Abstract
Tympanoplasty is one of the ever evolving surgical procedures mainly aimed at restoring the hearing loss and eradication of middle ear disease. We have made an attempt to assess the hearing improvement of various types and techniques of tympanoplasty. A prospective observational study was done on 50 cases of CSOM, of which 45 cases were tubotympanic type, and 5 cases were attico-antral. Patients of only pure conductive component with good cochlear reserve and good Eustachian tube function were considered for the study. This study aims at assessing the hearing improvement with various types of tympanoplasty.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Chronic suppurative otitis media is worldly prevalent disease with otorrhoea, hearing loss, otalgia causing psychological trauma and financial burden to the society. In an attempt to overcome this menace, various techniques of Tympanoplasty have evolved out and from time to time improvisation was done based mainly in terms of hearing improvement and disease free ear.
CSOM is the main indication for Tympanoplasty. It is a disease of the middle ear with a wide range of pathology affecting mastoid, facial nerve and ET. For this reason Tympanoplasty unlike Stapedotomy, doesn’t have a standardised procedure. The technique and procedure varies according to the individual case findings and pathology.
“Tympanoplasty is an operation to eradicate disease in the middle ear and to reconstruct the hearing mechanism, with or without tympanic membrane grafting [1]”. This operation can be combined with either an intact canal wall (ICW) or a canal wall down (CWD) Mastoidectomy to eradicate disease from the mastoid area.
Since the fundamental principles of Tympanoplasty [1] were introduced by Wullstein and Zollner, surgery of the ear has been directed toward the restoration of function as well as providing a stabilized trouble-free ear. Zollner and Wullstein provided a classification of Tympanoplasty that focused on the type of ossicular chain reconstruction (OCR) needed. The five types of Tympanoplasty they described refer to the most lateral intact structure on which the conductive mechanism will be constructed. Type I Tympanoplasty indicates all three ossicles to be present and mobile. Thus, OCR is not needed. Type II grafts the tympanic membrane to an intact incus and stapes. A type III exists when an intact mobile stapes superstructure is present and the tympanic membrane or graft remains directly on the stapes superstructure. Type IV describes an absent or eroded superstructure with the graft or tympanic membrane overlying a mobile stapes footplate. Type V Tympanoplasty refers to a fenestration created in the horizontal semicircular canal.
This Prospective and observational study is focused on Tympanoplasty and reconstruction of the tympanic membrane and analyses the audiometric pattern of hearing loss in CSOM patients undergoing Tympanoplasty pre- operatively, and assess the outcome of the surgery in terms of improvement in hearing after 3 and 6 months later post- operatively. The Success rate is judged by the standard parameters like the Gain in A–B gap to within 20 dB, Gain in Air Conduction and Gain in hearing more than 15 dB post-operatively.
Materials and Methods
Only 50 patients are included in the present study. Among the 50 patients 5 patients with Attico antral disease and 45 with Tubotympanic disease are included. Patients of both safe and unsafe type of chronic suppurative otitis media with good cochlear reserve and good Eustachian tube function were selected. Patients with complications of CSOM Patients, suffering from hypertension and diabetes, Patients with any malignancy, Patients having hearing loss of sensorineural type or mixed type were excluded from the study.
All the patients who presented signs and symptoms suggesting CSOM were submitted to an assessment protocol, supervised by the same examiner based on a guided history taking, specific physical exam (otoscopy and rhinoscopy), audiogram, Examination under Microscope done to better visualize the tympanic membrane perforation. During history taking, the patients were questioned about disease onset, period of time spent without otorrhea, number of otologic infections per year and if they had undergone previous otologic surgeries.
Routine investigations apart from Examination under Microscope were done in every case, which has provided useful information i.e., perforation size (percentage of area perforated in the tympanic membrane), location according to quadrant (antero-inferior, antero-superior, postero-inferior and postero-superior), Tympanosclerosis, possibility of visualizing all the perforation borders and presence or absence of inflammatory mucosa in the middle ear. Patient was assessed radiologically to know the presence and extent of Cholesteatoma by X-ray Mastoids and C.T. Scan. All patients underwent diagnostic nasal endoscopy (DNE) in order to check nasal conditions, looking for pathologies that could interfere in the proper functioning of the Eustachian tube.
The audiometry was done following standard protocol. Pure tone Audiogram is done in every selected patient, comprising the following frequencies: 250, 500, 1000, 2000, 3000, 4000, 6000 and 8000 Hz in all the patients who presented satisfactory clinical control of otorrhea, and who were the candidates for the surgical procedure, which gave an assessment of the degree of hearing loss and its type. For calculation of average of hearing loss (air conduction threshold) three frequencies were selected. They were: 500, 1000 and 2000 Hz. These frequencies were selected because they represent speech frequency range and elevation of threshold in these frequencies will be clinically significant.Pure tone threshold audiometry has become the standard behavioral procedure for describing audiometry sensitivity; therefore, pure tone audiometry had been used for assessment of hearing level in this study.
