Abstract
Adenotonsillectomy is the commonest otorhinolaryngology surgery for paediatrics. The purpose of this study was to determine the safety and outcome of adenotonsillectomy in a tertiary center in Malaysia. This was achieved by studying the demographics, indications, co-morbidities of patients and its association with the complications of the procedure. This retrospective study was conducted from November 2011 until October 2016. Medical records of patients aged 2–12 years old who had adenotonsillectomy done in our center were retrieved for data collection. A total of 143 patients who fulfilled the inclusion and exclusion criteria were recruited. Median age was 7.52 (± 2.98 SD) years old. Allergic rhinitis was the commonest co-morbidity (40%). Recurrent tonsillitis was the main indication (60%), followed by sleep disordered breathing (SDB) without apnea (29%), obstructive sleep apnea (OSA) (7%) and other indications (4%). Post-operative paediatric intensive care unit (PICU) admission was very low (1.4%) and was reserved for those with severe OSA with complications. None of the patients admitted to PICU post-operative had respiratory complications. The prevalence of post-tonsillectomy bleeding was only 2.1%. There was no significant association between patient’s co-morbidity with operative complications (p = 0.269). Adenotonsillectomy is indicated for children with recurrent tonsillitis and paediatric SDB. The two most severe complications, namely post-tonsillectomy haemorrhage and respiratory complications occurred but incidence was low. Criteria of post-operative PICU or paediatric high dependency unit admission for paediatric SDB has to be based on multiple clinical and logistics factors and not only patients co-morbidity and indication of surgery.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Adenotonsillectomy is a surgical procedure done with or without adenoidectomy that completely removes the tonsil, including its capsule, by dissecting the peritonsillar space between the tonsil capsule and the muscular wall [1]. It is the commonest otorhinolaringology surgical procedure for paediatric population. According to the American Academy of Otolaringology – Head and Neck Surgery, in 2006 alone there were more than 530,000 of procedures done for children aged less than 15 years old in the United States.
The American Academy of Otolaryngology—Head and Neck Surgery published a guideline for tonsillectomy in children whereby the indications for tonsillectomy are divided into absolute and relative. Absolute indications are enlarged tonsils that cause upper airway obstruction, severe dysphagia, sleep disorders or cardiopulmonary complications, peritonsillar abscess that is unresponsive to medical management, tonsillitis resulting in febrile convulsions and tonsils requiring biopsy to define tissue pathology. Relative indications for adenotonsillectomy includes three or more infections per year despite adequate medical therapy, persistent foul taste or halitosis due to chronic tonsillitis, chronic or recurrent tonsillitis in a Streptococcus carrier not responding to beta-lactamase-resistant antibiotics and unilateral tonsil hypertrophy that is presumed neoplastic. The guideline also issues contraindications for tonsillectomy which include bleeding diasthesis, anaemia, acute infection, poor anaesthetic or uncontrolled medical illness.
Although adenotonsillectomies are routinely performed, morbidity can never be overlooked. Bleeding and respiratory compromise are the two most common complications of adenotonsillectomy [2]. Post tonsillectomy haemorrhage (PTH) is a serious and well-known complication of adenotonsillectomy. Primary PTH occurs in the first 24 h post-operatively and the risk of this complication to develop is between 0.5–4.5% [2]. Secondary PTH occurring after 24 h up to 10 days post-operative is reportedly due to sloughing of eschar, trauma from solid food intake, tonsillar bed infection or idiopathic causes [3].
Respiratory complications occur in 5% to 25% of patients undergoing tonsillectomy for OSA compared to about only 1% in patients without OSA [4, 5]. It is more likely to occur in certain clinical conditions namely emergency tonsillectomy for severe OSA, children with age less than 3 years old and in those with comorbidities such as asthma, broncho-pulmonary dysplasia and neuromuscular or craniofacial abnormalities [6]. It is reported that children with obstructive sleep apnoea (OSA) tend to develop respiratory compromised as compared to PTH and vice versa in groups of children without OSA [2].
