Abstract
This was a randomized clinical trial, of thirty-two patients undergoing endoscopic ossiculoplasty, as a second look surgery, at 6 months after primary endoscopic cholesteatoma surgery, in a duration of 9 years. All patients underwent trans-canal endoscopic ossiculoplasty under local anesthesia. Prosthesis used were (1) Titanium partial ossicular replacement prosthesis (PORP) in fourteen, (2) Titanium total ossicular replacement prosthesis (TORP) in six and (3) Autologous cartilage in twelve cases. Puretone audiometry (PTA) were done preoperatively and postoperatively at 2 months and 3 years. Out of twenty-four cases, which presented only with stapes superstructure; fourteen underwent PORP ossiculoplasty and twelve had cartilage short columella ossiculoplasty (SCC). Out of eight cases, which had only mobile stapes footplate, six underwent TORP ossiculoplasty and only two underwent long columella cartilage ossiculoplasty (LCC). Pre-operative average air conduction threshold (AC) of pure tone audiometry were 45.47 dB (PORP), 66.10 dB (TORP), 49.15 dB (SCC) and 59.15 dB (LCC) groups. The post-operative AC at 2 months were respectively 27.37 dB (PORP), 45.83 dB (TORP), 29.99 dB (SCC) and 39.15 dB (LCC) groups. The gap of air and bone conduction (ABG) at 2 months post-operative stage were 19.05 dB (PORP), 20 dB (TORP), 20.32 dB (SCC) and 39.15 dB (LCC) groups and not much changed after 3 years. Extrusion occurred in three PORPs and four TORPs at 4–8 years after surgery. Four cases were lost to follow up. No extrusion occurred in cartilage ossiculoplasty. Trans-canal endoscopic autologous cartilage ossiculoplasty shows encouraging results comparable to titanium prosthesis in repairing ossicles in cholesteatoma disease.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Cholesteatoma diseases affecting the middle ear and attic, cause erosion of the ossicles in majority of late presentations. After complete removal of the cholesteatoma along with involved parts of the ossicles; the middle ear sound conduction mechanism is lost due to disruption of the ossicular chain. To repair the defect many materials are used till date for ossiculoplasty. The materials used are allogenic ossicles, cartilage, titanium, Teflon, gold, hydroxy apatite etc. But the best results are obtained from autogenic ossicles [1] and cartilage [2]. Conventionally microscopes are the mainstay of ossiculoplasty. Endoscopy has given: (a) wide angle of view with possibility of seeing the whole of the tympanic ring and ear canal in the same visual field, (b) more visual clarity in visualization of structures, (c) mobility which allows bypassing of narrow parts in ear canal wall and giving sense of depth, (d) seeing corners by using 0° and 30° endoscopes and (e) accuracy by magnification and seeing from close range [3]. But one-handed technique which by majority is taken as a handicap is not a hindrance in practice.
Aims
This was a randomized clinical trial, aimed at comparing the results of titanium prosthesis and autologous cartilage; used in endoscopic trans-canal ossiculoplasty.
Materials and methods
Inclusion criteria
Post-operative second look surgery cases of middle ear and attic cholesteatoma, performed at 6 months after primary endoscopic cholesteatoma surgery, in which both malleus and incus were damaged or removed due to disease involvement were taken for study. The primary cholesteatoma surgeries were done by endoscopic trans-canal or inside out mastoidectomy done by endoscopic end-aural technique; collected in a span of 9 years from January 2009 to December 2017. The ossicular configurations picked up for study were Type C (M-S+) and Type D (M-S−) of Austin Kartush classification of ossicular status [4].
Exclusion criteria
Children and adults who could not undergo surgery by local anesthesia, persons suffering from diabetes mellitus, chronic renal failure, hepatitis B and C, HIV infections, heart abnormalities, liver function abnormalities and any other major medical problems were excluded from the study.
