Abstract
Acute myocardial infarction (AMI) is a heart lesion, that endangers the life safety of patients. This study focused on exploring the clinical effect of miR-542-3p on AMI and no-reflow after percutaneous coronary intervention (PCI). Serum samples were collected from 100 AMI emergency inpatients. The expression of miR-542-3p was quantified by qPCR. The predictive role of miR-542-3p was disclosed by plotting ROC curve. In addition, AMI subjects were cataloged into a group of no-reflow and normal reflow group. The risk factors of no-reflow were estimated by logistic regression analysis. In the serum samples of AMI patients, the level of miR-542-3p showed a pattern of decreasing. MiR-542-3p expression represented a high sensitivity and specificity of the prediction of AMI. A decrease of miR-542-3p content was revealed in AMI patients without reflow after PCI. Logistic regression results reflected that miR-542-3p was an independent biomarker for no-reflow. The declined miR-542-3p expression was a predictive marker for AMI and no-reflow in AMI patients.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Acute myocardial infarction (AMI) has become an important cause of increased mortality in cardiovascular diseases [1]. AMI is mainly caused by the formation of blood clots in the coronary arteries, resulting in the occlusion of the vascular lumen [2]. Acute ST-segment elevation myocardial infarction (STEMI) refers to persistent and severe myocardial ischemia caused by coronary artery occlusion, which eventually leads to acute myocardial death. For AMI patients, rapid opening of the infarction-related artery is the most important and key means of its treatment [3]. The survival rate of patients with AMI is determined by the opening time of the infarct-related artery and the recovery of myocardial and microcirculation in the infarct-related area [4]. Urgent percutaneous coronary intervention (PCI) is a routine surgical treatment accepted as a crucial treatment for patients with AMI [5]. PCI can rapidly open the IRA and restore coronary blood flow of patients [6]. No reflow or slow reflow occurs in 2.3–41% of patients with AMI undergoing PCI [7]. The no-reflow situation after PCI is involved in a poor clinical prognosis. No reflow is often accompanied by complications such as infarct extension, ventricular remodeling, malignant arrhythmia, and cardiac dysfunction, which increases the incidence of heart failure [8]. Therefore, the primary clinical task is to find more indicators to indicate no-reflow and to guide effective treatment.
MiRNA is a newly discovered non-coding protein, which plays its biological function through the expression of post-transcriptional regulatory genes. MiRNAs can remain stable in different environments, such as high temperature, changing value, and repeated freezing and thawing, which provides the possibility of circulation for clinical diagnosis and assessment of disease [9]. There are a variety of abnormal circulating expressions in AMI, among which, miR-142, miR-17-5p, and miR-145, have been expected to be specific for the prediction of myocardial infarction [10, 11]. In patients with AMI, blood levels of miR-122 and miR-22 are measured and found to be dramatically altered in the acute phase of patients, suggesting a new marker of possible diagnosis [12]. Plasma levels of miR-19b-3p, miR-134-5p and miR-186-5p increase in the early phase of AMI, and their combination shows a high efficacy on AMI [13]. In a hypoxia/reoxygenation model, the content of miR-542-3p is declined, and it ameliorates the damage of cardiomyocytes [14], providing the correlation between this miRNA and myocardial disease. Another publication explores the roles of miR-542-3p in coronary heart disease and certified miR-542-3p participates in the accommodation of Chinese traditional medicine on this disorder by enhancing the oxidation and inflammatory response [15]. Therefore, clinical studies on miR-542-3p in human thrombotic cardiovascular diseases may provide a new idea for the prevention and diagnosis.
We suppose that miR-452-3p may be related to AMI and its expression is altered with the occurrence of AMI in patients. By comparing the changes of miR-542-3p in patients with AMI and control individuals, this study explored the possible value of miR-542-3p in the diagnosis of patients with AMI. Additionally, the patients were cataloged into no-reflow group and normal group after the PCI operation. The predictive significance of miR-542-3p for no-reflow was estimated.
