Abstract
The defect of low density lipoprotein receptor disturbs cholesterol metabolism and causes familial hypercholesterolaemia (FH). In this study, we directly delivered exogenous Ldlr gene into the liver of FH model mice (Ldlr −/−) by lentiviral gene transfer system. The results showed that the Ldlr gene controlled by hepatocyte-specific human thyroxine-binding globulin (TBG) promoter successfully and exclusively expressed in livers. We found that, although, the content of high density lipoprotein in serum was not significantly affected by the Ldlr gene expression, the serum low density lipoprotein level was reduced by 46%, associated with a 30% and 28% decrease in triglyceride and total cholesterol, respectively, compared to uninjected Ldlr −/− mice. Moreover, the TBG directed expression of Ldlr significantly decreased the lipid accumulation in liver and reduced plaque burden in aorta (32%). Our results indicated that the hepatocyte-specific expression of Ldlr gene strikingly lowered serum lipid levels and resulted in amelioration of hypercholesterolaemia.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Low density lipoprotein receptor (LDLR) is a transmembrane glycoprotein that mediates endocytosis of apoB100 and apoE-containing lipoproteins such as LDL and very low-density lipoproteins (VLDL) remnants and intermediate density lipoprotein (IDL). The lipids were then subjected to further degradation in lysosomes. Majority of cholesterol is eliminated in the circulation through the LDL receptor pathway. The defect in Ldlr gene results in disruption of cholesterol homeostasis and leads to disease such as familial hypercholesterolaemia (FH). FH is an autosomal dominant disorder, characterized by elevation of plasma LDL-cholesterol. The accumulated cholesterol accelerates deposition in the arterial wall and increases risk of premature atherosclerosis and coronary heart disease (Nair et al. 2014). Current management strategies for FH includes lifelong statins or nonstatins such as bile acid resin, niacin and fibrate treatment, as well as surgical interventions involving orthotopic liver transplantation and LDL apheresis that the blood was physically purged of LDL-cholesterol (Anedda et al. 2011; Küçükkartallar et al. 2011; Orsoni et al. 2011). However, the therapeutic efficacy of drug treatment varies depending on genetic background, especially on LDLR genotype (Elis et al. 2011). Moreover, the adverse effects in response to drugs such as liver toxicity or myopathy increases after prolonged use (Miltiadous et al. 2005). The surgical intervention methods are costly and especially, require lifelong immunosuppressant for individuals who received liver transplantation (Marais and Blom 2013).
Reconstruction of the LDLR function through gene therapy is considered an ideal strategy. Sustained expression of a therapeutic gene in specific tissues, in an appropriate amount, is one of the critical success factors for gene therapy. Liver plays a crucial role in bodily biochemical processes, where a myriad of proteins necessary for metabolism and immune response are synthesized. This makes the liver an attractive organ for gene therapy and widely used for the expression of therapeutic transgene. Recently, we demonstrated that human thyroxine-binding globulin (TBG) promoter can direct efficient and sustaining transgene expression in hepatocyte (Yan et al. 2012). In this study, liver directly delivered the exogenous Ldlr gene mediated by lentiviral vector via hydrodynamic tail vein injection and used the TBG promoter to restrict Ldlr expression in the liver of Ldlr-deficiency mice (Ldlr −/−). We further analysed the effects of Ldlr gene expression on lipoprotein profiles. The results showed that the treatment dramatically lowered serum LDL cholesterol and reduced vascular lesion.
Materials and methods
Cloning and lentivirus preparation
Murine Ldlr cDNA (GenBank: NM_010700.3) was amplified and inserted into human immunodeficiency virus (HIV)-based lentiviral pLVX-Puro vector (Clontech, Mountain View, USA). A 400-bp hepatocyte-specific TBG promoter was cloned upstream of Ldlr coding sequence to replace the cytomegalovirus (CMV) promoter. The resulting recombinant lentiviral vector, pLV-TBG-Ldlr was then confirmed by sequencing. For virus production, the overnight incubated 293T cells were transfected with 7 μg of pLV-TBG-Ldlr plasmid along with 36 μL of Lenti-X HTX Packaging Mix (Clontech) following instructions from the manufacturer. The medium was replaced with complete culture medium, Dulbecco’s modified Eagle’s medium (DME) (Invitrogen, Carlsbad, USA) containing 10% FBS, 6 h after transfection. Forty-eight hours later, the supernatant of transfectant was collected by centrifugation at 15000 rpm for 20 min and filtered through a 0.45- μm pore-size cellulose acetate filter (Whatman, Maidstone, UK). The titers of lentivirus determined by qRT-PCR were 2×108 TU/mL. The lentiviral particles were stored at −80°C for further infection at optimum titer.
