Abstract
Renal cancer is the most lethal urological cancer and characterized by high metastasis rate at initial diagnosis and drug resistance to current chemotherapeutics. Betulinic acid is a pentacyclic triterpene with broad biological activity that occurs naturally in variety of plants. Even though the anti-cancer efficacy of betulinic acid have been reported by many studies, the information about the pathways and the molecules which are affected by betulinic acid in renal cancer are limited. Epithelial–mesenchymal transition (EMT) is considered as the initial step of metastasis and contributes to drug resistance of cancer cells. Depending on the role of EMT in cancer progression and drug resistance, targeting EMT may represent an effective strategy in this context. Therefore, we aimed to investigate the anti-metastatic effects of betulinic acid on renal cell carcinoma cells by evaluating two EMT markers, SNAIL-1, and SDC-2. Following the treatment of betulinic acid at determined doses by WST-1 cytotoxicity assay in our previous study, SDC-2 expression level was decreased in both cell lines. Additionally, in correlation with this result, we also found a reduction in SDC-2 and SNAIL-1 protein levels which are measured by ELISA. Furthermore, the migration and invasion capacities were suppressed by betulinic acid treatment in metastatic renal adenocarcinoma ACHN cells. Taken together, our findings indicate that betulinic acid may constitute a potential treatment approach for renal cancer with further investigations.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Renal cancer is the most lethal urological cancers and accounts for approximately 2% of all adult malignant tumors [1]. According to GLOBOCAN research, 431,288 new cases of renal cancer were diagnosed and 179,368 patients died of renal cancer in 2020 [2]. Renal cancer is a heterogeneous type of cancer with different genetic and molecular alterations and also has many histological subtypes such as clear cell renal cell carcinoma (ccRCC), papillary renal cell carcinoma (pRCC) and chromophobe renal cell carcinoma (crRCC) [3].Therefore, since renal cancer cannot be considered as a single type of cancer, patient management and determination of appropriate treatment options are critical [4]. Treatment options for renal cancer are determined by location, size, stage, histological type, and genomic profile of the tumor [5]. Renal cancers which are diagnosed at early stage and localized are treated with nephrectomy and ablative therapies [6]. On the other hand, about 30% of patients have advanced and metastatic disease at initial diagnosis since renal cancer does not show any specific clinical symptoms. While the 5 year survival rate of the patients who are at early stage is 80–90%, the rate is significantly reduced to 10–12% for patients with advanced or metastatic disease [7]. Approved targeted drugs such as sunitinib, sorafenib, axitinib, bevacizumab and cabozantinib are used in the treatment of advanced or metastatic patients [8]. However, a substantial majority of patients who are receiving approved therapies develop resistance to these therapeutics and eventually experience tumor progression [9]. Due to the high metastasis rate at initial diagnosis and challenges in treatment of renal cancer, there is a need to develop efficient potential anti-cancer drugs to reduce mortality and improve the 5-year survival rate.
Natural compounds derived from plants have become potential therapeutics for human disease due to their low toxicity and potent efficacy. The fact remains that this compounds exhibit anti-cancer activity with reducing the side effects of current therapeutics and improving survival rate and quality of life [10]. One of these natural compounds, betulinic acid (3β‐hydroxy‐lup‐20(29) ‐en‐28‐oicacid) is a member of triterpenoids and its chemical structure consists of pentacyclic isoprene units. It is mainly obtained from the bark of Betula sp. and Betulaceae, and the barks, leaves and roots of various plants such as Platanus acerifolia, Pterospermum heterophyllum and Tetracera potatoria are also sources of betulinic acid [11]. Betulinic acid has been shown to have anti-inflammatory [12], anti-obesity [13] and anti-oxidant [14] effects in recent studies along with its strong anti-cancer effects. It is known that betulinic acid has an anti-proliferative effect against cancer cells without causing toxicity in healthy cells [15]. Moreover, it has been determined that betulinic acid suppresses tumorigenesis through apoptotic, autophagic [16] and metastatic [17] pathways in various cancer types. Metastasis, which is the main cause of cancer lethality, is a process, in which the cancer cells leave their primary site and enter the bloodstream to locate in distant organs. This process is managed by a series of mechanisms that regulate the alteration of genomic profiles, cell phenotypes, and microenvironment interactions [18]. The transformation of cancer cells with epithelial phenotype in the primary site into motile cells, by increasing mesenchymal characteristic features is called epithelial–mesenchymal transition (EMT) [19]. During the EMT, cells lose their cell-to-cell junctions, apical-basal polarity, and adherence to basement membrane, acquiring the anterior–posterior polarity and cell-extracellular matrix dissociation. This transformation is orchestrated by transcription factors such as SNAIL, zing-finger E-box-binding (ZEB) and TWIST, which suppress epithelial markers genes E-cadherin, Occludins and Claudins, and stimulate mesenchymal marker genes N-cadherin, Vimentin, and matrix metalloproteinases (MMPs) [20]. The expressions of these markers are majorly controlled by one of the SNAIL proteins; SNAIL-1, which binds to E-box DNA sequences through carboxy terminal zing-finger domains of the genes [21]. On the other hand, Syndecan-2 (SDC-2) is a cell surface heparan sulfate proteoglycan, which has also been determined to have a role in differentiation of tumor cells during EMT and induce invasive phenotype in various studies, apart from its role in tissue and organ differentiation and embryonic angiogenesis [22, 23]. Although there are many studies in the literature on the expression of SDC-2 in different cancer types, the relationship between SDC-2 and renal cancer has not yet been demonstrated.