Materials and Methods
Research Object and Grouping
A total of 100 STEMI patients within 12 h in The Affiliated Hospital of Xuzhou Medical University from October 2019 to June 2022 were included in the study. Inclusion criteria were: (1) Patients with typical symptoms of angina pectoris, such as squeezing or tightening of the anterior chest and shortness of breath after activity; (2) Patients whose electrocardiogram indicated previous ST-segment changes; (3) increases in myocardial marker levels; (4) Imaging evidence suggests new local abnormal wall motion or loss of viable myocardium. Meanwhile, 101 age- and gender-matched subjects who had chest pain but with no AMI during the same period were randomly selected as the control group. Coronary angiography was conducted in 101 controls to exclude coronary heart disease. All subjects including patients and controls with a history and clinical features of infectious disease, auto-immune, malignant tumor, peripheral vascular disease, lung diseases, hepatic or hematologic disorders, or chronic renal failure requiring dialysis were excluded from the present study. This project followed the tenets of the Declaration of Helsinki and was reviewed by the ethics committee of the hospital (XYFY2019-KL005). All patients provided signed the informed consent for the project study.
All patients underwent physical examination, and collected basic clinical information. The venous blood of all patients was collected within 12 h after admission. After stirring and centrifugation in anticoagulant vessel, serum was acquired.
Treatment of PCI
Patients were given enteric-coated aspirin 300 mg, atorvastatin 80 mg, and clopidogrel 600 mg orally before emergency PCI. Electrocardiograph monitoring and arterial pressure monitoring were performed routinely during the operation. Coronary angiography (CAG) was performed using a coronary angiography tube through the right radial artery approach to identify the location and number of coronary artery lesions and infarct-related arteries. The guide catheter was placed at the opening of the corresponding coronary artery, and the guide wire was sent to the distal end of the vascular lesion. Thrombus aspiration was performed when necessary, and balloon pre-dilation was performed or not.
Thrombolysis in myocardial infarction (TIMI) blood flow grading method was used to evaluate the occlusion and opening degree of occlusion-related vessels. According to the situation of patients after PCI, patients were included into normal blood flow group (TIMI = 3) and the no-reflow group (TIMI ≤ 2). The blood was isolated after 48 h of PCI therapy.
MiR-542-3p Expression Evaluation
A miRNA (TIANGEN, Beijing, China) extraction kit was utilized to extract RNA from serum samples as per the instructions. The prepared serum specimens were defrosted and removed to the corresponding new tube with lysate. The homogenate stood at room temperature for 5 min. Chloroform was added separately to each sample tube, anhydrous ethanol, protein removal solution, bleach solution, and water to obtain RNA solution. Single strand synthesis using reverse transcription kit (TIANGEN, Beijing, China) and the total sample. In this experiment, the relative quantitative analysis of the expression level of the miR-542-3p is carried out systematically, and the internal parameter is U6. Upstream primers and downstream primers were provided by Guangzhou Ruibo Company (China). In each reaction system of qPCR, there is 4 µl cDNA, 10 µl SYBR master mix, 0.4 µl burn dye mixture, water, and upstream and downstream primers. The amplification strips of the reaction were: pre-denaturation, then denaturation, annealing, and extension, and the specific operations were carried out according to the kit manual. Relative levels were calculated using the relative expression of genes formula 2−∆∆CT.
Statistical Method
SPSS Software was applied in statistical analysis. The measurement data of the clinical characteristics of the AMI group and the control group were expressed as mean ± standard deviation and were measured between the two groups by t-test. The count data were compared by χ2 test, and the P value was calculated. The receiver operating characteristic (ROC) curve was drawn. Logistic regression analysis was used to measure the correlation between miRNA levels in AMI. A statistically significant difference was considered by P < 0.05.
Results
General Clinicopathological Data
The demographic information and chronic disease data were recorded. A total of 100 patients included 47 males and 53 females. As can be seen from Table 1, the baseline information in the two groups, including gender, average age, BMI, combined hypertension, combined diabetes, and hyperlipidemia showed no dramatic difference (P > 0.05).
Predictive value of Serum miR-542-3p for AMI Patients
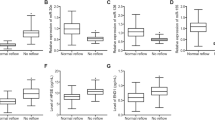
The serum miR-542-3p was compared in AMI group and the control group. As expressed in Fig. 1, the content of miR-542-3p declined compared with controls (Fig. 1, P < 0.001), reflecting that AMI connected to the reduction of miR-542-3p expression.
