Abstract
The term “large-vessel vasculitis” refers to chronic inflammation affecting the elastic arteries, mainly aorta and its major branches. Large-vessel vasculitis affecting the aorta is termed as “aortitis.” This leads to diffuse wall thickening, loss of elasticity, stenosis, occlusion, dissection, calcification or aneurysm formation. Vasculitis involving the aorta includes Takayasu arteritis (commonest large-vessel vasculitis in India), giant cell arteritis (GCA), the periaortitis spectrum (including inflammatory abdominal aortic aneurysm), rheumatic diseases and IgG4-related disease. It is important for physicians to be aware of the aortic manifestations of common vasculitis—so that clinically relevant aortic involvement is not missed. Also, it is equally important for surgeons to keep in mind that aortic aneurysms can have an inflammatory aetiology. The primary reason for this is the central role that immunosuppressive therapy plays in the management of inflammatory aortic aneurysms. Surgical or percutaneous interventions, when needed, are most likely to succeed when performed after activity control; perioperative steroids may be beneficial in select cases, and postoperative disease activity control is imperative.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
The term “aortitis” is used for inflammatory changes to the aortic wall from varying aetiologies. The inflammatory response may be limited to the aortic wall or accompanied by changes directly adjacent to the vessel. A distinction should be made between infectious and non-infectious aortitis. Takayasu arteritis (TA) and GCA are the most common non-infectious aortitis, with Takayasu disease being the single most important cause in India. Other causes are less common [1,2,3,4,5] (Table 1). In one prospective study from West, among 788 patients, largely elderly (mean age 72.6 ± 9.6 years) requiring surgery for thoracic aortic disease (aneurysm or dissection), 39 (4.9%) were due to histologically proven aortitis. The distribution of aetiologies in these elderly patients with an inflammatory cause was as follows: giant cell aortitis (n = 30), Takayasu arteritis (n = 1), inflammatory aneurysm (n = 3), non-specific lymphoplasmacellular aortitis (n = 2), systemic lupus erythematosus aortitis (n = 1) and Behçet syndrome (n = 1) [5].
Clinical presentation is diverse, ranging from asymptomatic disease or vague constitutional symptoms to hypertension, spontaneous dissection and aneurysm rupture. Disease activity control using steroids and immunosuppressive agents is the cornerstone of therapy for non-infectious aortitis. Interventions including ballooning, stenting or surgery are fraught with a risk of recurrence, disease manifesting in other regions of aorta on follow-up and need for re-do procedures, but are inevitable in select cases. Every effort should be made to control disease activity prior to intervention.
Takayasu Arteritis
Takayasu arteritis (aortoarteritis, pulseless disease) is a chronic, large-vessel vasculitis affecting the aorta, its major branches and sometimes pulmonary artery. The disease, though more common in Asians and Africans, has worldwide distribution. TA is usually progressive with relapses and remissions. It more commonly affects the young with a predilection for females.
The American College of Rheumatology (ACR) suggested a set of diagnostic criteria for diagnosis (Table 2) [6]. It consists of six diagnostic criteria. Three out of these six are required for diagnosis of TA.
Angiography [digital subtraction angiography (DSA), computed tomography (CT)/magnetic resonance (MR) angio] remains the gold standard for diagnosis. The differential diagnoses include other causes of non-infectious large-vessel vasculitis (Table 1), infective vasculitis (e.g., tuberculosis and syphilis) and developmental abnormalities (coarctation of aorta and Marfan syndrome). Most of these have specific features that enable diagnosis.
Etiology and pathologic features
The aetiology of TA is not clear but can best be described as a genetically predisposed T cell–mediated, autoimmune response to components of the vessel wall [7, 8]. Evidence of genetic predisposition comes from the high frequency of certain human leucocyte antigen (HLA) alleles (e.g., HLA B52) as well as some instances of familial clustering. Candidate agents that may serve as a trigger for the autoimmune response include Mycobacterium tuberculosis, streptococci, spirochetes as well as soluble antibodies of another autoimmune disease. Molecular mimicry to vessel wall from these antigens may contribute in pathogenesis.