With respect to this, we aimed the investigation of the effect of betulinic acid on EMT pathway, by measuring SNAIL-1 and SDC-2 levels in renal cell carcinoma cells. Our results showed that betulinic acid dramatically reduced SDC-2 gene expression and SNAIL-1 and SDC-2 protein levels and suppressed migration and invasion in renal cancer cells.
Materials and methods
Reagents and assay kits
Betulinic acid was purchased form Sigma-Aldrich (St Louis, MO, USA). The stock solution was prepared by diluting with DMSO (dimethyl sulfoxide) (Glentham Life Sciences, Corsham, United Kingdom) (Lot: GK2245) to final concentration of 100 µM and stored at −20 °C until being used. Cell lines and all cell culture reagents were purchased from ATCC (American Type Culture Collection, Manassas, USA). WST-1 cell viability assay kit was obtained from Roche Life Science (Mannheim, Germany). RNA isolation (Catalog Number: 12183018A) and cDNA (Lot:0,065,423) synthesis kits were purchased from Thermo fisher Scientific (Massachusetts, USA). SNAIL-1 (Catalog Number: KTE62329) and Syndecan-2 (Catalog Number: KTE60728) ELISA kits were purchased form Abbkine Scientific (California, USA). Migration (Catalog Number: 3465-096-K) and Invasion (Catalog Number: 3467-096-K) assay kits were bought from Trevigen Inc. (Gaithersburg, Maryland, USA).
Cell lines and cell culture
CAKI-2 (clear cell renal cell carcinoma) and ACHN (metastatic renal adenocarcinoma) cells were cultured in McCoy’s 5A medium and EMEM (Eagle’s Minimum Essential Medium), (GIBCO, Green Island, NY, USA) respectively. The cell culture media are supplemented with %1 Penicillin–Streptomycin and %10 Fetal Bovine Serum (FBS) (GIBCO, Green Island, NY, USA). All cell lines were maintained in humidified incubator with 5% CO2 at 37 °C.
Cell viability assay
In our previous study, in which we examined the anti-cancer effect of betulinic acid, we performed the WST-1 cell viability assay to determine the cell viability of cells treated with betulinic acid [24]. Briefly, cells (1 × 104 cells per well) were seeded in 96-well plates and incubated for 24 h. Thereafter, cells were treated with betulinic acid, prepared in increasing concentration (1 µM, 2.5 µM, 5 µM, 7.5 µM, 10 µM, 25 µM, 50 µM) from the stock solution for 24 h, 48 h and 72 h incubation time. At the end of each incubation period, 10 µl WST-1 solution was applied to each well and incubated for 4 h at 37 °C. Color change was measured at 440 nm using microplate ELISA reader (Thermo Fisher Scientific, USA).
Detection of gene expression levels
Total RNA was isolated from cells using total RNA isolation kit after betulinic acid treatment. Total RNA was used to synthesize cDNA via High-Capacity cDNA Reverse Transcription Kit. To detection of RNA expression levels Real-Time Polymerase Chain Reaction (qPCR) was performed using TaqMan Probe. The real-time PCR reaction conditions were as follow: denaturation at 95 °C for 15 s; annealing at 60 °C for 1 m; and elongation at 72 °C for 30 s for 40 cycles. GAPDH was used normalization and the expression levels of SNAIL-1 and SDC-2 genes were calculated as \(\Delta\)CT. Each experiment group was performed in duplicate.