Although adenotonsillectomy is a common surgical procedure done in Malaysia, to date there are limited data on the outcome and safety of adentonsillectomy. Literature search showed there are only a few local studies on the safety of adenotonsillectomy. However, these studies were not specific for the paediatric age group. Raja Ahmad reported on the safety of adenotonsillectomy by studying the prevalence of intra-operative and post-operative complication rate. Their study concluded that this surgical procedure is safe for ambulatory services [7]. Another study by Nurliza was conducted to evaluate patient’s satisfaction and determining the complication rate of day care tonsillectomy [8]. Hence this study aimed to study the safety and outcome of paediatric adenotonsillectomy in a tertiary centre in Malaysia.
Materials and Methods
The main objective of this study was to determine the safety and outcome of paediatric adenotonsillectomy performed in Universiti Kebangsaan Malaysia Medical Centre (UKMMC). Further specific objectives were to identify the demographics and co-morbidities of patients, indications for adenotonsillectomy, the prevalence of complications and incidence of post-operative PICU admission.
This retrospective study was conducted in Universiti Kebangsaan Malaysia Medical Centre from 1st November 2016 to 31st October 2017. Sampling method was universal sampling and patient cohort was identified from ORL–HNS operation theatre registry in UKMMC. All recruited samples that fulfilled the inclusion and exclusion criteria were selected. Patients’ medical history and surgical record were retrieved from the medical record unit for data collection. The data collection sheet used for this study comprised of five main components which consist of the demographic data of patients including their co-morbidities, indications for surgery, operative complications, post-operative admission unit and post-operative outcome. Patients had been followed up for at least six months post-operatively and phone interviews were made for patients who missed their clinic follow up. Parents were asked regarding the outcome of surgery in terms of the recurrence of sore throat, snoring and further apnea episodes post-adenotonsillectomy.
All data was analysed using SPSS software version 23.0. Categorical variables were summarized in percentage and frequencies while quantitative variables were summarized using means and standard deviation. Chi square test and t-test were performed to determine the association between two categorical data. A P value of < 0.05 was considered as statistically significant.
Results
A total of two hundred and fifty nine (259) adenotonsillectomies were performed from 1st July 2011 until 30th June 2016. One hundred and forty three (n = 143) children who fulfilled the inclusion were recruited in this study.
Eighty-eight patients were male (57.9%) and 64 (42%) were female. The youngest age was two and the oldest was twelve years old with the mean age of 7.52 ± 2.98. (Table 1).
Allergic rhinitis was the commonest associated co-morbidities (40%), out of which forty patients had only allergic rhinitis (28%) while another fourteen patients had confounding asthma with allergic rhinitis (10%). Other associated co-morbidities were asthma (3.5%) and others (lymphoma, IgA nephropathy, cerebral palsies and congenital syndromes) at 6.3%. The remaining half of the patients in this study had no underlying co-morbidities (51%).
Two main indications for adenotonsillectomy were recurrent tonsillitis (60%) and paediatric sleep disordered breathing (SDB) (29%) (Table 2). In the context of recurrent tonsillitis, 37% of the patients had associated obstructive symptoms and another 23% had no obstructive symptoms. Ten patients in this study were diagnosed with obstructive sleep apnea (7%). The diagnosis of these patients was made either by an overnight pulse oxymetry or a sleep study done under the paediatric respiratory unit. Other indications of adenotonsillectomy were for chronic tonsilitis, diagnostic tonsillectomy for lymphoma and adenoid hypertrophy (4%).
In this study, ninety percent of patients had no complications following adenotonsillectomy. The two most critical complications of adenotonsillectomy were haemorrhage and respiratory complications. The incidence of post-tonsillectomy haemorrhage was low. Primary post-tonsillectomy hemorrhage occurred only in two patients (1.4%) and only one patient had secondary post-tonsillectomy hemorrhage (0.7%) (Table 3). Primary post-tonsillectomy hemorrhage which occurred during the first 24 h post-operative were treated conservatively with ice gargles, analgesia and intravenous antibiotics. The indication for adenotonsillectomy in both cases were recurrent tonsillitis. One patient with recurrent tonsillitis developed secondary post-tonsillectomy haemorrhage at day 3 post-operatively. This patient was readmitted for observation but no further surgical exploration was required.