To explore the predictive value of miR-542-3p for AMI, the ROC was plotted using the serum expression level of miR-542-3p of all enrolled individuals. The area under the curve (AUC) was 0.931 (Fig. 2), lending evidence that miR-542-3p was an indicator of diagnosing AMI. When the cut-off value is optimal, the corresponding sensitivity and specificity were 80.00% and 87.13%, as shown in Fig. 2.
Expression of miR-542-3p in Groups of Normal Flow and No-Reflow
Considering the TIMI grade, 20 cases were cataloged in no-reflow group, and 80 cases with normal blood flow after PCI treatment. Serum miR-542-3p content in patients with no-reflow decreased dramatically, and the difference was statistically significant compared with that of normal group (Table 2, 0.27 ± 0.061 versus 0.62 ± 0.14). The abnormal content of miR-542-3p in patients with no-reflow indicated that miR-542-3p might be correlated with the prognosis of AMI.
Comparison of Clinical Characters Between the Two Groups After PCI
The comparison of clinical information and characteristics of coronary angiography in groups of the no-reflow and normal group is shown in Table 2. Demographic data and chronic diseases were not different between the two groups (Table 2, P > 0.05).
The patients vascular status and scoring system are cataloged in Table 2. The results indicated that there was no statistical difference in culprit vessel type between the no-reflow group and the normal blood flow group (P > 0.05). The number of diseased vessels was decreased in a group with normal blood flow group (P < 0.05). Additionally, culprit vessel length and onset to the culprit vessel opening time declined in the normal blood flow group compared to the group without reflow group (P < 0.05). The secretion of D-dimer and NT-proBNP was diminished in group with normal blood flow (P < 0.001). The percentage of patients in II and III levels of Killip grade and high risk of TIMI risk score was increased in the group without reflow group (P < 0.05).
Independent Risk Tool for Patients With No-Reflow
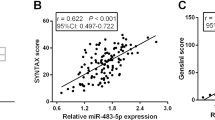
The above indexes with differences in Table 2 and miR-542-3p levels were arranged and expressed in the multivariate logistic model. As documented in Table 3 and forest plot in Fig. 3, NT-proBNP (OR: 0.262, 95% CI: 0.070–0.981) and miR-542-3p (OR: 0.140, 95% CI: 0.029–0.671) were independent risks for AMI patients without reflow after PCI surgery (Table 3, P < 0.05).
Discussion
As a common heart disease, AMI has manifestations of rapid onset, quick progress, and poor mortality [16]. Once it comes on, it will endanger the life safety of patients. AMI Acute necrosis of myocardial tissue due to sustained severe ischemia. Early diagnosis improves survival and long-time prognosis in patients with AMI [17]. Patients with AMI need to be diagnosed as soon as possible, and further treatment plans should be decided according to the time of myocardial infarction. Early treatment is closely involved in the good prognosis of patients. Currently, clinically diagnosed serum biomarkers mainly include creatine kinase isoenzyme, myoglobin, and myoglobin [18]. Although the above markers have reached certain levels in the sensitivity and specificity of early diagnosis, sensitivity and specificity are often not insufficient, researchers continue to study new serum markers with high sensitivity and specificity, especially for good serum markers that can reflect the prognosis of patients. Thus, this investigation focus on searching for a novel clinical biomarker. MiRNAs exert their biological impacts by horizontally regulating the expression of boot genes, and thus participate in the maintenance of various physiological functions in the body [19]. MiR-17-3p, miR-190-5p, and miR-202-5p are closely correlated to myocardial ischemia–reperfusion damage, and their expression is abnormal in this dysfunction [20,21,22]. Altered miR-223 expression is a mediator of cardiac hypertrophy, thus correlating with the pathogenesis of the cardiac disease [23]. Circulating miR-22-5p, miR-132-5p, and miR-150-3p are raised in patients with AMI [24]. These above statements that miRNAs are involved in cardiovascular diseases.