Measurement of protein levels by ELISA
SNAIL-1 and SCD-2 protein levels were measured by Enzyme-Linked Immunosorbent Assay (ELISA). Briefly, after the cells were treated with betulinic acid, cell culture supernatants were diluted with sample dilution buffer. Samples and diluted standards were applied in wells. End of incubation period, wells were washed with wash buffer. HRP-conjugated antibody and chromogen A and B solutions were added, respectively. Finally, stop solution was added in each well and color change from blue to yellow was observed. Plates were measured at 450 nm using microplate ELISA reader.
Migration and invasion assays
For the cell migration and invasion assays, initially cells were starved with serum-free medium for 24 h. Then, betulinic acid treated cells were seeded at 5 × 104 per well into top chamber. Medium containing 10% FBS was added to bottom chamber. The FBS in the medium was used as a chemoattractant for cells. After 24 h of incubation at 37 °C, aspirated top and bottom chamber and washed each well with Wash Buffer. Calcein-AM and Cell Dissociation solution was added to bottom chamber of the black assay plate and incubated at 37 °C for one hour. Removed top chamber, and bottom chamber was read at 485 nm excitation, 520 nm emission using fluorescence reader. (BioTek Instruments, Vermont, USA).
Statistical analysis
Statistical analyzes were performed using the SPSS 21.0 package program. The statistical significance limit was accepted as p < 0.05. Mann–Whitney-U test was used in the evaluation between groups.
Results
Anti-proliferation effect of betulinic acid in renal cell carcinoma cells
In our previous study we conducted in our laboratory on the anti-proliferation effect of betulinic acid on the same renal cell carcinoma cells as described above [24]. According to the results, betulinic acid significantly reduced cell viability in CAKI-2 and ACHN cells and the effective doses of betulinic acid were chosen as 25 µM and 50 µM and the optimal incubation time to 24 h. We observed 46.6% and 84.3% decrease in cell viability for 24 h at 25 µM and 50 µM, respectively. At the same incubation time and concentrations, 53.5% and 70.6% decrease in cell viability of ACHN cells was observed, respectively. On the other hand, we did not observe any significant toxic effect betulinic acid on healthy cells that we used as a control.
Betulinic acid inhibits SDC-2 gene expression level
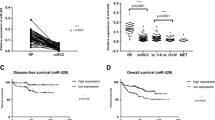
We determined the effect of betulinic acid on the EMT marker SDC-2 and its relationship with renal cancer for the first time in the literature. Accordingly, we observed that SDC-2 expression level was decreased in both renal cell carcinoma cells treated with betulinic acid compared to untreated cell group. As shown in Fig. 1A, SDC-2 gene expression level was markedly suppressed in CAKI-2 cells treated with 25 µM (p = 0.006) and 50 µM (p = 0.001) betulinic acid. Conversely, SNAIL-1 gene expression level was significantly increased in both cell lines (Fig. 1B).
Effect of betulinic acid on SDC-2 and SNAIL-1 gene expression level. Changes in the expression of A SDC-2 and B SNAIL-1 genes after 25 and 50 µM betulinic acid treatment were assessed by Real-Time PCR, and results are represented as \(\Delta\)CT in the graphs. (SDC-2: Syndecan-2, BetA: Betulinic Acid)
Betulinic acid inhibits SNAIL-1 and SDC-2 protein levels
Following the determination of gene expression levels, we also examined the effect of betulinic acid on these protein levels. According to ELISA results, in CAKI-2 cells, compared to untreated cell group, we observed 22.6% and 20.9% decrease in SDC-2 protein level at 25 µM and 50 µM concentrations, respectively (Fig. 2A). These results correlated with SDC-2 gene expression results in CAKI-2 cells. Besides we also detected 1.4% and 10.1% decrease in SDC-2 protein level at 25 µM and 50 µM concentrations in ACHN cells, respectively. On the other hand, SNAIL-1 protein level was decreased in ACHN cells, treated with betulinic acid at 25 µM (29.2%) and 50 µM (14.1%) concentrations (Fig. 2B).