Pathologically, the disease is caused by T cell–mediated response to vasa vasorum and other components of the wall of aorta, its large branches and in some cases the pulmonary artery. TA is a panarteritis, but it begins with granulomatous inflammation of the adventitia and outer part of tunica media (Fig. 1a, b); inflammation of the vasa vasorum is a prominent feature. Inflammatory cells include gamma delta T lymphocytes, natural killer cells, macrophages and occasional giant cells [7, 8].
a Granulomatous inflammation of descending thoracic aorta involving junction of tunica media and adventitia during active phase of TA. b Mononuclear cell infiltration of tunica media (M) and fibrosis in adventitia (A) during chronic phase of TA [images from Vaideeswar and Deshpande [8] with permission]
As the inflammation progresses to involve the full thickness of the vessel wall, there can be
-
Loss of elasticity of the aortic wall causing hypertension.
-
Luminal narrowing causing decreased perfusion distal to the stenosis and, in case of aortic narrowing, proximal hypertension.
-
Rapid or more severe inflammation leads to loss of smooth muscle cells, medial weakening, vascular dilatation and even aneurysm formation.
-
Severe intimal calcification in chronic disease.
On histopathology, the chronic phase shows patchy infiltration of tunica media with mononuclear cells and scarring (Fig. 1b); the healed phase shows fibrosis. Medial destruction results in not only vascular ectasia, but also frank aneurysms (Fig. 2). The aneurysms (saccular or fusiform) occur in 2–6%, but usually co-exist with stenotic lesions. Aneurysms devoid of stenosis or pseudo-aneurysms are extremely rare, and so are dissections [8].
a Multi-focal aortic disease with skip areas showing a large aneurysm in the abdominal aorta. The wall of the aneurysm when studied histologically also showed the presence of chronic dissection as seen in b haematoxylin and eosin (×100) and c elastic van Gieson (×100). Arrow points to the intimal flap. The wall is represented only by thickened intima (I) and adventitia (A) [images from Vaideeswar and Deshpande [8] with permission]
Although distribution as well as mode of involvement (stenotic versus aneurysmal) of different vessels that are involved is influenced by race to an extent, there is no way to predict its pattern in an individual patient. Overall, predominantly stenotic disease is far more common than aneurysmal form. There are pathologic features that may help to distinguish between giant cell arteritis and Takayasu arteritis. Aortic wall thickness is generally greater in Takayasu arteritis than in GCA. In addition, GCA is more commonly associated with inflammation that is most severe in the inner media, and GCA is not as often associated with the severe adventitial scarring seen in Takayasu arteritis. Compact granulomas are more commonly seen in Takayasu arteritis than in GCA.
Clinical features
Clinical features are determined by the stage of disease (active versus chronic), the vessels involved and the mode of involvement. In the active phase, patients may present with non-specific symptoms such as low-grade fever, malaise, muscle pain, arthralgia and carotid tenderness. Later on, affected arteries may develop stenosis, occlusion, dilatation and/or aneurysm formation. In this chronic stage, patients frequently present with signs and symptoms of diminished or absent pulses, associated with limb claudication and blood pressure discrepancies [9, 10]. Vascular bruits may be heard over the carotids, subclavian and abdominal vessels. Hypertension is common, seen in one third to over three fourths of patients in different series. It generally reflects severe renal artery stenosis, but may also be caused or contributed by thoracic aorta stenosis and a non-compliant aorta [9].
Aortic involvement
As per the angiographic classification of TA suggested by Moriwaki et al. [10], aortic branches are involved in type I; rest types II to V have some involvement of the aorta (Table 3).
Coronary or pulmonary involvement to be labelled C+ or P+, respectively.