The second look surgeries were done by the senior surgeon only through trans-canal endoscopic technique after 6 months of the primary surgery under local anesthesia. Prosthesis used were selected randomly from titanium and autologous cartilage. In cases where the stapes superstructure were present, either titanium PORP or short columella autologous cartilage were used. Cases in which only mobile stapes footplate were present, either titanium TORP or long columella autologous cartilage were used. Pure tone audiometry were done preoperatively and after 2 months and 3 years of the ossiculoplasty. Post-operative complications like pain, hearing deterioration, discharge and extrusion of the prosthesis were noted. Satisfaction of the patients regarding the outcome of the surgery were also noted. Statistical analysis was done by SPSS software version 23.
Preparations
All cases were thoroughly examined under endoscopy before surgery for any infections, discharges, fungal growth, dead tissue debris and residual cholesteatoma. The middle ear and mastoid cavities were usually free from disease before start of the ossiculoplasty. Preoperative Pure Tone Audiometry (PTA) and all hematological, radiological and biochemical investigations were done before proceeding for surgery to exclude diabetes mellitus, chronic renal failure, hepatitis B and C, HIV infections, heart abnormalities, liver function abnormalities and any other major medical problems. Patients were skin tested for hypersensitivity to lignocaine and prescribing antibiotics. Patients were kept in empty stomach minimum 6 hours before surgery to avoid vomiting and nausea. Painting of povidone iodine lotion and cleaning with rectified spirit of the external canals were done on the operating table.
Anesthesia
Sedation and premedication in adults was usually given with injections of promethazine (12.5 mg), glycopyrrolate (0.2 mg), tramadol (100 mg) and ondansetron (4 mg). Children below 18 years were given premedication and sedation by titrating the dose as per body weight. The premedication was given half an hour before surgery. Lignocaine 2% with adrenaline 1:30,000 dilution was used for local infiltration. Lignocaine 4% lotion with adrenaline 1:10,000 dilution was used for local application for surface anesthesia of middle ear mucosa. Cotton balls or absorbable gelatin gel (gelfoam) soaked in 1:1000 adrenaline were used for hemostatic packing during dissection. Strict hemostasis was a mandatory requirement for endoscopic ossiculoplasty technique.
Surgical Procedure
Patients were kept in supine position with a soft pillow underneath the head, face turned away from the surgeon. Sterile clear plastic adhesive drape with a small hole in the center for the pinna was applied to the operating side of the face and head of the patient for keeping the operating field sterile. The rest of the patient’s body except the face was covered with sterile cotton drapes. Under endoscopic control 0.3 ml injections of 2% lignocaine and adrenaline infiltration was given at the hairline (osseo-cartilaginous junction) of the external ear canal at 12, 3, 6 and 9 O’clock positions. A few cotton balls soaked in 4% lignocaine with adrenaline were kept on the tympanic membrane or middle ear to anesthetize the mucosa. As per requirement, the tragus alone or along with conchal cartilage was infiltrated for taking cartilage and perichondral grafts.
Perforated margin of the tympanic membrane was made raw by excising the edges. In cases with intact pars tensa, this step was not needed. Elevation of the tympanomeatal flap was made according to the available tympanic membrane remnant in relation to the shape of the mastoid cavity or atticotomy cavity. A circumferential incision was given from 3 O’clock to 12 O’clock clockwise on right side and 9 O’clock to 12 O’clock anticlockwise on the left side at 5 mm to 1 cm away from the annulus. Then the skin flap was elevated away from the bony canal wall along with the whole annulus. The tympano-meatal flap was reflected superiorly and kept away from the operating area. The middle ear cavity was examined thoroughly with 30° 3 mm diameter endoscopes for any residual disease and condition of the stapes superstructure or the footplate of the stapes.