Only the patients with pure conductive type of hearing loss are taken into study. The Audiometer (Elcon N3D) used in this study was manual. The technique followed was Carhart and Jerger’s technique which is mostly used (technique of 5 up and 10 down method). The test was performed in acoustically treated room with no ambience noise. Standard headphone was used for air conduction. Where ever the Interaural bone gap was 40 dB or more masking was applied. Patient was explained about the procedure before audiometry and adequate time was taken for testing.
The operations are performed under local or general anesthesia using a microscope. The in-lay technique was used for all perforations; the perforation was approached in a trans-meatal via when the perforation borders were visible and the external acoustic meatus favored its visualization, and the perforation was approached via retro-auricular incision when one of the borders was not seen or the external acoustic meatus was too curved and thus preventing the visualization of the whole perforation; as to the type of graft, we used either the temporal muscle fascia or tragus cartilage with its perichondrium, After clearing the disease from the middle ear and mastoid as necessary, the status of ossicular chain was assessed. Type of Tympanoplasty procedure was planned according to the status of the middle ear and ossicular chain.
All the patients are followed after surgery as usual on the 7th and 14th days. But the audiogram was done on 12th and 24th weeks to assess the outcome i.e., the improvement of hearing objectively.
We used the criteria recommended by the Japan Clinical Otology Committee for calculation of the hearing improvement (Tai, 1998) [2].
-
Using the proportion of patients with a postoperative hearing within 40 dB as the first criterion
-
Using hearing gain exceeding 15 dB as the second criterion
-
Using postoperative air-bone gap within 20 dB as third criterion
All the results are tabulated and analyzed and compared with other standard studies.
Observation
A period of 24 months was taken into study. The detailed information regarding age, sex, clinical findings, pre-operative air bone gap findings, intra-operative middle ear and ossicular pathology, type of reconstruction and post-operative air bone gap findings were noted.
As shown in Table 1, majority of cases (80%) were between 11 and 30 years, the mean age was 23.5 years. Females—26 (52.00%) are more compared to male—24 (48.00%), patients in the present study. Of the 50 patients, 21 (42%) patients had disease in the right ear, 21 (42%) had disease only in left ear and 8 patients (16%) had disease in both ears. Out of the eight patients with bilateral disease, the ear with more hearing loss and extensive disease was operated on first.
Commonest presenting complaints are ear discharge and hearing loss seen in all the (100%) patients. Tinnitus is found in 15%, pain in the ear in 33.3% and vertigo in 11.3% of patients as shown in Table 2. On microscopic examination of the operating ears, the presence of central perforation was the commonest finding (90%). Attic perforation is seen in 4% of patients and Postero Superior Marginal perforation in 6%. Of all the perforations, majority was located in Central Malleolar region 19 (38%) as shown in Table 3.
In the present study we observed that 100% patients had hearing threshold more than 30 dB. Majority of patients have came with mild to moderate hearing loss that ranged from 35.1–50 dB i.e., 41 patients out of 50 (82.00%) as shown in Table 4.

Out of 50 patients we had performed 37 (74.00%) type I Tympanoplasties, 8 (16.00%) type II and 5 (10.00%) patients required type III Tympanoplasties along with MRM.
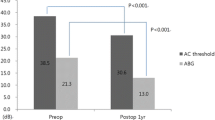
Mean pre op hearing loss in all the three types of Tympanoplasties and the mean post op hearing levels are shown in Table 8. Majority of patients have been benefited by gaining 15.1–30 dB of hearing i.e., 38 out of 50 (76%) as shown in Table 5. Out of 50 patients, 47 patients (94%) showed excellent surgical success rate by means of graft uptake and only 3 patients had residual perforations of the Tympanic membrane as shown in Table 6. Out of 50 patients, 42 patients (86%) have come into the normal range of hearing, Only 8 patients were still lying in the range of mild deafness as shown in Table 7.
Using computer software Microsoft Excel 2007, data processing and analysis done. ‘t-test’ and ‘paired t-test’ were applied. Whenever necessary P values of <0.05 were considered to be statistically significant.
Table 8 shows types of tympanoplasty with pre op and follow up post op hearing threshold with statistical significance. There is a gain of 18.8 dB in type 1, 26.46 dB in type II and 20.27 dB gain type III tympanoplasty.
