Abstract
The optimal treatment for hepatocellular carcinoma (HCC) is surgical resection. However, only a small percentage of patients are amenable to this option. Percutaneous radiofrequency interstitial thermal ablation (TA) proved to be effective in the treatment of unresectable HCC. Recent advances in laparoscopic ultrasound have improved the accuracy in detecting small intrahepatic HCC nodules missed by pre-operative imaging techniques. Our objective was to evaluate an operative combination of laparoscopic ultrasound with laparoscopic thermoablation (LTA) in the treatment of HCC not amenable to liver resection. The aim of our review was to evaluate the advantages and limits of the laparoscopic approach according the criteria of the evidence-based medicine. LTA of HCC proved to be a safe and effective technique both in the short- and long-term follow-up period. This technique may be indicated in selected cases when the percutaneous approach to the lesion is very difficult or contraindicated.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
In recent years, radiofrequency interstitial thermal ablation (TA) has been performed with good results in patients with hepatocellular carcinoma (HCC). Furthermore, while TA is most commonly performed through a percutaneous approach [1, 2], there is a sub-group of patients who may benefit from a laparoscopic thermoablation (LTA) approach [3]. The rationale of this technique is to combine the advantages of an improved staging allowed by the intracorporeal ultrasound examination [4] with a safe approach to liver lesions difficult or impossible to be treated percutaneously [3]. The aim of our review was to evaluate the advantages and limits of the laparoscopic approach according the criteria of the evidence-based medicine (www.cebm.net). A systematic research of PubMed, Science Citation Index, and Embase databases was accomplished for articles published before October 2019. We identified 29 articles using the keywords “laparoscopic radiofrequency and hepatocellular carcinoma” and “laparoscopic microwave and hepatocellular carcinoma” to obtain all studies useful for this review analysis. Manual cross-referencing was accomplished, and we also analyzed the reference lists of the included articles to identify further undetected studies. Case reports and abstracts were excluded. Table 1 shows the characteristics of these 29 studies [4,5,6,7,8,9,10,11,12,13,14,15,16,17,18,19,20,21,22,23,24,25,26,27,28,29,30,31,32].
Basing on its peculiar characteristics, the LTA should be able:
To stage the intrahepatic HCC disease at best using laparoscopic ultrasound (LUS) [33];
To treat patients at risk of unsuccessful therapy through a percutaneous access;
To treat safely those patients at risk of complications;
To improve the thermoablation results (total necrosis and tumor recurrence).
Staging of the intrahepatic disease
Although intraoperative ultrasound (IOUS) is the most effective tool for detecting focal liver lesions [34], this technique has shown remarkable amount of false positive for what concern HCC definition in cirrhotic patients [35]. The introduction of second-generation US contrast agents, has improved the accuracy of IOUS in this specific field [36]. This technique via laparoscopic approach so-called laparoscopic ultrasound (LUS) uses a linear array high-resolution (7.5 MHz) transducers mounted on probes that are introduced through standard 11.0 mm trocars. Even if few papers have been reported, LUS shown a great value in HCC diagnosis and staging (Table 2); better staging, by detecting new suspect HCC in 8–22% of cases [6, 7, 10, 12, 17, 26], means to avoid unnecessary laparotomy with a remarkable percentage of patients (16.5%) as reported by Lai et al. who shown 44 out of 122 consecutive patients with HCC and liver cirrhosis found to be unresectable after laparoscopic staging [37]. Authors concluded that LUS have a significant effect both on identifying surgically untreatable disease and in selecting the optimal treatment strategy. The key point is to be sure of histology of new suspect HCC found by LUS.
Moreover, Ido et al. [38] reported power of LUS in detecting new suspect HCC nodules in 64 out of 186 patients (34.4%); LUS guided biopsy was made on all 134 new lesions with a histological confirm in 28 cases (21%). Nevertheless, this quite low yield of LUS in detecting true HCCs, the authors outlined that when new nodular lesions are detected by LUS, these patients must be considered at high risk for recurrence, even if there is no histological evidence of HCC. We reported similar results in our personal series with 22% out of 68 patients submitted to LUS showing new malignant nodules. These findings support the validity of a single-stage approach with discovery and immediate treatment of new HCC nodules allowed by the LUS use [26].