Subclavian, carotid and renal arteries are commonly involved. In Japan, the incidence of types I and IIa is more common whereas in India, types IV and V are more common [9, 10].
Aortic involvement occurs in the form of diffuse wall thickening (causing hypertension), stenosis (Fig. 3), occlusion (Fig. 4), calcification (Fig. 5), dissection, dilatation and/or aneurysm formation [5,6,7,8]. Aortic aneurysm is a serious complication of TA. Ascending aorta is the most common site of aortic dilatation. This may further lead to aortic regurgitation. Left ventricle dysfunction and congestive cardiac failure are other serious complications and may be associated with valvular regurgitation or hypertension.
The incidence of aortic aneurysm shows wide geographic variations, but stenotic disease is universally more common than aneurysms. Studies from China show consistently lower incidence of aortic aneurysm than other regions (1 to 5% vs 13 to 45%) (Table 4) [11,12,13,14,15,16]. The presence of severe calcification is protective against aneurysm formation, while the presence of wall thickening is associated with increased risk of rupture. In most series, the incidence of aneurysm rupture in TA is low when compared with non-inflammatory aneurysms [16].
Aortic regurgitation may result from annular dilatation caused by ascending aorta and aortic root distension (Fig. 6), as well as direct inflammatory involvement of valve leaflets. Congestive cardiac failure may be associated with hypertension, aortic regurgitation and myocardial involvement; it is among the most frequent causes of death in patients of TA.
Investigations
Activity monitoring
The erythrocyte sedimentation rate (ESR) is elevated in active disease in up to three quarters of patients, but it is a poor predictor of death and acute events. High-sensitivity C-reactive protein (hs-CRP) is also commonly used to assess disease activity. It has been observed by the authors that disease progression may occur even after normalization of ESR, as evidenced by progression of angiographic disease. Pentraxin-3 has been suggested to be superior marker to ESR and CRP to assess vascular inflammation, and may be especially useful in assessing disease activity in patients on immunosuppressive therapy [9, 17]. Recently, work has focused on the role of inflammatory cytokines. Interleukin-6 and interleukin-18 are elevated in Takayasu’s disease. These may prove to be useful markers for monitoring treatment response.
Angiography
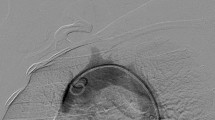
DSA of the aorta and its branches has traditionally been the gold standard method for definitive diagnostic assessment. Luminal changes range from smooth tapering stenoses to frank occlusion, and collateral vessels may be seen. DSA reduces the contrast load and helps to accurately localize stenotic or aneurysmal involvement of aorta and its branch arteries (Fig. 7). Angiography is also essential if percutaneous intervention is to be considered, for defining the site severity of lesions and for planning and performing angioplasty.
CT, MRI and PET scan
CT and magnetic resonance imaging (MRI) are important initial tools for investigating patients of TA, because they can assess luminal and mural changes, as well as angiographic appearances. They also help in planning of treatment mode. As compared with conventional angiography, a wide area of vascular lesions can be assessed and vessel wall thickness can be estimated. In the acute inflammatory stage, the wall becomes thickened, a feature not seen in normal adults.
Inflamed tissue has an increased glucose metabolism, and activity can be detected by an increased uptake of radiolabelled glucose (18FDG) in the aorta and/or its major branches. Unlike the heart, aortic wall normally does not show prominent 18FDG uptake. This modality is highly sensitive and may detect very early disease even before stenosis or aneurysms develop.
Indian perspective
The average age of the Indian patient at presentation is in the third decade. The average age of presentation at our centre was 23 years, and female-to-male ratio was 3:1. The Indian male patients with TA have a higher frequency of hypertension and abdominal aorta involvement while female patients have a tendency towards involvement of aortic arch and its branches. The incidence of aortic regurgitation has been low (7–25%) in series from India. Aortic regurgitation was seen in 10% (33) patients at our centre. In Japan, TA frequently involves the aortic arch and the branches arising from it. In contrast, abdominal aorta and its branches are frequently involved in Indian patients [9, 15]. At our centre, abdominal aorta was involved in 60% patients (198) and arch was involved in 35% (116). Both arch and abdominal aorta were involved in 5% (17) patients.