MiR-542-3p associates with cardiac development and pathologic mechanisms. In an analysis of expression profile in heart failure, miR-542-3p may act as a key gene in ischemic cardiomyopathy [25]. Lu et al. certify that the concentration of miR-542-3p is declined in cardiomyocyte damage [14]. In this experiment, serum samples were collected from AMI patients and normal control subjects, and a serum level of miR-542-3p was detected by quantitative method. It was found that level of miR-542-3p in patients with AMI was diminished, verifying that miR-542-3p was implicated in AMI. Many miRNAs are applied as indicators for risk prediction. Serum miR-199a, miR-146, and miR-26a are overexpressed in AMI patients and the authors indicate these miRNAs may be beneficial for the prediction of AMI [26]. MiR-19a is proven to be an appropriate predictive biomarker for patients with AMI with high efficacy [27]. Current study enrolled the miR-542-3p expression to plot the ROC curve. The AUC and efficacy analysis results reflected that low expression of miR-542-3p was of certain predictive value for AMI.
PCI is the primary treatment for revascularization after AMI, clinically, PCI is often used to treat AMI, which can quickly open the blocked coronary artery, promote the rapid recovery of ischemic myocardial blood perfusion and save patients' lives [28]. The myocardium of most patients is effectively perfused, but there are still some patients who cannot obtain normal blood perfusion even after the infarct-related artery is opened, resulting in the no-reflow phenomenon [29]. In patients without reflow, epicardial blood flow returns to normal, but peripheral tissue level perfusion is seriously insufficient, and the myocardial associated with the infarct site does not receive effective blood perfusion [30]. The survival rate of patients with AMI was determined by the opening time of infarct-related arteries and the recovery of myocardial and microcirculation blood flow in infarct-related areas [31]. For patients with AMI, opening a blood vessel as early as possible will benefit the patient the most. Therefore, whether myocardial perfusion is effective in AMI patients after PCI is the primary problem for the success of PCI.
As per the TIMI risk score, AMI patients were cataloged into the group without reflow and group with normal blood reflow. Current study provided miR-542-3p was a low expression in the no-reflow group, representing that miR-542-3p might be correlated with the reflow situation of AMI patients suffering PCI management. Many subjects on abnormal expression and predictive impacts of miRNAs for PCI have been published. The expression of miR-17–92 is correlated with Tai Chi intervention in coronary heart disease patients after PCI [32]. MiR-186-5p expression shows an increase in AMI patients after admission, while it declined after PCI management [33]. The declined miR-30e expression is of the prediction value of reflow [34]. We attempted to explore the value of biochemical parameters and miR-542-3p on the station of reflow after PCI. The logistic analysis stated that miR-542-3p was an independent predictive tool for AMI patients without reflow after PCI.
As previous evidence reported, miR-542-3p is at low expression in the cardiomyocyte hypoxia/reoxygenation model [14, 35]. In addition, a recent study pointed out that miR-542-3p is involved in the protective mechanism of isoflurane pretreatment on myocardial ischemia–reperfusion injury [36], which was in accordance with our present findings in clinical AMI samples. It is believed that the present results can fill the gap in the clinical value of serum miR-542-3p in AMI patients in the clinic. However, the timeline changes of miR-542-3p in AMI cases were not included in the current study, which can help to reflect the correlation between miR-542-3p and disease states. In future, other groups of AMI patients should be included, and a timeline of the changes that occur to miRNA should be recorded to better understand its correlation with disease states.
To sum up, miR-542-3p was decreased in AMI patients and is an indicative marker for AMI. The expression of miR-542-3p declined in group of no-reflow after PCI. The detection of miR-542-3p has a significant clinical effect in screening no-reflow after PCI in AMI.
Data availability
The datasets used and/or analyzed during the current study are available from the corresponding author on reasonable request.
References
Damluji, A. A., Van Diepen, S., Katz, J. N., Menon, V., Tamis-Holland, J. E., Bakitas, M., Cohen, M. G., Balsam, L. B., & Chikwe, J. (2021). Mechanical complications of acute myocardial infarction: A scientific statement from the American Heart Association. Circulation, 144(2), e16–e35.
