78 ± 5.23 dB.
Site | Pre op. AB gap (dB) Mean ± SD |
|---|---|
Group A | 14.12 ± 4.92 |
Group B | 18.77 ± 4.34 |
Group C | 15.33 ± 2.08 |
Group D | 15.36 ± 5.63 |
Group E | 19.78 ± 5.23 |
The difference between group E and group A or C or D is statistically significant (p < 0.05). However difference between group E and group B is not significant (p > 0.05).The difference between group D and group A or C is statistically insignificant. Group C also has significant difference with group A or D or E. The difference between group C and group B is statistically significant (p < 0.05).
Duration
Duration of disease (in years) | No. of patients | % |
|---|---|---|
Group A (< 1 year) | 3 | 3 |
Group B (1–5 year) | 25 | 25 |
Group C (\(\ge \) 5 year) | 72 | 72 |
In our study, majority of patients 72 (72%) belonged to group C followed by group B having 25 (25%) patients. Group A had only 3 (3%) of patients.
Duration of disease (AC) | Pre op. AC (dB) Mean ± SD |
|---|---|
Group A (< 1 year) | 36.23 ± 1.07 |
Group B (1–5 year) | 25.67 ± 6.38 |
Group C (\(\ge \) 5 year) | 28.78 ± 6.50 |
In our study, mean preoperative hearing loss (AC threshold) of group A was 36.23 ± 1.07 dB and of group B was 25.67 ± 6.38 dB. Group C had mean preoperative hearing loss (AC threshold) of 28.78 ± 6.50 dB.
Comparison
Groups | t-value | p-value | Significance |
|---|---|---|---|
Group A vs Group B | 2.81 | 0.009 | S |
Group A vs Group C | 1.97 | 0.052 | NS |
Group B vs Group C | 2.07 | 0.041 | S |
The difference in preoperative hearing threshold (AC Threshold) between group A & B and group B & C was significant statistically. However, the difference of preoperative hearing threshold (AC Threshold) between group A and group C was not significant statistically.
Duration of disease (AB) | Pre op. AB gap (dB) Mean ± SD |
|---|---|
Group A (< 1 year) | 12.9 ± 8.05 |
Group B (1–5 year) | 13.86 ± 4.19 |
Group C (\(\ge \) 5 year) | 16.47 ± 5.51 |
In our study, mean preoperative air-bone gap (AB gap) of group A was 12.9 ± 8.05 dB and of group B was 13.86 ± 4.19 dB. Group C had mean preoperative air-bone gap (AB gap) of 16.47 ± 5.51 dB.
Comparison
Groups | t-value | p-value | Significance |
|---|---|---|---|
Group A vs Group B | 0.34 | 0.73 | NS |
Group A vs Group C | 1.08 | 0.28 | NS |
Group B vs Group C | 1.17 | 0.24 | NS |
The difference in preoperative air-bone gap (AB gap) between all the three groups was not significant statistically.
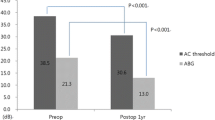
Surgical Outcome
In our study, Group II had least postoperative air bone gap (7.61 ± 3.55 dB) at three months. In group I postoperative air bone gap was 8.02 ± 3.12 dB. Group III had greatest postoperative air bone gap 9.85 ± 3.45 dB. In our study, 3 months postoperative air bone gap was least in group A (7.92 ± 2.85 dB), followed by group D (8.01 ± 3.90 dB), followed by group C (9 ± 3 dB), followed by group E (10.05 ± 4.72 dB), followed by group B (10.52 ± 3.39 dB). In our study, mean postoperative AB gap at 3 months was least in group C (10 ± 3 dB), followed by group C (8.44 ± 3.59 dB). Group B had maximum postoperative AB gap of 8.49 ± 4.34 dB.
Complications
In our study, at one month follow up out of total 100 patients, 90 patients (90%) had no complications, 5 patients (5%) had residual perforation, wound gap and otitis externa in 2 patients (2%) each. Only 1 patient (1%) had developed wound haematoma. However, at 3 months follow up 94 patients (94%) had no complications. Residual perforation persisted in all 5 patients (5%) at 3 months. 1 patient had otitis externa at 3 months.

Discussion
Various studies have tried to characterize and note various parameters of hearing affected by tympanic membrane perforation and tried to draw a correlation across these variables to give a better insight. There is still scope for further study to understand this correlation between characteristics of tympanic membrane perforation and its effect on hearing. Our study was an effort in this direction.