Management
Management of TA is challenging and consists of a multi-pronged approach involving activity control, medical therapy for hypertension and left ventricle dysfunction (if present). Surgical or percutaneous treatment of vascular stenosis and aneurysms may also be required as well as management of any aortic regurgitation. Monitoring and control of blood pressure may be difficult in cases with absent or reduced pulses in some extremities. Blood pressure measurements should be made in the unaffected extremities. Treatment of hypertension and congestive heart failure is done as per standard guidelines. In the presence of treatment-resistant hypertension, renal artery and thoracic aorta stenosis should be specifically looked for.
Glucocorticoids (prednisolone) and other immunosuppressives (methotrexate, azathioprine cyclophosphamide, leflunomide, mycophenolate mofetil) are the key therapy in acute inflammatory phase of TA.
Therapy with biological agents (anti-TNF agent—infliximab and monoclonal antibody against interleukin-6 (IL-6)—tocilizumab) have recently been shown to have promising results in refractory cases [18]. Revascularisation therapy is essential in uncontrolled hypertension secondary to renal artery stenosis, stenosis of aorta, symptomatic coronary ischaemia and cerebrovascular disease. Endovascular interventions have become preferable option particularly for discrete stenosis of aorta [19], renal [20], subclavian [21], carotid and other branch arteries causing severe ischemia. They should preferably be performed after control of disease activity.
Aortic dissection is a very rare manifestation of TA but is a situation where intervention cannot be postponed till activity control. A case of successful endovascular management of acute aortic dissection in a patient with TA has been recently reported [22] (Fig. 8).
Computed tomography aortogram (CTA) showing a aortic dissection (Stanford type B) of the descending thoracic aorta leading to severe narrowing of true lumen of aorta by displaced intimal flap (white arrow). Yellow circle denotes the proximal landing zone of the stent graft; here, the diameter of the aorta is 13.6 mm. b Three-dimensional (3D) reconstructed image showing aortic dissection. c Three-dimensional reconstructed image showing the completely sealed-off aortic dissection and well-expanded stent graft. d CTA at 1-year follow-up showing good expansion of stent graft and true lumen (figure from Tyagi et al [22])
Endovascular repair for descending thoracic and abdominal aorta aneurysms at risk of rupture is increasingly being used, when the lesion anatomy and branches permit.
Surgery for aortic aneurysm in TA
About 20% of patients of TA require surgery. It is indicated for the relief of ischemic symptoms during the sclerotic phase in patients not amenable to percutaneous intervention, aneurysm with risk of rupture or severe aortic regurgitation. Various surgical procedures in TA include aortocervical bypass, cervico-subclavian, aortocoronary bypass, aortoaortic bypass, aortic root replacement, renal artery bypass and nephrectomy. It is usually risky to perform surgery in a TA patient during acute inflammation because of potential of valve and graft detachment. Progressive aortic regurgitation (AR) may require surgical therapy either with valve replacement or with valve repair. Surgery in TA acute phase is difficult as the tissue is fragile and inflamed.
Vascular reconstruction in patients with TA was approached with considerable trepidation in the past, particularly during the acute phase because of fear of occlusion of the involved vessel or graft, or anastomotic disruption. However, with progressive refinements in technique and increasing experience, as well as use of hybrid (open surgical plus endovascular repair) techniques, surgery of the aortic valve, arch and other parts of aorta can now be taken up with reasonable expectations.