Cell culture and transduction
One day before transduction, the H22 cells were seeded in 6-well plate at 2×105 cells per well and cultured in DMEM containing 10% FBS, 100 U/mL penicillin and 100 U/mL streptomycin at 37°C with 5% CO2. Viral supernatant and polybrene (4 μg/mL) (Sigma-Aldrich, St Louis, USA) were added into the medium. After transduction for 8 h, the virus-containing medium was discarded and replaced with fresh growth medium. The cells were then cultured for additional 24 h to reach 80–90% confluence. Finally, the cells were harvested for analysis or selected using the puromycin (900 μg/mL, Sigma-Aldrich) to obtain stably transfected cell clones.
Enzyme-linked immunosorbent assay (ELISA)
The total cellular protein was isolated and diluted with blocking solution containing 2% bovine serum albumin. A sandwich ELISA was used to determine LDLR level (R&D system, Minneapolis, USA). The assays were performed according to the manufacturer’s instructions. Finally, the optical density of each well was determined using a microplate reader at 450 nm.
Quantitative RT-PCR
Five days after transfection, the mice were anesthetized and sacrificed. Total RNA was extracted from liver, lung, heart, spleen, kidney and intestine by TRIzol reagent (Invitrogen). Aliquots of 1 μg total RNA was reverse transcribed into cDNA using M-MLV reverse transcriptase (Promega, Madison, USA) and oligo (dT) primers. The synthetic cDNA was subsequently used as template, and real-time quantitative RT-PCR was performed on the Applied Biosystem 7500 Real Time PCR System using SYBR green PCR Master mixture (Stratagene, La Jolla, USA) with the primers specific for Ldlr gene. The results were normalized to mouse Gapdh gene (GenBank ID: NM_008084) and relative LDLR mRNA abundance was calculated using the 2−ΔΔCT method. For each sample, the data were verified at least in triplicate and averaged.
Western blot
Protein was extracted from liver and quantified using the BCA method. The 10–20 μg protein was loaded on a 12% SDS-PAGE gel and separated by electrophoresis. After transferred to an immobilon-Nc membrane and blocked in TBST (20 mM Trisbase, pH 7.6, 150 mM NaCl, 0.1% Tween 20) containing 5% nonfat milk for several hours, the membrane was incubated with primary antibodies against LDLR (1 : 200 dilution, Santa Cruz Biotechnology, Santa Cruz, USA) in blocking solution overnight at 4°C followed by washing thrice at 15 min intervals with TBST. The membrane was further incubated with horseradish peroxidase-conjugated secondary antibodies (1 : 5000 dilution, Santa Cruz). After additional washing, HRP activity was detected by enhanced chemiluminescence (ECL) (Byotime Bio., Nantong, China) according to the manufacturer’s instructions.
Animal studies
All procedures were approved by the Animal Care and Use Committee of Guizhou Medical University, and performed according to the Care and Use of Laboratory Animals published by the US National Institutes of Health. Ldlr −/− mice on C57BL/6J background were originally obtained from the Jackson Laboratory (Bar Harbor, USA), which were maintained in a pathogen-free barrier facility under 20–22°C temperature, 12-h light/dark cycle conditions. The animals were kept on standard diet before the age of four weeks and then received a western-type diet (WTD) (21% fat, 0.15% cholesterol; Tengxin Bio Inc., Chongqing, China) for 12 weeks to induce hypercholesterolaemia. After induction, the mice were randomized into either a control group or intervention group (n = 12 for each group). For intervention group, mice were anesthetized and received 200 μL lentiviral particles (2×108 TU/mL) of pLV-TBG-Ldlr via hydrodynamic tail vein injection. Animals were then allowed to recover and were kept before they were sacrificed.
Plasma lipid analyses
After fasting overnight, the blood samples were collected from retro-orbital venous plexus of anesthetized mice. Plasma was separated by centrifugation. Total cholesterol, triglycerides and lipoproteins in plasma were determined using an enzymatic assay (Jiancheng, Nanjing, China) following the manufacturer’s instructions.