The tragal cartilage was harvested along with the perichondrium attached to both sides. Usually it gives a polygonal cartilage measuring about 20 mm in length in the vertical axis and 15 mm in width in the horizontal axis and 1.5 to 2 mm in thickness (Upper left corner in Fig. 1). Leaving a 5 mm strip of cartilage covered with perichondrium towards the wider lateral end an incision was given on the posterior surface of the tragal cartilage cutting through the posterior perichondrium and full thickness of cartilage and leaving the anterior layer of perichondrium intact. By cutting the perichondrium along the margins the long strip of cartilage was removed away from the anterior perichondral layer. (1) Now we find a cartilage strip about 10 mm × 15 mm covered by the posterior layer of perichondrium (Lower left corner in Fig. 1). From this cut a 4 mm wide strip along with the perichondrium attached to one side (Lower right corner in Fig. 1). It was further trimmed to about 10 mm in size and one end was further trimmed to about 3 mm in width. A hole of about 2 mm × 2 mm was made in the wider end about 2–3 mm from the edge with small curette. The remaining tissues were kept as reserve. (2) The other piece with about 10 mm anterior perichondrium attached to it was taken and the posterior perichondrium layer was separated from the cartilage by cutting the edges. This leaves a strip of 5 mm broad cartilage strip with 5 mm of posterior layer of perichondrium attached to it and 10 mm broad anterior perichondral layer attached to its other edge (upper right corner in Fig. 1). When we take a square cartilage measuring 5 mm × 5 mm and remove the other parts of the cartilage away from the perichondral attachment; we get a 5 mm × 5 mm square cartilage attached with 5 mm and 10 mm wide perichondrium attached to its either edges. The total measurement of the perichondrium at its margins were 20 mm × 15 mm. This was used to repair the tympanic membrane. The square cartilage is made into a circular one. The remaining pieces of cartilage removed could be used to make the long columella or used to strengthen the lateral edge of the tragal skin during stitching the cut edge of tragus.
In cases where the stapes superstructure were absent, a titanium TORP or long cartilage columella were used to bridge the gap from the footplate of stapes to the perichondral or temporal fascia graft reinforced by a cartilage plate of 5 mm diameter (details given below). A strip of fascia or perichondrium of approximate size of 4 × 5 mm is placed over the footplate of stapes to stabilize the TORP.
Long cartilage columella (LCC)
A long cartilage columella measuring about 4 mm in length and about 2 mm thick and 2 mm wide was fashioned from the mastoid cortical bone or tragal or conchal cartilage in a shape shown in Fig. 2. When the long cartilage columella was not available in desired stiffness from tragus, it was harvested from the cymbal cartilage in pinna or cortical bone from mastoid. A strip of cartilage measuring 3 mm × 10 mm was cut along with perichondrium on one side of the cartilage. One end of the cartilage strip was made about 4 mm wide and a small hole was made to receive the long columella. The narrower end of the cartilage strip was inserted in a small shallow caved out area lateral to the bony Eustachian orifice on the anterior wall of the pro-tympanum or supratubal recess, made by curetting the bony wall and glued with blood clots. This was done to stabilize this end of the cartilage strip. The broader end hovers above the long columella and receive it in the hole made for it. The long cartilage columella was kept on the footplate of the stapes after interposing a cushion made of piece of fascia (about 4 × 5 mm) over the stapes footplate to stabilize the cartilage columella. The center of the cushion of fascia is deepened by the tip of suction canula of 18 gauge.
In cases where the stapes superstructure were present, titanium PORP or short cartilage columella were used to repair the ossicular defect. In case of PORP, the head of the stapes was connected with the fascia or perichondrium graft reinforced by a cartilage plate (detail is given below).
Short cartilage columella (SCC)
A long cartilage strip measuring 3 mm × 10 mm (similar to what was mentioned in the previous paragraph) was used with a hole in the broader end to accommodate the head of the stapes. The narrow end of the cartilage strip was fixed as previously described (Fig. 3).
Another circular cartilage measuring about 5 mm diameter was harvested from tragus as an island over a circular perichondrium measuring about 15 mm diameter and kept over the long cartilage strip of the LCC or SCC; or over the TORP or PORP (briefly mentioned above). When the size of the perichondrium was not adequate, a circular temporalis fascia measuring about 20 mm diameter was also used to spread over the perichondrium. The reflected tympano-meatal skin flap was delicately apposed over the fascia graft. The procedure of putting the prosthesis or cartilage columella was done last after reflecting the neo-tympanic membrane, so that it would not slip. After the trapped air was driven away from between the various layers, the position of the columella was further confirmed by gently elevating the edge of the tympano-meatal flap in the 7 to 8 O’clock position. Patient being under light sedation and local anesthesia can be tested of hearing improvement on the operating table itself by voice free field test.