Betulinic acid suppresses migration and invasion of metastatic renal adenocarcinoma cells
We examined the effect of betulinic acid on migration and invasion levels which are known to be key steps in the metastatic process of cancer cells. As presented in Fig. 3A, betulinic acid treatment suppressed migration and invasion in metastatic renal adenocarcinoma ACHN cells depending on increasing concentrations. Accordingly, in ACHN cells treated with betulinic acid at 25 µM concentration, there was a decrease of 28% and 12.9% in migration and invasion rate, respectively. When 50 µM betulinic acid was applied, 46.37% and 15.65% reduction in migration and invasion rate was observed. Contrary to this, we did not observe any significant change in migration and invasion rates in CAKI-2 cells (Fig. 3B).
Effect of betulinic acid on migration and invasion capacities of renal cell carcinoma cells. Migration and invasion rates were measured in A metastatic renal adenocarcinoma ACHN cells and B clear cell renal carcinoma CAKI-2 cells treated with 25 µM and 50 µM betulinic acid, and the results are represented as percentages in the graphs. (BetA: Betulinic Acid)
Discussion
Renal cancer is a lethal and the most prevalent genitourinary cancer type with high mortality and morbidity rates, and its incidence is increasing every year [2]. Treatment of a localized tumor at early diagnosis includes nephrectomy and ablative therapy, while a combination of surgery and targeted systemic therapies are applied in advanced and metastatic renal cancer [8]. Despite the successful progress in these therapies, the high mortality rate of renal cancer patients is explained by the high metastasis rate of the patients at the initial diagnosis and high resistance to chemotherapeutic treatment [7]. Chemotherapeutic treatments, even with strong destructive effects on cancer cells, are still effective to a certain level due to their substantially toxic side effects. Therefore, it has become an urgent need to develop new drug strategies to cope with these challenges in renal cancer treatment. Natural compounds derived from plants are being investigated as potential therapeutics in cancer treatment due to their low toxicity on normal cells, high efficacy against cancer cells and better cost-effectiveness [10].
Betulinic acid is a pentacyclic triterpene which has a wide biological activity as well as its potent anti-cancer effects [12]. Although it is known that betulinic acid constitutively triggers the mitochondrial apoptosis pathway [25] without inducing toxicity to normal cells [26], according to many studies, it has been determined that betulinic acid shows anti-cancer effects in various types of cancers through other different cellular pathways. For instance, Xu et al. demonstrated that betulinic acid induced apoptosis following the ROS generation by downregulated PI3K/Akt signaling pathway in human cervical cancer cells [26]. In other studies, it has been reported that betulinic acid inhibited translocation of NF-kB to the nucleus [27] and suppressed angiogenesis by inhibiting STAT-3 and HIF-1α from binding to the VEGF promoter [28]. Even though there are many findings on the anti-cancer effects of betulinic acid in various cancers, the mechanism of action directly on molecules and other different pathways in renal cancer remains unclear. In the present study, we reported the anti-metastatic efficacy of betulinic acid on renal cell carcinoma cells. The results showed that betulinic acid inhibited invasion, migration, and suppressed epithelial-mesenchymal transition marker, SDC-2.
Epithelial–mesenchymal transition (EMT) is considered as the initial step of metastasis, in which the cancer cells with epithelial origin acquire mesenchymal and invasive phenotype and thus, contribute tumor progression in several cancer types including renal cancer. Krebs et al. reported that ZEB1, an EMT transcription factor, is closely associated with tumor grade, invasion, metastasis and tumor progression in mouse pancreatic cancer model [29]. Studies have shown that higher expressions of Vimentin and TWIST1 and lower expression of E-cadherin are associated with high tumor grade, poor prognosis and worse progression-free survival in renal cancer patients [30, 31]. In addition to triggering metastatic properties, EMT is also known to be associated with drug resistance in cancer cells. Iseri et al. demonstrated the upregulation of Slug, N-cadherin and Vimentin expressions and the downregulation of E-cadherin, Occludins and Claudins expressions in paclitaxel, docetaxel and doxorubicin resistant MCF-7 cells compared to sensitive MCF-7 cells [32]. Moreover, in oxaliplatin resistant hepatocellular carcinoma cells with high migration and invasion capacity, knockdown of SNAIL reversed the EMT process and increased the sensitivity of cells to oxaliplatin [33]. Epithelial–mesenchymal transition seems to play a major role in metastasis and drug resistance processes, the two main causes of cancer-related deaths. Therefore, targeting the reversal of drug resistance induced by EMT using natural compounds in anti-cancer drug studies may be a useful and more inclusive strategy.