In our study, the most commonly affected age group was 21–30 years (33%). Our observation was similar to Sood et al. [11] but differed from the studies of Nahata et al. [12] and Bhusal et al. [13] where the most common age group was 15–24 years. There were 36 males and 64 females (male: female 1:1.77). Our finding was similar to that of Nahata et al. [12], Maharjan et al. [14] and Ibekwe et al. [15] where female preponderance seen but differed from the findings of Pannu et al. [10] and Nepal et al. [16] where there was male preponderance.
All the ears included in our study had a mild degree of hearing loss. One possible reason may be the exclusion of unsafe ears and ears with ossicular and mastoid pathology from the study. This finding was similar to the study of Nahata et al. [12] where most ears had mild hearing loss but differed from that of Maharjan et al. [14] because he found that most of ears had a moderate degree of hearing loss.
On the basis of size, perforations were divided into three groups as stated previously. The highest number of ears in our study were seen in 9–30 mm2 group (53%), while the lowest number was seen in < 9 mm2 group (10%). We observed that hearing loss increases with increase in size of perforation. This increment was statistically significant (p value < 0.05). Our view is supported by studies of Sood et al. [11], Nahata et al. [12], Maharjan et al. [14], Pannu et al. [10] and Nepal et al. [16].
However, Ribeiro et al. [17] observed no significant relation between size of perforation and degree of hearing loss in patients with inactive chronic otitis media. His study included 187 patients with inactive chronic otitis media who had a pure conductive hearing loss.
The mechanism of conductive hearing loss due to tympanic membrane perforation may be explained by the effect of two factors:-
-
Reduction in the ossicular coupling that is caused by a loss in the sound pressure difference across the inner and outer surface of tympanic membrane which decreases the phase differential between oval and round windows.
-
Reduction in the surface area of tympanic membrane that is necessary for transmission of sound wave from the external auditory canal through the ossicles to the cochlea.
In the studies of Nahata et al. [12] and Pannu et al. [10], according to the area, tympanic membrane perforations were categorised into three groups as the following: group I (0–9 mm2), group II (9–30 mm2) and group III (more than 30 mm2). Nahata et al. [12] found that the degree of hearing loss in relation to the surface area of tympanic membrane perforation was 29.41 ± 4.39 dB, 34.69 ± 4.96 dB and 38.79 ± 3.44 dB respectively. They excluded the presence of ossicular abnormality by paper patch test. The results of Pannu et al. [10] were 31.43 ± 11.59, 39.88 ± 11.43 and 55.22 ± 7.15 respectively. However they did not adopt any specific method to exclude the presence of ossicular abnormality.
In our study, the sites of tympanic membrane perforation were divided into five groups in relation to the handle of malleus. Group A (anterior) consisted of perforations involving anterosuperior quadrant, anteroinferior quadrant and both anterosuperior and anteroinferior quadrants. Group B (posterior) consisted of perforations involving posterosuperior quadrant, posteroinferior quadrant and both posterosuperior and posteroinferior quadrants. Group C (superior) consisted of perforations involving both anterosuperior and posterosuperior quadrants. Group D (inferior) consisted of perforations involving both anteroinferior and posteroinferior quadrants. Perforations involving any three or all four quadrants were grouped as Group E (central) perforations. Most (31%) of perforations were located posteriorly (group B). This finding was different from other studies that showed central group as predominant Bhusal et al. [13] (34%), Nahata et al. [12] (69%), Maharjan et al. [14] (60.5%), Ibekwe et al. [15] (77.9%) and Sood et al. [11] (80%). However, Pannu et al. [10], found most of perforations were situated anteriorly (38%).
According to the average hearing loss of speech frequencies, the maximum degree of hearing loss in our study was observed in Group E (central) perforations (34.67 ± 4.20 dB). Posterior perforation caused hearing loss more than anterior one (32.71 ± 5.88 dB: 24.99 ± 6.21 dB respectively). There was a statistically significant difference in the degree of hearing loss between Group E (central) perforation and that of Group A (anterior) or Group C (superior) or Group D (inferior) (p value < 0.05), but difference between group E and group B was insignificant (p value > 0.05). The difference between posterior and anterior group perforations was significant statistically (p value < 0.05).
Our result was consistent with the observation of Bhusal et al. [13] and Ali and Alshareda [18]. Bhusal et al. [13] found that the highest degree of hearing loss was in big central perforations (45 ± 7.6 dB), then in posterior perforations (43.3 ± 7 dB) and lowest in anterior perforations (31 ± 3 dB). The difference was insignificant between central and posterior perforations (p value > 0.05), but it was significant between anterior and that of central or posterior one (p value < 0.05). Ali and Alshareda [18] also found that maximum degree of hearing loss was observed in the central perforation (37 ± 6 dB), followed by posteriorly located perforation (25.6 ± 5 dB) and anteriorly located perforation (24.8 ± 5 dB). There was a significant difference in degree of hearing loss between centrally located perforation and that of anterior or posterior one (p value 0.000). The difference was insignificant between posterior and anterior perforation (p value 0.441).