Only one daycare patient (0.7%) developed respiratory complication in which laryngospasm occurred during extubation. The laryngospasm resolved after administration of nebulized beta-blockers and the patient required monitoring in a normal ward post-operatively. The indication of surgery for this particular case was recurrent tonsillitis with obstructive symptoms without any other co-morbidity.
Other operative complications encountered in this study were local soft tissue trauma (3.5%) and poor pain control or poor oral intake (7%). A Fischer exact test was conducted and showed no significant association between patient’s co-morbidity with complications of surgery (p = 0.269) (Table 4).
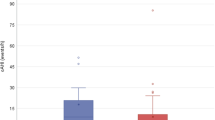
A total of ninety-nine patients underwent adenotonsillectomy as elective surgery (69%) in which ninety patients (63%) were admitted back to their respective ward post-operatively. Six patients (4.2%) who had elective adenotonsillectomy were admitted to PHDU and another two (1.4%) were admitted to PICU (Fig. 1) . At our center admission for post-operative monitoring in PICU/PHDU were planned based on patient’s co-morbidity namely severe OSA with complications, morbid obesity, poorly controlled asthma and congenital heart disease. Forty-four patients underwent adenotonsillectomy as daycare surgery (30.8%). All were discharged well on the same day except for the one patient who developed laryngospasm.
The outcome of surgery was assessed at six months post adenotonsillectomy (Table 5). Phone interviews were done for those who were no longer on follow-up. Three main symptoms were studied as the outcome of surgery. These symptoms are recurrent sore throat, residual snoring and sleep apnea. At six months post adenotonsillectomy, all patient no longer has recurrent sore throat (100%). For snoring symptoms, twenty-seven complained of residual snoring (18.5%) and the remaining 116 patients (81.1%) had no more snoring. As for witnessed apnea, all patients in this study has no more witnessed apnea post adenotonsillectomy.
Discussion
Adenotonsilectomy is a common otorhinolaryngology procedure in the paediatric age group. Common indications are recurrent tonsillitis and sleep disordered breathing (SDB) [1]. In our study, the commonest indication is recurrent tonsillitis (either with or without any obstructive symptoms) followed by sleep disordered breathing. This was comparable to a multi-center prospective study done in Switzerland whereby the commonest indication for adenotonsillectomy was recurrent tonsillitis [9]. As part of rising cases of paediatric obesity some study have reported the shifting trend of indication whereby SDB or obstructive sleep apnea (OSA) has since emerge as a common indication for adenotonsillectomy [1, 10, 11].
Allergic rhinitis is an important co-morbid which needs to be identified and managed well as it has a significant impact on the quality of life and presence of residual symptoms in paediatric patients with SDB. In this study, 40% of patients have allergic rhinitis which is comparable with a study by Kim et al. in which they reported 56% of their study subject had associated allergic rhinitis [12]. A study on quality of life amongst paediatric patients with SDB who underwent adenotonsillectomy at our center reported that those with allergic rhinitis had lesser improvement on quality of life score post-operatively [13]. Lee et al. also reported that presence of allergic rhinitis contributes to the persistent of obstructive symptoms post adenotonsillectomy [14].
One of the severe and dreaded complication of adenotonsillectomy is postoperative hemorrhages which were recorded in three patients (2.1%). These cases were managed conservatively and none had to be explored for hemostasis. All three adenotonsillectomies were done for recurrent tonsillitis. A retrospective case control study by Perkins et al. found a significant association between post tonsillectomy hemorrhage with the indication of recurrent tonsillitis (p = 0.04) [3]. A meta-analysis of complications in paediatric adenotonsillectomy by De Luca et al. reported that presence of tonsillitis without OSA increases the odds for haemorrhagic complications by 2.5 folds [2]. However, association between recurrent tonsillitis and post-tonsillectomy hemorrhage in this study was not significant (p = 1.00). One possibility is due to the fact that majority of our cases were done using cold instruments and meticulous haemostasis were done with bipolar diathermy.