Measurement of atherosclerotic lesion
The mice were euthanized and aortas from the proximal aortic arch to the thoracic artery were dissected. The samples were subsequently fixed overnight with formaldehyde. After removing the adventitial fat, the aortas were split longitudinally and stained with oil Red O (Sigma-Aldrich) for 1 h. Finally, they were pinned en face and photographed. The total arterial surface area and total lesion area were determined using Image-Pro Plus. The extent of lesion development was calculated as percentage of oil red O positive areas.
Statistical analysis
The data were expressed as mean ± standard error of the mean (SEM), and were analysed using SPSS program. Paired statistical analysis was done using student’s t-test. P < 0.05 was considered statistically significant.
Results
Ldlr gene expression in H22 cells
We generated the recombinant lentiviral vector pLV-TBG-Ldlr in which the Ldlr gene was controlled by hepatocyte- specific TBG promoter. To characterize the vector, H22 hepatic cells were transfected after virus package. The cells were harvested 48 h later and subjected to LDLR measurement. ELISA results showed that 126 μg/mg LDLR was produced in transfected cells which was two-fold higher than that expressed in untransfected cells (56 μg/mg) (figure 1a). Lentivirus can mediate foreign DNA integration into host genome resulting in stable expression of transgenes. Therefore, we detected the LDLR level at different time point to investigate the long-term performance of pLV-TBG-Ldlr. Although, the LDLR expression was slightly lower than levels at 48 h and 10 days, we obtained 120 μg/mg LDLR from transfected cells at 30 days, which is dramatically higher compared to the expression in untransfected cells (56 μg/mg) (P < 0.05) (figure 1b). These results demonstrated that the exogenous LDLR could effectively and sustainedly express in H22 cells at least for 30 days.
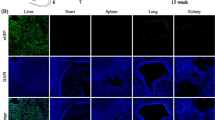
Ldlr gene specific expression in liver
To explore the expression of LDLR in vivo, the lentiviral pLV-TBG-Ldlr was injected into Ldlr −/− mice via tail vein. Five days after injection, livers were isolated and subjected to analysis by Western blot. We detected the LDLR expression in livers. In contrast, there were no detectable LDLR in the untreated mice (figure 2a). Next, the liver, lung, heart, spleen, kidney and intestine were dissected from treated Ldlr −/− mice, and LDLR mRNA abundances were measured by qRT-PCR. The result showed that a great amount of LDLR was expressed in liver. However, we could not identify measurable LDLR mRNA in other tissues such as lung, heart, spleen, kidney and intestine, which indicated that the TBG promoter controlled foreign Ldlr gene exhibited hepatocyte-specific expression (figure 2b).
Expression of Ldlr lowered lipid levels in serum
To determine the physiological effects of Ldlr expression in mice, the plasma from treated Ldlr −/− mice were collected and the total cholesterol (TC), triglycerides (TG), low density lipoprotein (LDL) and high density lipoprotein (HDL) were assayed. All the levels in the infected mice showed significantly lower than those in control Ldlr −/− mice except HDL. Among them, LDL level was strikingly reduced, amounted to 46%. Additionally, there was a 30 and 28% decrease in TG and TC, respectively, compared to uninjected mice. The HDL cholesterol displayed no significant changes after the LDLR expression and almost remained the same as in untreated mice (table 1). The results indicated that the production of Ldlr gene functioned well in vivo and resulted in effective amelioration of hypercholesterolaemia.
Expression of Ldlr decreased lipid accumulation in liver and reduced aortic plaque formation
To evaluate the lipid accumulation in tissues, liver cryosections from Ldlr −/− mice injected with Ldlr were stained with oil red O. We found that the liver section appeared smoother and showed less lipid accumulation (figure 3, a & b), while obvious lipid droplets were observed in the untreated groups. The evidences indicated the liver-directed expression of Ldlr facilitated decrease in cholesterol retention in livers and therefore improved cholesterol metabolism in Ldlr −/− animal. To further investigate the effects of Ldlr expression on plaque formation, we stained en face preparations of aortas from the proximal aortic arch to the thoracic artery with oil red O, and quantified the positive plaque accumulated at intima surface which revealed a 32% reduction in plaque area in Ldlr-expressed mice compared with untreated controls (figure 3, c–e).