No gelfoam (absorbable gelatin gel) was used inside the middle ear cavity. This was to reduce the possible adhesion and fixation of ossicles to promontory and surrounding middle ear mucosa. The external canal was packed till the hairline or osseocartilaginous junction with gelfoam impregnated with moxifloxacin skin ointment. The rest of the external canal was packed with moxifloxacin ointment. Then a cotton ball was used to plug the external auditory meatus and cotton gauze pads were used to dress the ear and bandaged with mild pressure.
Post-operative dressing was done at 7 days with cutting of stitch put on the site of cartilage removal in tragus. Endoscopic dressing was done at 30 days. Post-operative PTA was taken at 2 months and 3 years after day of surgery.
Reporting of results of hearing improvement were done by measuring the closure of the gap of air-bone conduction threshold (ABG) as per the guidelines laid down by Kartush as below:- (1) Excellent: 0 to 10 dB, (2) Good: 10 to 20 dB, (3) Fair: 20 to 30 dB, and (4) Poor: above 30 dB [4].
Results
The age of the patients ranged from 8 to 64 years with the mean and standard deviation (SD) being 30 (± 16.25) years. Sex distribution was 24 males and 8 females. Average duration (SD) of the disease is 21.81 (± 11.57) years. In all cases the malleus and the incus were absent. 24 cases presented only with stapes superstructure. Out of these, 14 cases were fitted with titanium PORP ossiculoplasty and cartilage short columella ossiculoplasty one in 12 cases. 8 cases had only mobile stapes footplate. Out of these 6 cases (75%) underwent titanium TORP ossiculoplasty and only two cases (25%) underwent long columella cartilage ossiculoplasty.
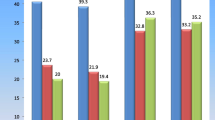
Pre-operative average air conduction threshold (AC) of pure tone audiometry (PTA) were 45.47 decibels (dB) in PORP group, 66.10 dB in TORP group, 49.15 dB in SCC group and 59.15 dB in LCC group. The post-operative AC threshold at 2 months were respectively 27.37 dB (PORP), 45.83 dB (TORP), 29.99 dB (SCC) and 39.15 dB (LCC) groups; and that at 3 years were respectively 26.66 dB(PORP), 49.16 dB(TORP), 31.42 dB(SCC) and 30 dB(LCC) (Table 1).
The ABG in pre-operative state were 37.14 dB (PORP), 40.27 dB (TORP), 39.5 dB (SCC) and 47.85 dB (LCC). ABG at 2 months post-operative stage were 19.05 dB (PORP), 20 dB (TORP), 20.32 dB (SCC) and 39.15 dB (LCC) and that at 3 years were respectively 17.57 dB (PORP), 22.5 dB (TORP), 20.71 dB (SCC) and 15 dB (LCC). (There were only two cases of LCC and one did not complete 3 years at the time of reporting and this may be the reason of the sudden reduction in ABG in 3 years). The result of the ossiculoplasty is taken as good if the ABG is reduced up to 20 dB. In our cases we find the results to be good in 10 of PORP (71.4%), 3 of TORP (50%), 6 of SCC (60%) and nil in LCC cases. The result was fair (20-30 dB) in 4 of PORP (28.6%), 3 of TORP (50%), 4 of SCC (40%) and 2 of LCC (100%) cases.
Extrusion occurred in 3 cases of titanium PORPs and 4 cases of titanium TORPs at a duration of 4 to 8 years after surgery. Four cases were lost to follow up.