Since adenotonsillectomies are routinely done for paediatric SDB and OSA, most centers advocate closer post-operative monitoring for respiratory complications in this group of patients. However, the guidelines for admission to paediatric intensive care unit (PICU) or paediatric high dependancy unit (PHDU) are only center based. Close post-operative monitoring in cases of paediatric SDB and OSA are deemed necessary as this group have higher risk for desaturation, apnea, atelectasis, pulmonary edema and cor pulmonale [5]. Those with mild complication may only need supplementary oxygen however in its severe form requires re-intubation [4]. In this study, two patients were electively admitted to PICU (1.4%) and another six were admitted to PHDU (4.2%). These admission numbers are comparative to another local study done in Universiti Malaya Medical Centre (UMMC) where the rate of elective admission post-adenotonsillectomy was much higher at 12.1% [15]. Indications for adenotonsillectomy in patients who were admitted to PICU/PHDU post operatively were severe OSA, paediatric SDB and recurrent tonsillitis with obstructive symptom. Two patients who were admitted to PICU were put on continuos positive airway pressure (CPAP) machine post-operatively and was monitored for any desaturation events. No desaturation events were observed and they were subsequently weaned off supplemental oxygen and allowed for normal ward transfer. Six patients who were admitted to PHDU did not require any post-operative supplemental oxygen. Patients with a planned admission to PICU/PHDU had their BMI recorded thus we were able to study the association between PICU/PHDU admission and BMI in this subgroup of patients. However, there was no significant association between overweight and obese BMI with post-operative admission to PICU/PHDU (p = 0.258). Thavagnanam reported a similar findings whereby there was no significant association between BMI and PICU admission in their study population (p = 0.09) [15]. In contrast, Tweedie et al. reported that children with obesity has higher likelihood ratio for post-operative PICU admission as compared to non-obese children (p < 0.001) [11]. Our finding which is similar to the local study in UMMC suggest that although obesity is a risk factor which necessitates close post-operative monitoring, the monitoring can also be done in an acute bed in a normal ward where the nursing staff can identify early signs of respiratory distress and initiate supplementary oxygen or non-invasive ventilation.
The outcomes of surgery in this study were determined by the presence of three main symptoms namely recurrent sore throat, residual snoring and apnea episodes. All children with recurrent tonsillitis were successfully treated with adenotonsillecotmy as they did not have recurrent sore throat at six months post operatively (100%). The outcome of surgery in children with recurrent tonsillitis can also be measured by the quality of life post-surgery. In a study by Nikakhlagh, children who underwent adenotonsilectomy had better quality of life in terms of less hospital visits and less time taken off school (p < 0.05) [16]. Residual snoring was low (18.9%) and could be present due to other co-morbidity such as allergic rhinitis. Local study by Othman et al. reported that allergic rhinitis and obesity may influence the quality of life amongst children who underwent adenotonsillectomy for paediatric SDB [13].
This study has several limitations. The first limitation is the significant drop-out rate due to incomplete or missing data. As a result, we might missed capturing more complications which occurred during the study period. Secondly, data for BMI were only available for the subgroup of patients who had obstructive symptoms namely SDB or OSA, hence this did not allow us to run statistical test for association to represent the whole study population.
As a conclusion, adenotonsillectomy is indicated in children with recurrent tonsillitis and sleep disordered breathing with or without OSA with very low incidence of complication. Allergic rhinitis was found to be a significant co-morbidity that causes residual symptom of SDB and should be managed optimally. Criteria for post-operative PICU/PHDU admission has to be based on multiple clinical and logistics factors and not only patients co-morbidity and indication of surgery.