Yang et al. [11] recently reported their experience with 39 cases of aortic aneurysm spanning over 19 years. Twenty-three of these patients had thoracic aneurysm, 12 had abdominal aneurysm, 2 had thoraco-abdominal aneurysm, 1 had involvement of the whole aorta, and another had ascending aorta plus abdominal aorta involvement. Over two-third patients with thoracic aneurysm were symptomatic, primarily due to AR. Sixteen patients underwent aneurysm surgery at the first visit and four on follow-up. Of note, four patients were managed conservatively owing to complexity of vascular disease. One patient who had undergone Cabrol procedure died due to operative complications. All 20 aneurysm procedures done were radical replacement, and perioperative steroid therapy was used liberally. Radical surgery minimizes future risk of recurrent aneurysm and repeat surgical intervention. The benefits of perioperative steroids are widely believed to outweigh risk of accelerating aneurysm rupture and delaying wound healing [11].
In conclusion, surgical treatment of symptomatic TA by experienced surgeons is safe and effective. Symptomatic improvement and excellent long-term graft patency could be expected after arterial reconstruction. Radical surgical treatment for thoracic aortic aneurysms is highly recommended if technically possible. Effort should be made to take up the patient in quiescent phase of disease. Perioperative steroids should be considered, and postop control of disease activity as well as follow-up for possible complications like anastomotic site aneurysms is a must [11, 23, 24].
Giant cell arteritis
In the West, GCA is by far the commonest vasculitis causing aortic involvement, with annual incidence in individuals > 50 years being 15–25/100,000 in Europe [1, 2]. In India and other Eastern countries however, its frequency is much lower (< 1/100,000). Aortitis in GCA is frequently underestimated due to lack of symptoms. Thus, while earlier studies based on symptoms (mainly complications arising out of aortic involvement) found 3 to 18% of GCA patients to have aortitis, recent data based on MRI and PET scan suggests that over 50% patients of GCA have some involvement of the aorta, with a predilection for thoracic aorta. GCA confers an increased risk of both thoracic and abdominal aneurysms and of aortic dissection and/or rupture. Aortic involvement can precede cranial symptoms, be in association with cranial symptoms, or occur after the diagnosis of cranial GCA.
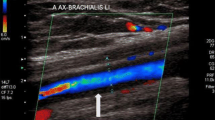
Large-vessel GCA may present in more subtle way. This type of GCA occurs more frequently in females at a younger age than those with cranial symptoms. Aortitis should be especially considered in patients with atypical clinical presentations of GCA (e.g., isolated laboratory evidence of systemic inflammation or relapse during treatment). Temporal biopsy is gold standard for cranial GCA diagnosis (Table 5). However, high-resolution colour Doppler ultrasound is non-invasive and reliable test for diagnosis. In patients with GCA, the halo sign (a hypoechoic ring around the temporal artery lumen, reflecting arterial inflammation) is very useful. Even in aorta, it shows hypoechogenic vessel wall enlargement. CT also shows hypodense vessel wall enlargement.18F-fluorodeoxyglucose positron emission tomography (FDG-PET) may have higher sensitivity for aortic involvement in GCA [1, 2, 24, 25].
The presence of aortic involvement does not affect the treatment strategy as such, unless the aortic aneurysm or regurgitation warrants surgical correction. Corticosteroids and immunosuppressive therapy form the cornerstone of treatment in GCA, irrespective of whether or not the aorta is involved. The treatment armamentarium has been enhanced with the addition of tocilizumab, a monoclonal antibody that inhibits IL-6 and has been shown to be effective in sustaining glucocorticoid-free remission up to 52 weeks [24, 25].
Patients with asymptomatic aortic involvement should be followed up long term for any delayed progression of aortic disease, leading to aortic aneurysm expansion or aortic regurgitation. The follow-up modality (echo, abdominal Doppler ultrasound or CT/MRI scan) should be individualized.