Johnson, K. W., Glicksberg, B. S., Shameer, K., Vengrenyuk, Y., Krittanawong, C., Russak, A. J., Sharma, S. K., Narula, J. N., Dudley, J. T., & Kini, A. S. (2019). A transcriptomic model to predict increase in fibrous cap thickness in response to high-dose statin treatment: Validation by serial intracoronary OCT imaging. EBioMedicine, 44, 41–9.
Wang, H., & Song, S. (2017). Comparison of right and left trans-radial catheterization for coronary angiography and intervention in patients with Acute myocardial infarction. Pakistan Journal of Medical Sciences, 33(3), 743–746.
Kim, S. H., Cho, J. H., Lee, Y. H., Lee, J. H., Kim, S. S., Kim, M. Y., Lee, M. G., Kang, W. Y., Lee, K. S., Ahn, Y. K., Jeong, M. H., & Kim, S. H. (2018). Improvement in Left ventricular function with intracoronary mesenchymal stem cell therapy in a patient with anterior wall ST-Segment elevation myocardial infarction. Cardiovascular Drugs and Therapy, 32(4), 329–38.
Lee, J. H., Eom, S. Y., Kim, U., Lee, C. H., Son, J. W., Jeon, D. W., Bae, J. H., Oh, S. K., Cha, K. S., Suh, Y., Koh, Y. Y., Yang, T. H., Shim, Dk., Bae, J. W., & Park, J. S. (2020). Effect of operator volume on in-hospital outcomes following primary percutaneous coronary intervention for st-elevation myocardial infarction: Based on the 2014 Cohort of Korean Percutaneous Coronary Intervention (K-PCI) Registry. Korean Circulation Journal, 50(2), 133–44.
Zhang, L., Qi, X., & Jia, X. (2018). Effect of different methods of administration of diltiazem on clinical efficacy in patients with acute ST-segment elevation myocardial infarction. Medical Science Monitor: International Medical Journal of Experimental and Clinical Research, 24, 6544–6550.
Yang, L., Cong, H., Lu, Y., Chen, X., & Liu, Y. (2020). Prediction of no-reflow phenomenon in patients treated with primary percutaneous coronary intervention for ST-segment elevation myocardial infarction. Medicine, 99(26), e20152.
Fajar, J. K., Heriansyah, T., & Rohman, M. S. (2018). The predictors of no reflow phenomenon after percutaneous coronary intervention in patients with ST elevation myocardial infarction: A meta-analysis. Indian Heart Journal, 70, S406-s18.
Xue, J., Jia, E., Ren, N., Lindsay, A., & Yu, H. (2019). Circulating microRNAs as promising diagnostic biomarkers for pancreatic cancer: A systematic review. OncoTargets and Therapy, 12, 6665–6684.
Chen, Z., Pan, X., Yan, G., Sheng, Z., & Ma, G. (2020). MmiR-142 is a sensitive biomarker for the diagnosis and prognosis of acute myocardial infarction. Clinical Laboratory. https://doi.org/10.7754/Clin.Lab.2019.191019
Xue, S., Liu, D., Zhu, W., Su, Z., Zhang, L., Zhou, C., & Li, P. (2019). Circulating MiR-17-5p, MiR-126-5p and MiR-145-3p are novel biomarkers for diagnosis of acute myocardial infarction. Frontiers in Physiology. https://doi.org/10.3389/fphys.2019.00123
Wang, Y. U., Chang, W., Zhang, Y., Zhang, L., Ding, H., Qi, H., Xue, S., Yu, H., Hu, L., Liu, D., Wang, Y., Zhu, W., & Li, P. (2019). Circulating miR-22-5p and miR-122-5p are promising novel biomarkers for diagnosis of acute myocardial infarction. Journal of Cellular Physiology, 234(4), 4778–86.