References
Baugh RF, Archer SM, Mitchell RB, Rosenfeld RM, Amin R, Burns JJ et al (2011) Clinical practice guideline: tonsillectomy in children. Otolaryngol-Head Neck Surg 144(1_supp1):S1–30
De Luca CG, Pacheco-Pereira C, Aydinoz S, Bhattacharjee R, Tan H-L, Kheirandish-Gozal L et al (2015) Adenotonsillectomy complications: a meta-analysis. Pediatrics 136(4):702–718
Perkins JN, Liang C, Gao D, Shultz L, Friedman NR (2012) Risk of post-tonsillectomy hemorrhage by clinical diagnosis. The Laryngoscope 122(10):2311–2315
Kieran S, Gorman C, Kirby A, Oyemwense N, Lander L, Schwartz M et al (2013) Risk factors for desaturation after tonsillectomy: Analysis of 4,092 consecutive pediatric cases. The Laryngoscope 123:2554–2559
Ma ALT, Lam Y, Wong S, Ng DK, Chan C (2012) Risk factors for post-operative complications in Chinese children with tonsillectomy and adenoidectomy for obstructive sleep apnea syndrome. Sleep Breath 16(3):909–911
Can Assessment for Obstructive Sleep Apnea Help Predict Postadenotonsillectomy Respiratory Complications? | Anesthesiology | ASA Publications [Internet]. [cited 2018 Oct 20]. Available from: https://anesthesiology.pubs.asahq.org/article.aspx?articleid=1944249
Ahmad R, Abdullah K, Amin Z, Rahman JA (2010) Predicting safe tonsillectomy for ambulatory surgery. Auris Nasus Larynx 37(2):185–189
Nurliza I (2011) Daycare tonsillectomy: a safe outpatient procedure hospital Sultanah Bahiyah, Alor Setar Malaysia Experience. Med J Malaysia 66(5):5
Wolfensberger M, Haury J-A, Linder T (2000) Parent satisfaction 1 year after adenotonsillectomy of their children. Int J Pediatr Otorhinolaryngol 56(3):199–205
Lalakea ML, Marquez-Biggs I, Messner AH (1999) Safety of pediatric short-stay tonsillectomy. Arch Otolaryngol Neck Surg 125(7):749
Tweedie DJ, Bajaj Y, Ifeacho SN, Jonas NE, Jephson CG, Cochrane LA et al (2012) Peri-operative complications after adenotonsillectomy in a UK pediatric tertiary referral centre. Int J Pediatr Otorhinolaryngol 76(6):809–815
Kim D-K, Han DH (2015) Impact of allergic rhinitis on quality of life after adenotonsillectomy for pediatric sleep-disordered breathing: Allergic rhinitis and adenotonsillectomy. Int Forum Allergy Rhinol 5(8):741–746
Othman MN, Bee See G, Abdul LH (2016) Impact of adenotonsillectomy on the quality of life in children with sleep disordered breathing. Int J Pediatr Otorhinolaryngol 91:105–107
Lee DJ, Chung YJ, Yang YJ, Mo JH (2018) The impact of allergic rhinitis on symptom improvement in pediatric patients after adenotonsillectomy. Clin Exp Otorhinolaryngol 11(1):52–57
Thavagnanam S, Cheong SY, Chinna K, Nathan AM, de Bruyne JA (2018) Pre-operative parameters do not reliably identify post-operative respiratory risk in children undergoing adenotonsillectomy: post-operative complications. J Paediatr Child Health 54(5):530–534
Nikakhlagh S, Rahim F, Boostani H, Shirazi STB, Saki N (2012) The effect of adenotonsillectomy on quality of life in adults and pediatric patients. Indian J Otolaryngol Head Neck Surg 64(2):181–183
Acknowledgements
The authors would like to thank the Medical Record Unit of Universiti Kebangsaan Malaysia Medical Center for their support during data collection and all the individuals involved in this project.
Funding
This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
Author information
Authors and Affiliations
Contributions
Data collection, analysis and manuscript writing.
Corresponding author
Ethics declarations
Conflict of interest
No Conflicts of Interest.All authors certify that they have no affiliations with or involvement in any organization or entity with any financial interest (such as honoraria; educational grants; participation in speakers’ bureaus; membership, employment, consultancies, stock ownership, or other equity interest; and expert testimony or patent-licensing arrangements), or non-financial interest (such as personal or professional relationships, affiliations, knowledge or beliefs) in the subject matter or materials discussed in this manuscript.
Ethical Approval
Approval of study was obtained from the Research & Ethics Committee of Faculty of Medicine, Universiti Kebangsaan Malaysia Medical Center (Project Code: FF-2016-400).
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Lokman, F.L., Goh, B.S. Paediatric Adenotonsillectomy: Its Safety and Outcome in a Malaysian Tertiary Medical Center. Indian J Otolaryngol Head Neck Surg 74 (Suppl 2), 1050–1055 (2022). https://doi.org/10.1007/s12070-020-02099-y
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12070-020-02099-y