Moreover, Klegar et al. [39] remarked high yield of LUS in changing operative management in 9/20 (45%) of HCC scheduled for liver resection. Management was changed because of LUS finding of severe nodular cirrhosis in four cases, more extensive staging in six cases either for number of nodules or for intrahepatic satellites metastases or carcinomatosis discover. On the contrary LUS shown a down staging in two cases, thus allowing a gentler procedure.
Among opponents of considering LUS as a crucial staging tool in HCC surgical treatment, Reddy et al. [40] reported his experience on 16 patients scheduled for liver transplantation (LT), all submitted to LUS as first step, thus showing to be suitable to LT in 100% of cases. Finally, at laparotomy, one patient was found to have extrahepatic disease; thus, the procedure was abandoned. One patient was found to have lesser curvature lymphadenopathy. Two patients had major vascular involvement noted in the explanted liver. Finally, authors concluded that laparoscopy cannot be routinely performed as a staging tool in a pre-transplant program due to low yield.
Any way on the basis of these data, there is a reasonable evidence that laparoscopic staging is useful and may alter patient management and treatment in patients with HCC and liver cirrhosis (level 2b of evidence).
Outcomes
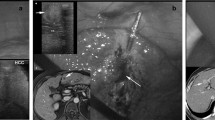
Fulfilling criteria for thermoablation laparoscopic approach are shown in Table 3, including patients not suitable to HR, or patients with HCC not visible to percutaneous route (liver dome) or deep next to hilum (high risk of biliary stricture), or superficial lesions juxta visceral structures (gallbladder, colon, or stomach) as regards laparoscopic approach is effective and safe, allowing the direct visualization of surrounding structures and their active protection by performing specific laparoscopic maneuvers (separating or cooling techniques) thus reducing the risk of visceral injuries [26].
Table 4 shows the outcomes in the published series. However, until 2013, the articles included few patients and the results reflect a pioneering period for the LTA. The ability to identify and treat lesions located at the dome of the liver, peripheral in the liver, or in proximity to other organs makes LTA more flexible than the percutaneous approach, while remaining minimally invasive [22, 26, 32]. However, if the percutaneous procedure is unfeasible, this can be considered a problematic situation also for the laparoscopic approach, influencing the LTA results. In the last years, as regards LTA efficacy, technical success (total necrosis) could be obtained in a single session in more than 90% of all patients and it is in the expected range (90–100%) with similar results obtained by the most important percutaneous series [1, 2, 41, 42]. On the other hand, local tumor progression (LTP) in an TA ablated site is a serious occurrence, with described rates ranging from 3.2 to 26% after RFA in percutaneous series [1, 41, 42], influenced by the tumor size and the difficult location of the nodules. Also for the laparoscopic approach, different indications (see Table 3) should influence the LTP results: in articles published in the last years, the LTP rates in the laparoscopic series ranged from 2.8 to 23%. Many of these studies have suggested that local control of the laparoscope is an advantage during LTA compared with the percutaneous approach. LTP rates shown in the LTA studies represent very good results considering the problematic locations of the HCC tumors submitted to a laparoscopic approach. Some Authors showed that subcapsular tumors and/or tumors contiguous to viscera had an independent statistical association with LTP after percutaneous ablation [22, 43, 44]. In subcapsular tumors, saline injection into the abdominal cavity could be an effective method to widen the extrahepatic space before the RFA procedure reducing the risk of visceral complications [45]. Also, in the study of De La Serna et al. [22], LTP rates are higher for HCC superficially located. However, in other studies the laparoscopic approach obtain higher rates of success for superficial lesions [26, 32], we ascribe the improved LTP rates to the fact that both LUS and direct visualization can become more precise in targeting the lesion, while the increased technical difficulty of placing percutaneously the electrode adequately for a subcapsular tumor, thus leading to incomplete ablation. Also, for lesions contiguous to viscera, they can safely be mobilized away from the target lesion decreasing the risk of LTP and complications after LTA. On the other hand, also for the laparoscopic approach, the presence of LTP after treatment of deep-sited lesions remains a real problem: larger studies should confirm that this approach could improve LTP and technique effectiveness for deep-sited nodules.