Discussion
The present study showed that there is no sex predilection for the CSOM. Out of 50 cases, 11–30 years age group people were high (80%) indicating the fact that CSOM is mainly the middle ear infection which tends to occur more in early decades of life and resolves to leave permanent perforations with conductive hearing loss in many cases. The mean age was 23.58 years.
In the present study of 50 cases, 45(90%) were of Tubotympanic type of CSOM and 5(10%) were of Atticoantral type of CSOM.
The findings were correlating with other studies, where in those studies have not included the attico-antral perforations in their study [3, 4].
It was observed that the greatest hearing loss was found in the big central perforation, whereas least in those of the anterior central perforations, which matched with other studies also [3, 4].
Yung [5] found similar findings that big central and posterior central perforation had greatest hearing loss compared to other sites of perforation. He found 43 dB HL in the series of big central and posterior central perforation as well. A postero-inferior perforation results in larger hearing loss than an antero-inferior perforation. Ahmad and Ramani [6] had also found similar findings in their study where they found 18.5 dB HL in anterior perforation and 29 dB HL in posterior perforation with 500 Hz. But they concluded: “It is seen that the difference in hearing losses between antero and postero-inferior perforations, is appreciable only at the lower frequencies”.
Therefore at the end, 46 out of 50 (92%) have come to the normal range of hearing. The mean pre op hearing loss was 42.50 dB, and the mean post op hearing was 20.41. This is due to the fact that, in all cases graft was well taken up. Four cases out of 50 (8%), in which mild deafness persisted due to the residual perforation resulting from post op infections.
Many studies on Tympanoplasty have found place in the literature with varying success rates [7–12]. It is difficult to compare these studies because of different age groups and sub groups, the definition of success; as many studies did not look at hearing outcome, the technique used and the experience level of the surgeon.
Conclusion
-
Tympanoplasty is a beneficial procedure for hearing improvement and the eradication of the disease.
-
Site of perforation affects the degree of hearing loss. Big central and central malleolar perforation having greater hearing loss than other perforation sites.
-
Though our case series is a small and follow up is only for 6 months, we tried to out lay the hearing loss pattern in CSOM cases and its improvement with Tympanoplasty surgery.
References
Sismanis A (2003) Tympanoplasty Glasscock–Shambaugh ‘surgery of the ear’, Chap 24. BC Decker Inc, Hamilton
Mills RP, Frootko NJ (1997) Management of chronic suppurative otitis media, & reconstruction of the middle ear, vol 3, Scott Brown 6th edn, Otology chapters 10, 11. Butterworth–Heinemann, London
Shrestha S, Sinha BK (2006) Hearing results after myringoplasty. Kathmandu Univ Med J 4(16):455–459
Bhusal CL, Guragain RPS, Shrivastav RP (2009) Correlation of hearing impairment with site of tympanic membrane perforation. BMC Ear Nose Throat Disord 4(9):1
Yung MW (1983) Myringoplasty: hearing gain in relation to perforation site. J Laryngol Otol 97:11–17
Ahmed S, Wand Ramani GV (1979) Hearing loss in perforations of the tympanic membrane. J Laryngol Otol 93:1091–1098
Roy Chaudhuri BK (2004) Three flap tympanoplasty—a simple and sure success technique. Indian J Otol HNS 56(3):195–200
Anand TS, Kathuria G, Kumar S, Wadhwa V, Pradan T (2004) Butterfly inlay Tympanoplasty: a study in Indian scenario. Indian J Otol HNS 54(1):11–13
Umar AS, Ahmed Z (2008) Anatomical and functional outcome following type-1 Tympanoplasty in chronic Tubotympanic suppurative otitis media, Issue 1. Military Hospital Rawalpindi, Combined Military Hospital Multan
Yuen AP, Ho WK, Hui Y, Wei WI, Au DK (2000) Correlation of pure tone audiogram results and hearing benefit of tympanoplasty for chronic suppurative otitis media. Ann Otol Rhinol Laryngol 109(4):381–384
Fukucbi I, Cerbiari DP, Garcia E, Rezende CEB, Rapoport PB (2006) Tympanoplasty: surgical results and a comparison of the factors that may interfere in their success. Braz J Otorhinolaryngol 72(2):267–272
Kakigi A, Kozakura K, Sawada S, Takeuchi S, Takeda T (2003) Renovation of surgical procedures and hearing results of type I Tympanoplasty. In: MEMRO Proceedings of the 3rd symposium, Matsuyama, Ehime, pp 421–25
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Shetty, S. Pre-Operative and Post-Operative Assessment of Hearing following Tympanoplasty. Indian J Otolaryngol Head Neck Surg 64, 377–381 (2012). https://doi.org/10.1007/s12070-011-0331-6
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12070-011-0331-6