Decreasing lipid accumulation in liver and reduced lesion sizes in aortas after Ldlr expression. (a, b) Liver cryosections from pLV-TBG-Ldlr injected mice and untreated control mice were stained with oil red O (×100). (c, d) En face preparations of aortas from the aortic arch to descending thoracic aorta dissected from Ldlr expression and control mice stained with oil red O. (e) Quantitative assessment of lesion area, expressed as percentage of atherosclerotic area / total area of the aorta. * P < 0.05, compared with controls.
Discussion
In blood, lipids transport in the form of lipoprotein complexes composed of proteins and lipids. The serum lipoproteins are classified according to their density chemical qualities which include chylomicron (CM), VLDL, LDL and HDL. The CM and VLDL are primarily rich in triglyceride, while LDL and HDL are rich in cholesterol. CM, VLDL and LDL contain a larger proportion of lipids and such excessive lipoprotein will be deposited in the aortas walls, which potentially causes atherosclerosis, myocardial infarction, stroke or other cardiovascular diseases. HDL carries the least amount of lipid with the highest proportion of protein and functions in reverse cholesterol transport in which excess cholesterol is transported by HDL back to the liver for breakdown and excretion, thus reducing the risk of cardiovascular diseases. The results of this study showed that the hepatic expression of Ldlr gene in hypercholesterolaemia mice sharply reduced the levels of triglyceride and LDL-cholesterol, while less affected the HDL cholesterol level which suggested that the treatment normalized the lipid profile and improved the cholesterol metabolism.
Selection of an ideal gene transfer system is a key step in gene therapy. Several viral vectors including adenovirus, lentivirus and adeno-associated virus (AAV), which are able to efficiently introduce foreign DNA into a wide range of cells, have been routinely used in gene therapy. Owing to large capacity for foreign DNA and easy to prepare high titer, the replication-defective adenovirus has become a common tool for delivery of therapeutic genes (Lugenbiel et al. 2012; Westphal et al. 2013; Uchida et al. 2014; Zeng et al. 2014). However, as a nonintegrative delivery system, adenoviral vectors can only allow transient episomal expression of foreign genes in the host cells which results in lost of transgenes expression overtime by dilution in dividing cells or degeneration in nondividing cells. Unlike adenovirus, AAV can mediate foreign DNA integration in host genome. However, the limited capacity and complicated procedures of virus packaging hamper its wider use (Tal 2000). Although, the wild-type AAV shows specific integration in chromosome 19, the integration of replication-defective AAV into host genome is random (Kaeppel et al. 2013). The lentiviral vector that derived from HIV can infect transient and dividing cells. Importantly, the integration property of lentiviral vector can confer transgene persistent expression in host organism. However, like the modified AAV, lentivirus also displays random integration which increases the risk of insertional mutagenesis (Ranzani et al. 2013). Obviously, a delivery system that not only efficiently introduce foreign DNA into host cells but also mediates the DNA targeted integration into precise locations is highly desired in gene therapy. Therefore, the use of virus-based delivery system combined with some site-specific recombinases, such as phiC31 integrase or artificial enzymes, such as transcription activator-like effector nuclease is possibly a promising strategy for the future.
To achieve higher therapeutic efficacy, the constitutive promoters such as CMV and elongation factor 1 α (EF1 α) were commonly used to direct the foreign genes in gene therapy. However, the whole tissue expression by such promoters make the regulation of therapeutic gene deviate from its original site, which leads to their expression almost impossibly at physiological levels. Further, these kind of promotes are not capable of restricting gene expression in desirable cells and potentially bring adverse effects in gene therapy. Especially, the risk of immune response will possibly increase when the therapeutic gene ectopically expresses in a particular cell type like dendritic cells. It was demonstrated that TBG promoter facilitates specific and persistent transgene expression in liver (Yan et al. 2012). Moreover, the activity is proved to be slightly less than CMV and EF1 α, but far greater than other hepatocyte-specific promoters such as apoE and CYP2E1 promoters. The TBG promoter has been increasingly and successfully applied in correction of genetic diseases such as mucopolysaccharidosis, muscular dystrophy and methylmalonic acidaemia (Carrillo-Carrasco et al. 2010; Bish et al. 2011; Cotugno et al. 2011) and demonstrated to be efficient in treating FH in this study.