Wang, K. J., Zhao, X., Liu, Y. Z., Zeng, Q. T., Mao, X. B., Li, S. N., Zhang, M., Jiang, C., Zhou, Y., Qian, C., Feng, K. G., Guan, H. Q., Tang, T. T., Cheng, X., & Chen, Z. J. (2016). Circulating MiR-19b-3p, MiR-134-5p and MiR-186-5p are promising novel biomarkers for early diagnosis of acute myocardial infarction. Cellular Physiology and Biochemistry : International Journal of Experimental Cellular Physiology, Biochemistry, and Pharmacology, 38(3), 1015–29.
Lu, Y., Wu, H., Deng, M., Huang, M., Pan, H., & Yang, P. (2022). miR-542-3p-targeted PDE4D regulates cAMP/PKA signaling pathway and improves cardiomyocyte injury. Contrast Media & Molecular Imaging, 2022, 7021200.
Yan, D., Zhao, L. L., Yue, B. W., Qian, H., Zhang, Z. H., Wang, N., Yan, S. H., & Qian, Y. L. (2019). Granule of BU-XIN RUAN-MAI attenuates the patients’ angina pectoris of coronary heart disease via regulating miR-542-3p/GABARAP signaling. Evidence-Based Complementary and Alternative Medicine : eCAM., 2019, 1808419.
Cao, X., Wu, J., Gu, Y., Liu, X., Deng, Y., & Ma, C. (2021). Post-traumatic stress disorder and risk factors in patients with acute myocardial infarction after emergency percutaneous coronary intervention: A longitudinal study. Frontiers in Psychology., 12, 694974.
Asaria, P., Elliott, P., Douglass, M., Obermeyer, Z., Soljak, M., Majeed, A., & Ezzati, M. (2017). Acute myocardial infarction hospital admissions and deaths in England: a national follow-back and follow-forward record-linkage study. The Lancet Public health, 2(4), e191–e201.
Wang, Q., Ma, J., Jiang, Z., Wu, F., Ping, J., & Ming, L. (2017). Identification of microRNAs as diagnostic biomarkers for acute myocardial infarction in Asian populations: A systematic review and meta-analysis. Medicine, 96(24), e7173.
Zhang, F., & Qiao, S. (2022). Research progress on the relationship between inflammation and colorectal cancer. Annals of Gastroenterological Surgery, 6(2), 204–211.
Li, Y., Li, Z., Liu, J., Liu, Y., & Miao, G. (2021). miR-190-5p alleviates myocardial ischemia-reperfusion injury by targeting PHLPP1. Disease Markers, 2021, 8709298.
Shi, J., Bei, Y., Kong, X., Liu, X., Lei, Z., Xu, T., Wang, H., Xuan, Q., Chen, P., Xu, J., Che, L., Liu, H., Zhong, J., Sluijter, J. P. G., Li, X., Rosenzweig, A., & Xiao, J. (2017). miR-17-3p contributes to exercise-induced cardiac growth and protects against myocardial ischemia-reperfusion injury. Theranostics, 7(3), 664–76.
Zhao, W., Wu, Y., Ye, F., Huang, S., Chen, H., Zhou, R., & Jiang, W. (2021). Tetrandrine ameliorates myocardial ischemia reperfusion injury through miR-202-5p/TRPV2. BioMed Research International, 2021, 8870674.
Wang, K., Long, B. O., Liu, F., Wang, J. X., Liu, C. Y., Zhao, B., Zhou, L. Y., Sun, T., Wang, M., Yu, T., & Gong, Y. (2016). A circular RNA protects the heart from pathological hypertrophy and heart failure by targeting miR-223. European Heart Journal, 37(33), 2602–11.
Li, H., Zhang, P., Li, F., Yuan, G., Wang, X., Zhang, A., & Li, F. (2019). Plasma miR-22-5p, miR-132-5p, and miR-150-3p are associated with acute myocardial infarction. BioMed Research International, 2019, 5012648.
Shao, X., Zhang, X., Yang, L., Zhang, R., Zhu, R., & Feng, R. (2021). Integrated analysis of mRNA and microRNA expression profiles reveals differential transcriptome signature in ischaemic and dilated cardiomyopathy induced heart failure. Epigenetics, 16(8), 917–932.
Xue, S., Zhu, W., Liu, D., Su, Z., Zhang, L., Chang, Q., & Li, P. (2019). Circulating miR-26a-1, miR-146a and miR-199a-1 are potential candidate biomarkers for acute myocardial infarction. Molecular Medicine, 25(1), 18.