In this study, we observed anti-metastatic effects of betulinic acid in CAKI-2 and ACHN cells. We carried out WST-1 assay to determine the anti-proliferative activity of betulinic acid in our previous study, and the results indicated that betulinic acid not only inhibited cell viability of renal cell carcinoma cells but also did not induce any toxic effect on healthy cells. In the light of these results, we evaluated the expression and protein levels of SNAIL-1 and Syndecan-2 (SDC-2) after the betulinic acid treatment. We found that betulinic acid reduced SDC-2 gene expression in both cell lines. Correlating with this result, SDC-2 protein level also decreased in both cell lines. Recent studies have revealed that, overexpression of SDC-2 in colon [23], prostate [34] and gastric cancer [35] are associated with tumor growth, aggressiveness, metastatic and invasive dispositions. Jang et al. determined that overexpression of SDC-2 leads to shedding of E-cadherin via matrix metalloproteinase-7 (MMP-7) activation and may initiate EMT by causing fibroblast-like morphological change of colon cancer cells [36]. On the other hand, it has been reported that betulinic acid impairs the metastatic capability of cancer cells by inhibition of EMT. Studies showed that betulinic acid repressed EMT by decreasing SNAIL, SLUG, Vimentin, and N-cadherin expression and by increasing E-cadherin expression in pancreatic [37], colorectal [19] and bladder cancer [38] cells. With our findings, the inhibitory effect of betulinic acid on SDC-2 and its relationship with renal cancer were determined for the first time in the literature. Furthermore, for the effect of betulinic acid on metastatic behavior of the cells, we also assessed migration and invasion assays. The important result at this point is that betulinic acid remarkably reduced the migration and invasion rates of metastatic renal adenocarcinoma ACHN cells.
To sum up, our findings suggest that betulinic acid have an inhibitory effect on SDC-2 and significantly reduced metastatic potential in renal cell carcinoma cells. Although further studies are needed to elucidate the mechanisms underlying the anti-metastatic potential of betulinic acid on renal cancer, our findings confirm that betulinic acid may be one of the potential treatment strategies for renal cancer.
References
Capitanio U, Bensalah K, Bex A, Boorjian SA, Bray F, Coleman J, Gore JL, Sun M, Wood C, Russo P. Epidemiology of renal cell carcinoma. Eur Urol. 2019;75(1):74–84.
Sung H, Ferlay J, Siegel RL, Laversanne M, Soerjomataram I, Jemal A, Bray F. Global cancer statistics 2020: GLOBOCAN estimates of incidence and mortality worldwide for 36 cancers in 185 countries. CA Cancer J Clin. 2021;71(3):209–49.
Inamura K. Renal cell tumors: understanding their molecular pathological epidemiology and the 2016 WHO classification. Int J Mol Sci. 2017;18(10):2195.
Linehan WM, Ricketts CJ. The cancer genome atlas of renal cell carcinoma: findings and clinical implications. Nat Rev Urol. 2019;16(9):539–52.
Bhatt JR, Finelli A. Landmarks in the diagnosis and treatment of renal cell carcinoma. Nat Rev Urol. 2014;11(9):517–25.
Jonasch E, Gao J, Rathmell WK. Renal cell carcinoma. BMJ. 2014;349: g4797.
Zeng Q, Zhang W, Li X, Lai J, Li Z. Bioinformatic identification of renal cell carcinoma microenvironment-associated biomarkers with therapeutic and prognostic value. Life Sci. 2020;243: 117273.
Pontes O, Oliveira-Pinto S, Baltazar F, Costa M. Renal cell carcinoma therapy: current and new drug candidates. Drug Discov Today. 2022;27(1):304–14.
Dutta S, Mahalanobish S, Saha S, Ghosh S, Sil PC. Natural products: An upcoming therapeutic approach to cancer. Food Chem Toxicol. 2019;128:240–55.
Lou H, Li H, Zhang S, Lu H, Chen Q. A review on preparation of betulinic acid and its biological activities. Molecules. 2021;26(18):5583.