Other inflammatory diseases with aortic involvement
Aortic involvement has been described in a number of systemic rheumatic diseases (Table 1). In most cases, the primary disease is already known and awareness regarding the possibility of aortic involvement holds the key to diagnosis. Aortic arch aneurysm and/or aortic valve regurgitation are the most frequent patterns of involvement and should be specifically looked for during clinical visits. Suspicion of inflammatory aortic lesions should also be aroused if patients with underlying rheumatic disease develop features like renal or mesenteric artery occlusion or decreased perfusion to the extremities. Once clinically suspected, the extent of aortic involvement can be further delineated by CT or MR angiography. Treatment of aortitis secondary to rheumatologic diseases or other vasculitis primarily entails escalation of the already ongoing immunosuppressive therapy. Non-urgent surgical interventions for the aortic disease component should be deferred till the inflammation has been controlled [1, 2].
Chronic idiopathic periaortitis
Chronic idiopathic periaortitis [25, 26] is another distinct entity associated with aortic inflammation and aneurysm formation; it includes the spectrum ranging from inflammatory abdominal aortic aneurysm (IAAA) to idiopathic retroperitoneal fibrosis [2]. At one end of the spectrum is IAAA, where abdominal aortic aneurysm is associated with some periaortic inflammation. The disease typically affects males in the sixth to seventh decade of life. The aneurysm may develop in the course of pre-existing periaortitis or retroperitoneal fibrosis; alternately, perivascular inflammation may develop in a pre-existing degenerative aneurysm. At the other end of the spectrum is retroperitoneal fibrosis, where inflammation extends beyond the periaortic area to retroperitoneal tissue, vena cava, ureters and even duodenum. Inflammation in periaortitis (and related diseases) typically starts in the vasa vasorum, and a considerable proportion show lymphoplasmacytic infiltrates staining positive for IgG4. Abdominal IgG4-related vasculitis/periaortitis also frequently shows elevated serum IgG4 levels. The subgroup with IgG4 positivity is important to identify as these patients may develop IgG4-related diseases later on in other organ systems [1, 2].
Differentiation between inflammatory and atherosclerotic aneurysms can be made on basis of CT, MRI or even abdominal ultrasound (in addition to presence of systemic features and raised inflammatory markers during active phase). In chronic periaortitis, retroperitoneal fibrosis as well as IAAA, glucocorticoids (prednisolone 1 mg/kg/day tapered over 3–6 months) are usually effective in the presence of disease activity; steroid-sparing agents may be required in patients who are resistant or intolerant to steroids. IgG4-related disease may respond to a lower dose of steroids. Tamoxifen may have a role in retroperitoneal fibrosis while B cell depletion with rituximab may be useful in IgG4-related disease. Ureter involvement has to be managed when present; initial approach is frequently ureteric stenting as the stents can be removed when the inflammation subsides. Vascular interventions in IAAA should be restricted to aneurysm diameters exceeding 5 to 5.5 cm or rapid increase (> 1 mm/month) accompanied by clinical symptoms. Danger of rupture is similar to atherosclerotic aneurysms of equal size. Open surgery generally consists of graft inclusion with minimal dissection of surrounding structures. However, stent-graft implantation has been shown to be safe, and reduction in aortic diameter as well as periaortic fibrosis has been documented. Adequate preprocedure, periprocedure and postprocedure control of disease activity is the key to achieving improved outcomes.
IgG4-related thoracic aortitis
IgG4-related vascular lesions occur in the aorta [26, 27] and branching medium-sized arteries with or without aneurysmal change. The inflammatory lesion mainly involves the adventitia, causing remarkable adventitial fibrous thickening with infiltration of inflammatory cells. Clinical symptoms associated with IgG4-related vascular lesions might be fever, abdominal pain, hydronephrosis or few subjective symptoms. Comprehensive diagnostic criteria are applied according to image findings of thickening lesions, high serum IgG4 levels and histopathological findings. Aortic specimens yielded during aneurysm surgery should be analysed for IgG4 staining of lymphoplasmacytic cells. Diagnosis is made if ≥ 50% plasma cells in the infiltrate are expressing IgG4. As a treatment, open surgical repair or endovascular aneurysm repair is performed for the aneurysmal cases, and steroid administration is used for the cases with strong inflammation.