Result of hearing improvement was statistically significant in all the ossiculoplasty materials used (Table 2). But in the PORP group the extrusion rate was quite high (21.4%). There were only two cases of LCC and one did not complete 3 years of reporting at the time of the study. The results of cartilage ossiculoplasty by SCC in cases where the stapes superstructures were present, are very encouraging and there were virtually no deterioration of hearing in long term follow up.
Discussion
The ideal prosthesis for ossicular reconstruction should be durable, biocompatible and easy to manipulate. Many alloplastic materials have been tried in the last three decades, such as Plastipore®, Proplast®, polyethylenes, polytetrafluroethylene, ceramics, Teflon®, hydroxyapatite, glass ionomer cement, titanium and gold. The use of homograft ossicular grafts have been abandoned by many because of risk of transmission of viral and other diseases [5]. Titanium PORP and TORP are popular with European otologists and its advantages are improved visibility via an open head, possible improved signal transfer at 2 kHz, improved handling to adjust individual anatomy, lightweight, rigidness, tissue compatibility and MRI compatibility [6, 7, 9, 10, 16]. Two-point stabilization technique of using autologous cartilage next to tympanic membrane and fascia over the footplate, which were done in our study, were used with improved results by Berenholz et al. [8]. The two-point stabilization was done to prevent slippage of TORP and LCC. Leonardo Berenholz et al. were of the opinion that cartilage did not get fixed to surrounding bone, like promontory and facial canal; and was considered a good option to make columella replacement from tympanic membrane to footplate of stapes, but lack of stiffness would be a significant disadvantage [8]. We have successfully used cartilage to fashion columella showing encouraging results. Our number of LCC was less and further study in this may ultimately prove its worth. Our technique of using a strip of cartilage fixed at one end to the wall of middle ear cavity makes the columella more stable and resistant to slippage.
In this study we attempted to focus only on more difficult cases of ossicular status (Austin/Kartush) Type C (M-S+) and Type D (M-S−) by using cartilage and titanium prosthesis and compared the results of the two identical groups of “SCC and PORP” on the one hand and “LCC and TORP” on the other hand respectively. The number of LCC were only two and thus the statistical calculation was not ideal to reach a logical conclusion in the comparison between TORP and LCC. The results of SCC was very much comparable to PORP. SCC is more favorable because of high chances of extrusion in PORP observed in the study. LCC results were encouraging in the two cases that were done. But more study is needed to reach to a conclusion. Autologous cartilage is more acceptable due to easy availability, no cost, no chance of disease transmission and less chances of extrusion and resorption.
We compared our cartilage ossiculoplasty with titanium prosthesis because, titanium prostheses are the most recent and are showing comparatively better results from those made from other materials [9, 10]. Most studies of titanium prosthesis ossiculoplasty combines both PORP and TORP and shows results of about 75% success rates and ABG ranging from 19 to 20.6 dB [7, 11, 12]. This is comparable to our study result of 71.4% success rate and ABG average of 19.05 dB. Two studies show much improved ABG in the range of 9 to 10.62 dB with about 73% success rate but follow up of only 13 months [11, 14]. Results of ossiculoplasty after cholesteatoma surgery are poorer [14]. In our study, all were canal wall down surgeries done for cholesteatoma. The ossiculoplasty was done 6 months after the primary surgery of cholesteatoma removal. At the end of the primary surgeries, the tympanic membranes were either closed or left with minimal perforations. The ossiculoplasty done 6 months later is beneficial because the middle ear mucosa and the canal skin are healed, healthy and have less bleeding during revision surgery. The improved result may be the result of operating on healed tympanic cavity.
Extrusion rate of titanium prostheses was low about 1% in the series of Dalchow et al. [15]. Displacement was seen in 2.2% by Meulemans et al. [13]. Our extrusion rate was very high regarding titanium PORP (21.4%) and TORP (66.6%). Most extrusion rates in studies did not mention separately for TORP and PORP; and follow up duration was much less than that of the present study. No extrusion of cartilage columella was reported in published literatures.
