Abstract
Background
This study mainly focus on hearing loss pattern in CSOM patients undergoing tympanoplasty surgery or tympanomastoidectomy pre-operatively and analysis of the outcome of the surgery in terms of improvement in hearing (air-bone gap) after 3 months of the surgery.
Methodology
All patients of age 15–65 years reporting to ENT OPD with ear discharge and decreased hearing were screened with detailed history, clinical examination and microscopic examination.110 cases of tympanic membrane perforation who were fit for surgery were advised tympanoplasty or tympanoplasty with mastoidectomy.
Results
Our study shows that postoperative air-bone gap closure is maximum for cortical mastoidectomy type I tympanoplasty (14.03 dB), followed with cortical mastoidectomy with type II (12.2 dB), Type I tympanoplasty (11 dB), cortical mastoidectomy with type III (7.72 dB). Procedures combined with modified radical mastoidectomy showed a very poor mean improvement in our study.
Conclusion
It is very difficult to predict the results preoperatively because outcome will depend on extent of involvement of middle ear cleft by the disease process which can only be assessed intraoperatively.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Chronic suppurative otitis media is a disease characterized by chronic inflammation of mucoperiosteal lining of the middle ear cleft resulting in recurrent otorrhea and impairement of hearing [1]. Chronic suppurative otitis media (CSOM) usually causes a wide range of middle ear pathologies including permanent mucosal damages, formation of granulation tissue, cholesteatoma, ossicular erosion, tympanosclerosis and is differentiated into inactive mucosal, inactive squamous, active mucosal and active squamous type of chronic otitis media (COM) [2]. The Tympanic Membrane play a significant role in physiology of normal hearing as well as have valuable role in the pathophysiology of chronic inflammatory middle ear disease (Table 1).
The goal of tympanoplasty is to remove the underlying disease, restore hearing and produce a safe dry ear [3]. This study attempts at assessing the hearing gain by the patients, who underwent different types of tympanoplasties according to their disease status. It is often difficult to predict the hearing gain of various tympanoplasties post-surgery (Table 2).
Tympanoplasty irrespective of combination of mastoidectomy is an indication for chronic ear disease process such as perforation of ear drum due to prior middle ear infections, atelactasis of tympanic membrane, retraction pocket, cholesteatoma and chronic otitis media with effusion or mastoid granuloma. Conductive hearing loss from ossicular chain deformities may occur from either discontinuity or fixation of ossicular chain [4]. Ossiculoplasty is done to reconstruct the ossicular chain. This study has been undertaken to establish definite predictor of hearing results according to type of tympanoplasties done.This study mainly focus on hearing loss pattern in CSOM patients undergoing Tympanoplasty surgery or tympanomastoidectomy pre-operatively, and analyze the outcome of the surgery in terms of improvement in hearing (air-bone gap) after 3 months of the surgery (Table 3).
Materials and Methods
Selection of Cases
All consecutive patients between age group of 15 to 65 years reporting to ENT OPD with Tympanic Membrane perforation who are fit for surgery and are advised tympanoplasty or tympanoplasty with mastoidectomy were included in the study. Patients presenting with chief complaints of discharge from ear and decreased hearing for duration of more than 3 months and diagnosed as chronic suppurative otitis media were taken into study. A written consent was taken before participation of the patients into the study. They were given detailed information about the procedure. A detailed history was taken and complete general, systemic examination and.
local examination was carried out.
Inclusion Criteria for this Study
Patient with
-
1.
Chronic suppurative otitis media (CSOM) with small, medium, large, subtotal, total, and attic perforation.
-
2.
Tympanosclerotic patches
-
3.
Pure conductive and mixed type of hearing loss
-
4.
Between the age of 15–65 year
-
5.
Sex: Both male and female
Exclusion Criteria for this Study
Patient with
-
1.
Patients not included in the above age group.
-
2.
All ASOM
-
3.
CSOM with sensory neural hearing loss (SNHL)
-
4.
CSOM with complications
-
5.
Pregnant female
-
6.
Immuno-compromised patient
-
7.
Patient having systemic illness like—Diabetes mellitus, hypertension, tuberculosis, hepatitis.