Conclusion
Most common causes of aortitis are Takayasu arteritis in young and GCA in older patients. Inflammatory process affects all the layers of the aortic wall. Takayasu arteritis is the most common form of aortitis in India and frequently causes stenosis of thoracic or abdominal aorta and its branches. Aneurysms have been reported in 7–25% of patients with TA and seem to mostly involve the ascending aorta followed by arch and descending thoracic aorta. Globally, giant cell arteritis is the most prevalent cause of aortitis, with evidence of some aortic involvement in up to 50% cases—though only a small number require management for the aortic disease in GCA. It commonly affects the thoracic aorta. Awareness regarding the possibility of aortic involvement in a variety of autoimmune and rheumatological diseases is the key to identifying cases with aortic involvement that require focused management. Periaortitis and IgG4-related aortic disease are other distinct, and frequently overlapping, disease processes that require tailored management. Infection should be ruled out before starting steroids in aortitis. Management of TA and GCA requires control of disease activity by steroids and/or immune suppressants. Surgical management or endovascular interventions, under the cover of immune suppressants, go a long way in managing the aneurysmal and stenotic aortic sequelae in these diseases. Symptomatic improvement and long-term graft patency should be expected after arterial reconstruction. Radical surgical treatment for large thoracic aortic aneurysms is recommended. Endovascular stent graft is a safer non-invasive option if technically feasible. Effort should be made to take up the patient in quiescent phase of disease. Perioperative steroids should be considered, and postop control of disease activity as well as follow-up for possible complications like anastomotic site aneurysms is a must.
References
Caspary L. Inflammatory diseases of the aorta. Vasa. 2016;45:17–29.
Töpel I, Zorger N, Steinbauer M. Inflammatory diseases of the aorta. Part 1: non-infectious aortitis. Gefässchirurgie. 2016;21:S80–6.
Loricera J, Blanco R, Hernández JL, et al. Non-infectious aortitis: a report of 32 cases from a single tertiary centre in a 4-year period and literature review. Clin Exp Rheumatol. 2015;33:S–19-31.
Miller DV, Isotalo PA, Weyand CM, Edwards WD, Aubry MC, Tazelaar HD. Surgical pathology of noninfectious ascending aortitis: a study of 45 cases with emphasis on an isolated variant. Am J Surg Pathol. 2006;30:1150–8.
Pacini D, Leone O, Turci S, et al. Incidence, etiology, histologic findings, and course of thoracic inflammatory aortopathies. Ann Thorac Surg. 2008;86:1518–23.
Arend WP, Michel BA, Bloch DA, et al. The American College of Rheumatology 1990 criteria for the classification of Takayasu arteritis. Arthritis Rheum. 1990;33:1129–34.
Arnaud L, Haroche J, Mathian A, Gorochov G, Amoura Z. Pathogenesis of Takayasu's arteritis: a 2011 update. Autoimmun Rev. 2011;11:61–7.
Vaideeswar P, Deshpande JR. Pathology of Takayasu arteritis: a brief review. Ann Pediatr Cardiol. 2013;6:52–8.
Tyagi S, Panja M, Sarkar PG. Challenges of Takayasu Arteritis in India. In: Wander GS, Pareek KK, editors. Medicine Update (API) 2016:, Publisher Jaypee, The Health Sciences Publisher; 26,p. 1314-1322.
Moriwaki R, Noda M, Yajima M, Sharma BK, Numano F. Clinical manifestations of Takayasu arteritis in India and Japan--new classification of angiographics findings. Angiology. 1997;48:369–79.