Conclusion
Autologous cartilage is an ideal choice of prosthesis for ossiculoplasty because it (1) is readily available from a few sites in the pinna, (2) is of no extra cost, (3) does not get fixed to bone, (4) does not transmit diseases, (5) is easily fashioned, (6) does not get extruded as there is no tissue reaction and (7) is not resorbed even years after being implanted.
The results of the most recent and widely acclaimed titanium prostheses are very much comparable to those of cartilage columella.
Endoscopic trans-canal approach under local anesthesia is a very convenient procedure, in which hearing can be tested roughly at the operating table itself. This procedure require short operating time, does not require overnight hospital stay, gives ease of maneuver and maximum clarity of vision.
References
Mahadevaiah A, Parikh Bhavin (2009) Use of autogenic and allogenic malleus in tympanic membrane to footplate assembly—long term results. Indian J Otolaryngol Head Neck Surg 61:9–13
Malafronte Giuseppe, Filosa Barbara, Mercone Frieda (2008) A new double-cartilage block ossiculoplasty: long term results. Otol Neurotol 29:531–533
Tarabichi Muaaz (1999) Endoscopic middle ear surgery. Ann Otol Rhinol Laryngol 108:39–46
Kartush JM (1994) Ossicular chain reconstruction. Capitulum to malleus. Otolaryngol Clin North Am 27:689–715
Sismanis A (2003) Tympanoplasty. In: Glasscock ME, Gulya AJ (eds) Glasscock-Shambaugh surgery of the ear, 5th edn. BC Decker Inc Elsevier, Hamilton, pp 463–485
Zenner HP, Stegmaier A, Lehner R, Baumann I, Zimmermann R (2001) Open Tubinggen titanium prosthesis for ossiculoplasty: a prospective clinical trial. Otol Neurotol 22(5):582–589
Krueger WWO, Feghali JG, Shelton C et al (2002) Preliminary ossiculoplasty results using the Kurz titanium prosthesis. Otol Neurotol 23(6):836–839
Berenholz L, Burkey J, Lippy W (2012) Total ossiculoplasty: advantages of two-point stabilization technique. Int J Otolaryngol. https://doi.org/10.1155/2012/346260
Gardner EK, Jackson CG, Kaylie DM (2004) Results with titanium ossicular reconstruction prosthesis. Laryngoscope 114(1):65–70
Martin AD, Harner SG (2004) Ossicular reconstruction with titanium prosthesis. Laryngoscope 114(1):61–64
Vassbotn FS, Meller P, Silvola J (2007) Short term results using Kurz titanium ossicular implants. Eur Arch Otorhinolaryngol 264(1):21–25
Ho SY, Battista RA, Wiet RJ (2003) Early results with titanium ossicular implants. Otol Neurotol 24(2):149–152
Meulemans Jeroen, Wuyts Floris L, Forton Glen E J (2013) Middle ear reconstruction using the Titanium Kurz Variac partial ossicular replacement prosthesis: functional results. JAMA Otolaryngol Head Neck Surg 139(10):1017–1025. https://doi.org/10.1001/jamaoto.2013.4751
Quaranta N, Zizzi S, Quarata A (2011) Hearing results using titanium ossicular replacement prosthesis in intact canal wall tympanoplasty for cholestestoma. Acta Otolaryngol 131(1):36–40
Dalchow CV, Grun D, Stupp HF (2001) Reconstruction of the ossicular chain with titanium implants. Otolaryngol Head Neck Surg 125(6):628–630
Fisch U, May J, Linder T, Newmann IC (2004) A new L-shaped titanium prosthesis for total reconstruction of the ossicular chain. Otol Neurotol 25(6):891–902
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
None.
Informed Consent
Informed consents were taken in accordance with ethical standards of the institution.
Rights and permissions
About this article
Cite this article
Potsangbam, D.S., Akoijam, B.A. Endoscopic Transcanal Autologous Cartilage Ossiculoplasty. Indian J Otolaryngol Head Neck Surg 71, 54–59 (2019). https://doi.org/10.1007/s12070-018-1518-x
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12070-018-1518-x