The difference between centrally located perforation and that of the other sites is significant because centrally located perforation includes both anterior and posterior perforations. The mechanism behind the increased hearing loss in the central perforation of the tympanic membrane could be due to the reduction in the effective area of membrane in contact with the sound waves. There is a reduction of pressure difference across the tympanic membrane and depending on the position of tympanic membrane perforation, there is a reduction in mechanical coupling between the remaining intact portion of membrane and malleus. The difference between anterior and posterior perforation is also significant. This can be explained on the basis that perforations over the posterior tympanic membrane expose the round window resulting in a sound pressure which diminishes cochlear response by a “phase cancellation effect”.
Our findings differed from that of Nahata et al. [12] who showed that posterior perforations had the greatest hearing loss (39.99 ± 2.79 dB), followed by central perforations (35.64 ± 5.31 dB) and lastly anterior perforations (30.1 ± 2.98 dB). The difference was significant (p value 0.000).
In our study, we did not find any significant correlation between duration of symptoms and the degree of hearing loss. This is in agreement with Sood et al. [11] who also observed no correlation between duration of symptoms and degree of hearing loss. However, Maharjan et al. [14] in their study found a strong correlation between duration of ear discharge and degree of hearing loss. The relation between duration of ear discharge and degree of hearing loss was statistically significant with p value (0.023). John et al. 2019 also found that hearing loss increased as the duration of disease increased at all the frequencies. Comparison of average hearing loss in all the three groups showed that average hearing loss increased, and it was statistically significant.
The main objectives of tympanoplasty are getting a dry middle ear, an intact tympanic membrane, and an audiometric improvement. The success rate in the literature shows a wide variation. In our study, results of graft uptake among 100 cases was 95 (95%). 5 patients (5%) had residual perforation at the end of our follow up of 3 months, whereas in study by Kumar et al. [19] out of 50 patients, who underwent tympanoplasty during the study period, graft was accepted in 40 (80%) patients and rejected in 10 (20%) patients. Sirena et al. [20] in their study found a success rate of 80%, when evaluating the closure of the perforation. Sheeehy et al. [21] in a review of 472 cases showed a tympanic membrane perforation closure rate of 97%, while Kotecha et al. [22] in their study showed a rate of 82.2%. Black and Wormald [23] showed a surgical success of 66.6%, and Pinar et al. [24] found graft uptake rate of 74.4%.
Out of 100 patients, 90 (90%) patients had no complications during first month of surgery. Residual perforation was seen in five patients (5%). Wound gaping was seen in two patients (2%) who were managed with secondary suturing. Two patients (2%) developed otitis externa for which appropriate medical therapy was given. One patient (1%) developed wound haematoma in immediate postoperative period. At three month follow up 94 patients (94%) had no complications, residual perforations had persisted in all the five patients (5%) and they were planned for revision surgery at a later date. Out of these five patients, one patient (1%) had associated persistent otitis externa.
Conclusion
This study has shown significant correlation between the size and the site of the perforation to the degree of hearing loss. The bigger the perforation, the greater the hearing loss. The central perforations were associated with more hearing loss than posterior perforations, thus refuting the hypothesis that site and size of a tympanic membrane perforation does not affect the degree of conductive hearing loss. This study did not show any correlation between duration of disease and degree of hearing loss. Surgical and audiometric results obtained in this study can be accepted as satisfactory and as expected by the literature.
Availability of data and materials
Available from the corresponding author on reasonable request.