Yang KQ, Meng X, Zhang Y, et al. Aortic aneurysm in Takayasu Arteritis. Am J Med Sci. 2017;354:539–47.
Li J, Sun F, Chen Z, et al. The clinical characteristics of Chinese Takayasu's arteritis patients: a retrospective study of 411 patients over 24 years. Arthritis Res Ther. 2017;19:107.
Watanabe Y, Miyata T, Tanemoto K. Current clinical features of new patients with Takayasu Arteritis observed from cross-country research in Japan: age and sex specificity. Circulation. 2015;132:1701–9.
Mwipatayi BP, Jeffery PC, Beningfield SJ, et al. Takayasu arteritis: clinical features and management: report of 272 cases. ANZ J Surg. 2005;75:110–7.
Jain S, Kumari S, Ganguly NK, Sharma BK. Current status of Takayasu arteritis in India. Int J Cardiol. 1996;54:S111–6.
Kerr GS, Hallahan CW, Giordano J, et al. Takayasu arteritis. Ann Intern Med. 1994;120:919–29.
Ishihara T, Haraguchi G, Kamiishi T, Tezuka D, Inagaki H, Isobe M. Sensitive assessment of activity of Takayasu's arteritis by pentraxin3, a new biomarker. J Am Coll Cardiol. 2011;57:1712–3.
Mason JC. Takayasu arteritis—advances in diagnosis and management. Nat Rev Rheumatol. 2010;6:406–15.
Tyagi S, Kaul UA, Nair M, Sethi KK, Arora R, Khalilullah M. Balloon angioplasty of the aorta in Takayasu's arteritis: initial and long term results. Am Heart J. 1992;124:876–82.
Tyagi S, Singh B, Kaul UA, Sethi KK, Arora R, Khalilullah M. Balloon angioplasty for renovascular hypertension in Takayasu's arteritis. Am Heart J. 1993;125:1386–93.
Tyagi S, Verma PK, Gambhir DS, Kaul UA, Saha R, Arora R. Early and long-term results of subclavian angioplasty in aortoarteritis (Takayasu disease): comparision with atherosclerosis. Cardiovasc Intervent Radiol. 1998;21:219–24.
Tyagi S, Bansal A, Gupta MD, Girish MP. Endovascular management of acute aortic dissection in Takayasu Arteritis. JACC Cardiovasc Interv. 2018;11:e99–e101.
Sasaki S, Kubota S, Kunihara T, Shiiya N, Yasuda K. Surgical experience of the thoracic aortic aneurysm due to Takayasu's arteritis. Int J Cardiol. 2000;75:S129–34.
Ando M, Kosakai Y, Okita Y, Matsukawa R, Takamoto S. Surgical treatment for aortic regurgitation caused by non-specific aortitis. Cardivasc Surg. 1999;7:409–13.
Lensen KD, Voskuyl AE, Comans EF, van der Laken CJ, Smulders YM. Extracranial giant cell arteritis: a narrative review. Neth J Med. 2016;74:182–92.
Van Bommel EF, van der Veer SJ, Hendriksz TR, Bleumink GS. Persistent chronic peri-aortitis (inflammatory aneurysm’) after abdominal aortic aneurysm repair: systematic review of the literature. Vasc Med. 2008;13:293–303.
Kasashima F, Kawakami K, Matsumoto Y, Endo M, Kasashima S, Kawashima A. IgG4-related arterial disease. Ann Vasc Dis. 2018;11:72–7.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Human and animal rights
Not applicable being a review article.
Conflicts of interest
The authors declare they have no conflict of interest.
Informed consent
Not applicable being a review article.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Tyagi, S., Safal, S. & Tyagi, D. Aortitis and aortic aneurysm in systemic vasculitis. Indian J Thorac Cardiovasc Surg 35 (Suppl 2), 47–56 (2019). https://doi.org/10.1007/s12055-019-00832-z
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12055-019-00832-z