Liver-directed gene transfer is an efficient strategy for delivering therapeutic genes into hepatocyte. However, the efficiency of gene transfer to hepatocytes is influenced by the size of fenestrae. The fenestrae are clustered into sieve plates in sinusoidal endothelial cells, which line the hepatic sinusoids and form a wall called endothelium to separate the hepatocytes or parenchymal cells from bloodstream. The sinusoidal endothelial cells filter the fluids and exchange between the sinusoid and the space of Disse through fenestrae. Therefore, the diameter of fenestrae is a determinant for passage of viral particles from the sinusoidal lumen to the surface of hepatocytes. It is reported that the diameter of fenestrae varied among species and exhibits considerably smaller in humans (107 nm) than that in C57BL/6 mice (141 nm) (Wisse et al. 2008; Jacobs et al. 2010). More importantly, the HIV-1-derived lentiviral vector was measured to be 150 nm in diameter, which is much larger compared with other viral particles such as adenoviral vectors (93 nm) and AAV (22 nm) (Snoeys et al. 2007; Jacobs et al. 2010). Therefore, the lentivirus delivery system is potentially restricted the passage by the size of human sinusoidal fenestrae, which will be a big challenge when applied in possible clinic trials.
In the current study, the LDL was reduced by 46% by Ldlr gene transfer in FH model mice. Two impressive reports suggest that the classical gene transfer with Ldlr can result in even higher efficacy in lowering serum cholesterol with 95% decrease in nonHDL cholesterol and 77% in total cholesterol, respectively (Kassim et al. 2010; Van Craeyveld et al. 2011). Further, both the studies revealed that the treatment induced marked regression of atherosclerotic lesion. Notably, the delivery of Ldlr system in those studies is respectively through adenoviral and AAV vector rather than the lentiviral vector used in our study (Kassim et al. 2010; Van Craeyveld et al. 2011). Therefore, whether the high potency of therapeutic outcome is due to the gene delivery strategy needs further investigation; and it will guide us to optimize the vector system.
In conclusion, the TBG promoter-directed exogenous Ldlr gene mediated by lentiviral vector system expressed specifically and efficiently in livers in FH model mice. We showed that the treatment restored LDL receptor function and led to drastic reduction in serum cholesterol level, which decreased lipid storage in the liver and prevented the development of atherosclerosis.
References
Anedda S., Mura S., Marcello C. and Pintus P. 2011 HELP LDL-apheresis in two cases of familial hypercholesterolemic pregnant women. Transfus. Apher. Sci. 44, 21–24.
Bish L. T., Sleeper M. M., Forbes S. C., Morine K. J., Reynolds C., Singletary G. E. et al. 2011 Long-term systemic myostatin inhibition via liver-targeted gene transfer in golden retriever muscular dystrophy. Hum. Gene Ther. 22, 1499–1509.
Carrillo-Carrasco N., Chandler R. J., Chandrasekaran S. and Venditti C. P. 2010 Liver-directed recombinant adeno-associated viral gene delivery rescues a lethal mouse model of methylmalonic acidemia and provides long-term phenotypic correction. Hum. Gene Ther. 21, 1147–1154.
Cotugno G., Annunziata P., Tessitore A., O’Malley T., Capalbo A., Faella A. et al. 2011 Long-term amelioration of feline mucopolysaccharidosis VI after AAV-mediated liver gene transfer. Mol. Ther. 19, 461–469.
Elis A., Zhou R. and Stein E. A. 2011 Effect of lipid-lowering treatment on natural history of heterozygous familial hypercholesterolemia in past three decades. Am. J. Cardiol. 108, 223–226.
Jacobs F., Wisse E. and De Geest B. 2010 The role of liver sinusoidal cells in hepatocyte-directed gene transfer. Am. J. Pathol. 176, 14–21.
Kaeppel C., Beattie S. G., Fronza R., van Logtenstein R., Salmon F., Schmidt S. et al. 2013 A largely random AAV integration profile after LPLD gene therapy. Nat. Med. 19, 889–891.
Kassim S. H., Li H., Vandenberghe L. H., Hinderer C., Bell P., Marchadier D. et al. 2010 Gene therapy in a humanized mousemodel of familial hypercholesterolemia leads to marked regression of atherosclerosis. PLoS One 5, e13424.
Küçükkartallar T., Yankol Y., Kanmaz T., Topaloğlu S., Acarli K. and Kalayoglu M. 2011 Liver transplantation as a treatment option for three siblings with homozygous familial hypercholesterolemia. Pediatr. Transplant. 15, 281–284.