References
Browning GG, Merchant SN, Kelly G, Swan IRC, Canter R, McKerrow WS (2008) Chronic otitis media. In: Gleeson M, Browning G (eds) Scott-Brown’s otorhinolaryngology, head and neck surgery, vol 5, 7th edn. Edward Arnold publishers, London, p 3396
Wever EG, Lawrence M (1992) The transmission properties of the middle ear, 1950. Ann Otol Rhinolaryngol 101:191–204
Payne MC Jr, Githler FJ (1951) Effects of perforations of the tympanic membrane on cochlear potentials. AMA Arch Otolaryngol 54:666–674
Voss SE, Rosowski JJ, Merchant SN, Peake WT (2001) How do tympanic membrane perforations affect middle ear sound transmission. Acta Otolaryngol 121(2):169–173
Mehta RP, Rosowski JJ, Voss SE, O’Neil E, Merchant SN (2006) Determinants of hearing loss in perforations of the tympanic membrane. Otol Neurotol 27:136–143
Donaldson JA, Duckert LG (1991) Anatomy of the ear. In: Paparella MM, Shumrick DA (eds) Otolaryngology. Basic sciences and related principles, 3rd edn. WB Saunders Company, Philadelphia, p 26
Wright T, Valentine P (2008) The anatomy and embryology of the external and middle ear. In: Gleeson M, Browning G (eds) Scott-Brown’s otorhinolaryngology, head and neck surgery, vol 5, 7th edn. Edward Arnold publishers, London, p 3108
Ogisi FO, Adobamen P (2004) Type 1 tympanoplasty in Benin: a 10-year review. Nigerian Postgraduate Med J 11:84–87
Tonndorf K (1978) Tympanic-membrane perforation in cats with experimentally induced tympanic-membrane perforation. J Acoust Soc Am 63:436–444
Pannu KK, Chadha S, Kumar D, Preeti (2011) Evaluation of hearing loss in tympanic membrane perforation. Indian J Otolaryngol Head Neck Surg 63:208–313
Sood AS, Pal P, Kumar A (2018) Tympanic membrane perforation: correlation of hearing loss with its site and size. Int J Otorhinolaryngol Head Neck Surg 4:397–402
Nahata V, Patil CY, Patil RK, Gattani G, Disawal A, Roy A (2014) Tympanic membrane perforation: Its correlationwith hearing loss and frequency affected—an analytical study. Indian J Otol 20:10–15
Bhusal CL, Guragain RP, Shrivastav RP (2006) Size of tympanic membrane perforation and hearing loss. J Nepal Med Assoc (JNMA) 45(161):167–172
Maharjan M, Kafl P, Bista M, Shrestha S, Toran KC (2009) Observation of hearing loss in patients with chronic suppurative otitis media tubotympanic type. Kathmandu Univ Med J (KUMJ) 7(28):397–401
Ibekwe TS, Nwaorgu OG, Ijaduola TG (2009) Correlating the site of tympanic membrane perforation with hearing loss. BMC Ear Nose Throat Disord 9(1):1
Nepal A, Bhandary S, Mishra SC (2007) Assessment of quantitative hearing loss in relation to the morphology of central tympanic membrane perforations. Nepal Med Coll J 9(4):239–244
Ribeiro FA, Gaudino VR, Pinheiro CD, Marcal GJ, Mitre EI (2014) Objective comparison between perforation and hearing loss. Braz J Otorhinolaryngol 80:386–389
Ali AH, Alshareda IM (2018) Relationship between tympanic membrane perforation and conductive hearing loss in patients with chronic otitis media. Int J Otorhinolaryngol Head Neck Surg 4(1):11–17
Kumar N, Chilke D, Puttewar MP (2012) Clinical profile of tubotympanic CSOM and its management with special reference to site and size of tympanic membrane perforation, Eustachian tube function and three flap tympanoplasty. Indian J Otolaryngol Head Neck Surg 64:5–12
Sirena E, Carvalho B, Buschle M, Mocellin M (2010) timanoplastia myringoplasty type 1 and in residency surgical results and audiometric. Int Archiv Otorhinolaryngol 14:4
Sheehy JL, Anderson RG (1980) Myringoplasty. A review of 472 cases. Ann Otol Rhinol Laryngol 89(1):331–334
Kotecha B, Fowler S, Topham J (1999) Myringoplasty: a prospective audit study. Clin Otolaryngol 24(2):126–129
Black JH, Wormald PJ (1995) Myringoplasty-effects on hearing and contributing factors. S Afr Med J 85(1):41–43
Pinar E, Sadullahoglu K, Calli C, Oncel S (2008) Evaluation of prognostic factors and middle ear risk index in tympanoplasty. Otolaryngol Head Neck Surg 139:386–390
Funding
No funding was received for study.
Author information
Authors and Affiliations
Contributions
RA analysed the patient regarding the hearing and performed clinical examination. KK supervised the clinical examination and hearing assessment and was major contributor, GK contributed in writing the manuscript. AS helped out the stastics. PK read and approved the final manuscript.
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no competing interests.
Ethics approval and consent to participate
Taken from institutional ethical committee.
Consent for publication
Granted by authors and institution.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Begh, R.A., Kishore, K., Kalsotra, G. et al. Impact of Site, Size and Duration of Tympanic Membrane Perforation on Hearing Loss and Postsurgical Outcome. Indian J Otolaryngol Head Neck Surg 74 (Suppl 1), 699–706 (2022). https://doi.org/10.1007/s12070-021-02487-y
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12070-021-02487-y