Zhang X, Hu J, Chen Y. Betulinic acid and the pharmacological effects of tumor suppression (Review). Mol Med Rep. 2016;14(5):4489–95.
Kun-Liu, Wang JY, Zhang L, Pan YY, Chen XY, Yuan Y.(2020) Effects of betulinic acid on synovial inflammation in rats with collagen-induced arthritis. Int J Immunopathol Pharmacol.;34:2058738420945078.
Kim KD, Jung HY, Ryu HG, Kim B, Jeon J, Yoo HY, Park CH, Choi BH, Hyun CK, Kim KT, et al. Betulinic acid inhibits high-fat diet-induced obesity and improves energy balance by activating AMPK. Nutr Metab Cardiovasc Dis. 2019;29(4):409–20.
Musayeva A, Unkrig JC, Zhutdieva MB, Manicam C, Ruan Y, Laspas P, Chronopoulos P, Göbel ML, Pfeiffer N, Brochhausen C, et al. Betulinic Acid Protects from ischemia-reperfusion injury in the mouse retina. Cells. 2021;10(9):2440.
Pisha E, Chai H, Lee IS, Chagwedera TE, Farnsworth NR, Cordell GA, Beecher CW, Fong HH, Kinghorn AD, Brown DM, et al. Discovery of betulinic acid as a selective inhibitor of human melanoma that functions by induction of apoptosis. Nat Med. 1995;1(10):1046–51.
Zhang Y, He N, Zhou X, Wang F, Cai H, Huang SH, Chen X, Hu Z, Jin X. Betulinic acid induces autophagy-dependent apoptosis via Bmi-1/ROS/AMPK-mTOR-ULK1 axis in human bladder cancer cells. Aging (Albany NY). 2021;13(17):21251–67.
Zeng A, Hua H, Liu L, Zhao J. Betulinic acid induces apoptosis and inhibits metastasis of human colorectal cancer cells in vitro and in vivo. Bioorg Med Chem. 2019;27(12):2546–52.
Fares J, Fares MY, Khachfe HH, Salhab HA, Fares Y. Molecular principles of metastasis: a hallmark of cancer revisited. Signal Transduct Target Ther. 2020;5(1):28.
Lamouille S, Xu J, Derynck R. Molecular mechanisms of epithelial-mesenchymal transition. Nat Rev Mol Cell Biol. 2014;15(3):178–96. https://doi.org/10.1038/nrm3758.
Dongre A, Weinberg RA. New insights into the mechanisms of epithelial-mesenchymal transition and implications for cancer. Nat Rev Mol Cell Biol. 2019;20(2):69–84.
Peinado H, Olmeda D, Cano A. Snail, Zeb and bHLH factors in tumour progression: an alliance against the epithelial phenotype? Nat Rev Cancer. 2007;7(6):415–28.
Hua R, Yu J, Yan X, Ni Q, Zhi X, Li X, Jiang B, Zhu J. Syndecan-2 in colorectal cancer plays oncogenic role via epithelial-mesenchymal transition and MAPK pathway. Biomed Pharmacother. 2020;121: 109630.
Mytilinaiou M, Nikitovic D, Berdiaki A, Kostouras A, Papoutsidakis A, Tsatsakis AM, Tzanakakis GN. Emerging roles of syndecan 2 in epithelial and mesenchymal cancer progression. IUBMB Life. 2017;69(11):824–33.
Ergen A, Iplik ES, Ertugrul B, Atas MN, Kasarci G, Cakmakoglu B. Examination of the apoptotic effects of betulinic acid on renal cancer cell lines. Marmara Medical Journal. 2021;33(3):113–8.
Fulda S, Scaffidi C, Susin SA, Krammer PH, Kroemer G, Peter ME, Debatin KM. Activation of mitochondria and release of mitochondrial apoptogenic factors by betulinic acid. J Biol Chem. 1998;273(51):33942–8.
Xu T, Pang Q, Wang Y, Yan X. Betulinic acid induces apoptosis by regulating PI3K/Akt signaling and mitochondrial pathways in human cervical cancer cells. Int J Mol Med. 2017;40(6):1669–78.
Shankar E, Zhang A, Franco D, Gupta S. Betulinic acid-mediated apoptosis in human prostate cancer cells involves p53 and nuclear factor-kappa B (NF-κB) pathways. Molecules. 2017;22(2):264.