Lugenbiel P., Bauer A., Kelemen K., Schweizer P. A., Becker R., Katus H. A. and Thomas D. 2012 Biological heart rate reduction through genetic suppression of G α(s) protein in the sinoatrial node. J. Am. Heart Assoc. 1, jah3-e000372.
Marais A. D. and Blom D. J. 2013 Recent advances in the treatment of homozygous familial hypercholesterolaemia. Curr. Opin. Lipidol. 24, 288–294.
Miltiadous G., Xenophontos S., Bairaktari E., Ganotakis M., Cariolou M. and Elisaf M. 2005 Genetic and environmental factors affecting the response to statin therapy in patients with molecularly defined familial hypercholesterolaemia. Pharmacogenet. Genomics 15, 219–225.
Nair D. R., Sharifi M. and Al-Rasadi K. 2014 Familial hypercholesterolaemia. Curr. Opin. Cardiol. 29, 381–388.
Orsoni A., Saheb S., Levels J. H., Dallinga-Thie G., Atassi M., Bittar R. et al. 2011 LDL-apheresis depletes apoE-HDL and pre- β1-HDL in familial hypercholesterolemia: relevance to atheroprotection. J. Lipid Res. 52, 2304–2313.
Ranzani M., Cesana D., Bartholomae C. C., Sanvito F., Pala M., Benedicenti F. et al. 2013 Lentiviral vector-based insertional mutagenesis identifies genes associated with liver cancer. Nat. Methods 10, 155–161.
Snoeys J., Lievens J., Wisse E., Jacobs F., Duimel H., Collen D. et al. 2007 Species differences in transgene DNA uptake in hepatocytes after adenoviral transfer correlate with the size of endothelial fenestrae. Gene Ther. 14, 604–612.
Tal J. 2000 Adeno-associated virus-based vectors in gene therapy. J. Biomed. Sci. 7, 279–291.
Uchida D., Shiraha H., Kato H., Nagahara T., Iwamuro M., Kataoka J. et al. 2014 Potential of adenovirus-mediated REIC/Dkk-3 gene therapy for use in the treatment of pancreatic cancer . J. Gastroenterol. Hepatol. 29, 973–983.
Van Craeyveld E., Gordts S. C., Nefyodova E., Jacobs F. and De Geest B. 2011 Regression and stabilization of advanced murine atherosclerotic lesions: a comparison of LDL lowering and HDL raising gene transfer strategies. J. Mol. Med. 89, 555–567.
Westphal M., Ylä-Herttuala S., Martin J., Warnke P., Menei P., Eckland D. et al. 2013 Adenovirus-mediated gene therapy with sitimagene ceradenovec followed by intravenous ganciclovir for patients with operable high-grade glioma (ASPECT): a randomised, open-label, phase 3 trial. Lancet Oncol. 14, 823–833.
Wisse E., Jacobs F., Topal B., Frederik P. and De Geest B. 2008 The size of endothelial fenestrae in human liver sinusoids: implications for hepatocyte-directed gene transfer. Gene Ther. 15, 1193–1199.
Yan Z. H., Yan H. and Ou H. L. 2012 Human thyroxine binding globulin (TBG) promoter directs efficient and sustaining transgene expression in liver-specific pattern. Gene 506, 289–294.
Zeng H., He X., Hou X., Li L. and Chen J. X. 2014 Apelin gene therapy increases myocardial vascular density and ameliorates diabetic cardiomyopathy via upregulation of sirtuin 3. Am. J. Physiol. Heart Circ. Physiol. 306, 585–597.
Acknowledgements
This study was supported by Guizhou Science and Technology Funds (no. 2012GZ81781) and the National Natural Science Foundation of China (no. 81460277).
Author information
Authors and Affiliations
Corresponding author
Additional information
[Ou H., Zhang Q. and Zeng J. 2016 Improving lipoprotein profiles by liver-directed gene transfer of low density lipoprotein receptor gene in hypercholesterolaemia mice. J. Genet. 95, xx–xx]
Rights and permissions
About this article
Cite this article
OU, H., ZHANG, Q. & ZENG, J. Improving lipoprotein profiles by liver-directed gene transfer of low density lipoprotein receptor gene in hypercholesterolaemia mice. J Genet 95, 311–316 (2016). https://doi.org/10.1007/s12041-016-0636-z
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12041-016-0636-z