Operation
Cases were operated under local anesthesia with sedation (2% xylocaine with adrenaline) and general anesthesia as per requirement. Surgeries were performed by senior surgeons of our hospital. Grafts material used are Temporalis fascia, Cartilage and Fascia lata. Type of surgery is decided intraoperatively depending upon extent of disease. Intra venous antibiotics were given during the hospital stay and patient discharged on oral antibiotics. Mastoid dressing kept for 7 days. Aural pack was removed on seventh day. Stitches removed on 7th post operative day. Patient were followed up for 3 months after surgery at the interval of every 15 days. Follow up Audiometry was done after 3 months of surgery.
Observation and Results
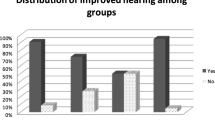
In our study, total 110 patients, out of which 41 (38%) of patients underwent Type I tympanoplasty followed by 26 (24%) cortical mastoidectomy with Type I tympanoplasty, 19 (17%) cortical mastoidectomy with Type III tympanoplasty, 11 (10%) Modified radical mastoidectomy with Type III tympanoplasty, 7 (6%) Modified radical mastoidectomy with Type IV tympanoplasty and 6 (5%) cortical mastoidectomy with type II tympanoplasty.
In our study of 110 patients, mean postoperative Air Bone Gap was 10 dB in Type I tympanoplasty, 14 dB in cortical mastoidectomy with Type I tympanoplasty, 14.1 dB in cortical mastoidectomy with Type II tympanoplasty, 21.9 dB in cortical mastoidectomy with type III tympanoplasty, 30.9 dB in Modified radical mastoidectomy with Type III tympanoplasty and 30.34 dB in Modified radical mastoidectomy with Type IV tympanoplasty.
In our study of 110 patients hearing assessment was done 3 months after the surgery. Mean PTA improvement in Type I Tympanoplasty was 11 dB, in cortical mastoidectomy with Type I tympanoplasty was 14.2 dB, in cortical mastoidectomy with Type II tympanoplasty was 13.4 dB, in cortical mastoidectomy with Type III tympanoplasty was 9.4 dB, in Modified Radical Mastoidectomy with Type III tympanoplasty was 5 dB, in Modified Radical Mastoidectomy with Type IV tympanoplasty was 3.4 dB.
Mean ABG improvement in Type I Tympanoplasty was 11 dB, in cortical mastoidectomy with Type I tympanoplasty was 14.03 dB, in cortical mastoidectomy with Type II tympanoplasty was 12.2 dB, in cortical mastoidectomy with Type III tympanoplasty was 7.72 dB, in Modified Radical Mastoidectomy with Type III tympanoplasty was 3.7 dB, in Modified Radical Mastoidectomy with Type IV tympanoplasty was 2.96 dB.
The p value for PTA improvement and that of air-bone gap comes out to be 0.0078 and 0.05 hence we can easily validate our hypothesis that different types of tympanoplasties have different level of improvement and are correlated.
Discussion
Chronic suppurative otitis media is a very common ENT problem worldwide, especially in developing countries. Around 7.8% of the Indians suffer from this infection according to WHO report [1]. It is more prominent in rural areas and is related with poor hygiene, illiteracy and is common among the middle- and low-income groups.
CSOM typically produces a mild-to-moderate conductive hearing loss. Of all the complications, hearing loss associated with chronic ear discharge is nearly always significant and tending to be more severe than those reported in other types of otitis media.
This prospective study was undertaken to study and compare hearing results in various types of tympanoplasties. Total 110 patients were included in the study.
In our study, patients from 15 to 65 years were taken into consideration. Majority of the patients 29 (26.3%) belonged to the age group ranging from 15 to 20 years compared to Indorewala et al. [7] where majority of the patients 33.3% belonged to the age group ranging from 31 to 45 years. In the study done by Balasubramaniam et al. [6] patient’s age ranging from 10 to 50 years were taken into consideration.
In our study, females 68 (62%) were slightly predominated over males 42 (38%) among 110 cases studied compared to Indorewala et al. [7] where also females were 335 (51.3%) predominated as compared to males 302 (48.72%).
In our study, 37% patients underwent type I tympanoplasty, followed by 24% patients had cortical mastoidectomy with type 1, followed by 17% patients who had cortical mastoidectomy with type III,10% had Modified radical mastoidectomy with Type 3. 6% patients underwent Modified radical mastoidectomy with Type 4. 5% patients underwent cortical mastoidectomy with type II. Compared with the study of Muqtadir et al. [5] in which 48% patients underwent cortical mastoidectomy with type I tympanoplasty, followed by 18% patients underwent cortical mastoidectomy with type III,16% patients had type 1 tympanoplasty,6% each had Modified radical mastoidectomy with Type 3, Modified radical mastoidectomy with Type 4 and cortical mastoidectomy with type II tympanoplasty.