Shin J, Lee HJ, Jung DB, Jung JH, Lee HJ, Lee EO, Lee SG, Shim BS, Choi SH, Ko SG, et al. Suppression of STAT3 and HIF-1 alpha mediates anti-angiogenic activity of betulinic acid in hypoxic PC-3 prostate cancer cells. PLoS ONE. 2011;6(6): e21492.
Krebs AM, Mitschke J, Lasierra Losada M, Schmalhofer O, Boerries M, Busch H, Boettcher M, Mougiakakos D, Reichardt W, Bronsert P, et al. The EMT-activator Zeb1 is a key factor for cell plasticity and promotes metastasis in pancreatic cancer. Nat Cell Biol. 2017;19(5):518–29.
Rasti A, Madjd Z, Abolhasani M, Mehrazma M, Janani L, Saeednejad Zanjani L, Asgari M. Cytoplasmic expression of Twist1, an EMT-related transcription factor, is associated with higher grades renal cell carcinomas and worse progression-free survival in clear cell renal cell carcinoma. Clin Exp Med. 2018;18(2):177–90.
Xu H, Xu WH, Ren F, Wang J, Wang HK, Cao DL, Shi GH, Qu YY, Zhang HL, Ye DW. Prognostic value of epithelial-mesenchymal transition markers in clear cell renal cell carcinoma. Aging (Albany NY). 2020;12(1):866–83.
Işeri OD, Kars MD, Arpaci F, Atalay C, Pak I, Gündüz U. Drug resistant MCF-7 cells exhibit epithelial-mesenchymal transition gene expression pattern. Biomed Pharmacother. 2011;65(1):40–5.
Ma JL, Zeng S, Zhang Y, Deng GL, Shen H. Epithelial-mesenchymal transition plays a critical role in drug resistance of hepatocellular carcinoma cells to oxaliplatin. Tumour Biol. 2016;37(5):6177–84.
Popović A, Demirović A, Spajić B, Stimac G, Kruslin B, Tomas D. Expression and prognostic role of syndecan-2 in prostate cancer. Prostate Cancer Prostatic Dis. 2010;13(1):78–82.
Wang J, Lu C, Chen J, Chen X, Wang S, Lu X, Tang X. Expression of Syndecan-2 in gastric adenocarcinoma and its effect on tumorigenesis in vitro. Transl Cancer Res. 2017. https://doi.org/10.21037/tcr.2017.08.04.
Jang B, Jung H, Chung H, Moon BI, Oh ES. Syndecan-2 enhances E-cadherin shedding and fibroblast-like morphological changes by inducing MMP-7 expression in colon cancer cells. Biochem Biophys Res Commun. 2016;477(1):47–53.
Sun L, Cao J, Chen K, Cheng L, Zhou C, Yan B, Qian W, Li J, Duan W, Ma J, et al. Betulinic acid inhibits stemness and EMT of pancreatic cancer cells via activation of AMPK signaling. Int J Oncol. 2019;54(1):98–110.
Kim SY, Hwangbo H, Kim MY, Ji SY, Kim DH, Lee H, Kim GY, Moon SK, Leem SH, Yun SJ, et al. Betulinic acid restricts human bladder cancer cell proliferation in vitro by inducing caspase-dependent cell death and cell cycle arrest, and decreasing metastatic potential. Molecules. 2021;26(5):1381.
Funding
This work was funded by Scientific Research Projects Coordination Unit of Istanbul University. Project No. TSA-2019–35150.
Author information
Authors and Affiliations
Contributions
MNA; Laboratory Analysis and Writing, BE; Laboratory Analysis, ESİ; Statistical Analysis, BÇ; Data Extraction, AE; Study Design and Writing.
Corresponding author
Ethics declarations
Conflict of interest
The authors have no conflicts of interest to declare.
Ethical approval
This article does not contain any studies with human participants or animals performed by any of the authors.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Ataş, M.N., Ertuğrul, B., İplik, E.S. et al. The inhibitory effect of betulinic acid on epithelial–mesenchymal transition pathway in renal cell carcinoma. Med Oncol 39, 170 (2022). https://doi.org/10.1007/s12032-022-01775-z
Received:
Accepted:
Published:
DOI: https://doi.org/10.1007/s12032-022-01775-z