Mansouri, F., & Seyed Mohammadzad, M. H. (2020). Molecular miR-19a in acute myocardial infarction: Novel potential indicators of prognosis and early diagnosis. Asian Pacific Journal of Cancer Prevention : APJCP., 21(4), 975–982.
Suga, T., Suga, Y., Oyama, K., Yoshida, M., & Hatori, T. (2020). Complete revascularization of simultaneous acute occlusion of three major coronary arteries. The Journal of Invasive Cardiology., 32(10), E267.
Yang, L., Cong, H., Lu, Y., Chen, X., & Liu, Y. (2021). A nomogram for predicting the risk of no-reflow after primary percutaneous coronary intervention in elderly patients with ST-segment elevation myocardial infarction. Annals of Translational Medicine, 9(2), 126.
Zalewski, J., Claus, P., Bogaert, J., Driessche, N. V., Driesen, R. B., Galan, D. T., Sipido, K. R., Buszman, P., Milewski, K., & Van de Werf, F. (2015). Cyclosporine A reduces microvascular obstruction and preserves left ventricular function deterioration following myocardial ischemia and reperfusion. Basic Research in Cardiology, 110(2), 18.
Hu, Y. C., Yao, W. J., Jin, D. X., Zhang, J. X., Wang, L., Zhang, R., Xu, J. H., & Cong, H. L. (2021). Bivalirudin in patients undergoing percutaneous coronary intervention and independent predictors of postoperative adverse events in these patients: A real world retrospective study. Medicine, 100(10), e25003.
Liu, J., Yu, P., Lv, W., & Wang, X. (2020). The 24-Form Tai Chi improves anxiety and depression and upregulates miR-17-92 in coronary heart disease patients after percutaneous coronary intervention. Frontiers in Physiology, 11, 149.
Li, Z., Wu, J., Wei, W., Cai, X., Yan, J., Song, J., Wang, C., & Wang, J. (2019). Association of serum miR-186-5p with the prognosis of acute coronary syndrome patients after percutaneous coronary intervention. Frontiers in Physiology. https://doi.org/10.3389/fphys.2019.00686
Hu, C. K., Cai, R. P., He, L., He, S. R., Liao, J. Y., & Su, Q. (2022). A Nomogram model for predicting the occurrence of no-reflow phenomenon after percutaneous coronary intervention using the lncRNA TUG1/miR-30e/NPPB biomarkers. Journal of Thoracic Disease, 14(6), 2158–2168.
Sun, S., & Mei, X. (2024). Effect of CASC15 on apoptosis and oxidative stress of cardiomyocytes after hypoxia/reperfusion injury. Revista Portuguesa de Cardiologia, 43(2), 77–84.
Wang, X., Wang, Y., Yuan, Y., Wang, L., & Zhang, D. (2024). Isoflurane pretreatment protects against myocardial ischemia/reperfusion injury via mediating lncRNA CASC15/miR-542-3p axis. Toxicology Mechanisms and Methods, 34(6), 694–702.
Funding
No funding was received for conducting this study.
Author information
Authors and Affiliations
Contributions
S.K. L and X.S. Z designed the research study. Y. C, S.K. L, X.S. Z and C.P. Z performed the research and analyzed the data. Y. C, S.K. L and C.P. Z wrote the manuscript. All authors contributed to editorial changes in the manuscript. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Conflict of interest
The authors report no conflicts of interest.
Ethical Approval
The study protocol was approved by The Ethics Committee of The Affiliated Hospital of Xuzhou Medical University and followed the principles outlined in the Declaration of Helsinki. In addition, informed consent has been obtained from the participants involved.
Consent for Publication
Not applicable.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Chen, Y., Liu, S., Zhang, X. et al. Changes and Diagnostic Significance of miR-542-3p Expression in Patients with Myocardial Infarction. Mol Biotechnol (2024). https://doi.org/10.1007/s12033-024-01272-w
Received:
Accepted:
Published:
DOI: https://doi.org/10.1007/s12033-024-01272-w