In our study, cortical mastoidectomy with Type I tympanoplasty showed the best mean air bone gap improvement of 14.03 dB, followed by cortical mastoidectomy with type II which had a mean improvement of 12.2 dB. Procedures combined with modified radical mastoidectomy showed a very poor mean improvement in our study; only 2.96 dB for MRM with type IV and 3.7 dB MRM with type III tympanoplasty. Type I tympanoplasty showed mean hearing improvement of 11 dB and cortical mastoidectomy with type III showed mean improvement of 7.72 dB compared with the study of Muqtadir et al. [5], where Type I with cortical mastoidectomy showed the best mean improvement of 16.7 dB, followed by type II with cortical mastoidectomy which had a mean improvement of 12.66 dB. Procedures combined with modified radical mastoidectomy also showed a very poor mean improvement in Muqtadir et al. [5]; only 1 dB for type IV with MRM and 4.33 dB with type III with MRM. Type I tympanoplasty showed mean improvement of 8.875 dB and cortical mastoidectomy with type III showed equal mean improvement of 8.5 dB.
Conclusion
Tympanoplasty is a valuable procedure that can lead to improvement in hearing function of patients and prevention of recurrent ear discharge. Ideal results can be achieved by the use of the appropriate surgical technique. Apart from the surgical procedure success of the surgery also depends on the post-operative care. Proper follow-up of patients is necessary to ensure effective outcome.
The success of surgery is determined in terms of air-bone gap improvement. Our study shows that postoperative air-bone gap improvement was maximum for cortical mastoidectomy with type I tympanoplasty (14.03 dB), followed with cortical mastoidectomy with type II (12.2 dB), Type I tympanoplasty (11 dB) and cortical mastoidectomy with type III tympanoplasty (7.72 dB). Procedures combined with modified radical mastoidectomy showed a very poor mean improvement in our study. It is very difficult to predict the results preoperatively because outcome will depend on extent of involvement of middle ear cleft by the disease process which can only be assessed intraoperatively.
References
Acuin J (2004) World Health Organization: chronic suppurative otitis media: burden of illness and management options. World Health Organization, Geneva
George GB, Merchant SN, Kelly G, Swan IR, Canter R, Mckerrow WS (2008) Chronic otitis media. In: Gleeson M (ed) Scott-Brown’s otorhinolaryngology head and neck surgery, 7th edn. Edward Arnold Publishers, London, pp 3397–3438
Sismanis A (2003) Tympanoplasty. In: Glascock ME (ed) Glsscock-Shambaugh surgery of the Ear, 5th edn. Decker BC, WB Saunders Company, Hamilton, pp 463–484
Merchant SN, Ravicz ME, Puria S, Voss SE, Whittemore KR Jr, Peake WT et al (1997) Analysis of middle ear mechanics and application to diseased and reconstructed ears. Am J Otol 18(2):139–154
Muqtadir F et al (2018) A study of hearing improvement gained after tympanoplasty using various methods in cases of CSOM. Int J Otorhinolaryngol Head Neck Surg 4(1):107–111
Balasubramaniam GK, ThirunavukkarasuR KRB, Palaniappan H, Shanmugam PR (2015) Hearing benefits in various types of tympanoplasties: a prospective study. Indian J Otol 21:129–133
Indorewala S, Adedeji TO, Indorewala A, Nemade G (2015) Tympanoplasty outcomes: a review of 789 cases. Iran J Otorhinolaryngol 27(79):101
Acknowledgement
All the authors are thankful to Dr. V.K.Mahadik (Medical Director, R.D Gardi Medical College, Ujjain) for giving us the permission for conducting the study in the institute and encouragement.
Funding
No funding sources.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declared that they have no conflict of interest.
Ethical Approval
The study was approved by the Institutional Ethics Committee.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Shakti, A., Vaidya, S., Agrawal, A. et al. Comparative Study of Hearing Results in Various Types of Tympanoplasties. Indian J Otolaryngol Head Neck Surg 74 (Suppl 1), 74–78 (2022). https://doi.org/10.1007/s12070-020-01832-x
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12070-020-01832-x