It’s mandatory to develop new laparoscopic ultrasound probes or navigation technologies able to simplify electrode insertion into the lesion, thus getting the procedure safer, more effective and reliable, and overcoming the limit of puncturing deep-sited tumors with a totally free-hand technique. Finally, LTA seems to obtain a good rate of total necrosis also in patients with lesions difficult to treat for their position (level 4 of evidence); further studies are needed to elucidate if LTA is able to obtain better results than the percutaneous approach in unselected patients.
Safe treatment of patients at risk of complications
The laparoscopic procedure proved to be feasible and safe with a low rate of serious complications [46,47,48]. In the majority of these series, severe complications rates (Dindo-Clavien classes superior to 3A and 3B) were 2% or less.
Most common complications after LTA are pulmonary affections (pneumonia and pneumothorax) due to the needle route through the wall chest, and postoperative bleeding from the abdominal wall (trocar access). The advantage of laparoscopic approach over the percutaneous via is the proper bleeding control if early recognize during operation. Moreover, there is so-called “post-ablative syndrome”, an early and transient postoperative (within 24–48 h) treatment-related side-effect, including abdominal pain, mild fever, and pleural effusion, generally not requiring any invasive treatment. Quite exceptional complications are bile duct stenosis, liver infarction, and liver abscess or failure. A very few cases of tumor seeding in the puncture route and intraperitoneal dissemination have been described.
Finally, the rate of complications is similar among both approaches (laparoscopic and percutaneous), with a mild advantage for the former especially for what concern bleeding and visceral damage control. (level 4 of evidence).
Conclusion
Laparoscopic thermoablation is an effective and safe curative treatment for HCCs not suitable to liver resection, when percutaneous approach is not feasible (level 4 of evidence).
Abbreviations
- HCC:
-
Hepatocellular carcinoma
- LTA:
-
Laparoscopic thermoablation
- LTP:
-
Local tumor progression
- TA:
-
Thermoablation
- HR:
-
Hepatic resection
- IOUS:
-
Intraoperative ultrasound
- INR:
-
International Normalized Ratio
- TACE:
-
Transcatheter arterial chemoembolization
- LUS:
-
Laparoscopic ultrasound
- CT:
-
Computed tomography
- MRI:
-
Magnetic resonance imaging
References
Lencioni R, Cioni D, Bartolozzi C. Percutaneous radiofrequency thermal ablation of liver malignancies: techniques, indications, imaging findings, and clinical results. Abdom Imaging. 2001;26:345–60.
Livraghi T, Meloni F, Di Stasi M, Rolle E, Solbiati L, Tinelli C, Rossi S. Sustained complete response and complications rates after radiofrequency ablation of very early hepatocellular carcinoma in cirrhosis: is resection still the treatment of choice? Hepatology. 2008;47:82–9.
Santambrogio R, Bianchi P, Pasta A, Palmisano A, Montorsi M. Ultrasound-guided interventional procedures of the liver during laparoscopy technical considerations. Surg Endosc. 2002;16:349–54.
Ido K, Isoda N, Kawamoto C, Hozumu M, Suzuki T, Nagamine N, Nakazawa Y, Ono K, Hirota N, Hyodoh H, Kimura K. Laparoscopic microwave coagulation therapy for solitary hepatocellular carcinoma performed under laparoscopic ultrasonography. Gastrointest Endosc. 1997;45:415–20.
Ito T, Niiyama G, Kawanaka M, et al. Laparoscopic microwave coagulation for the treatment of hepatocellular carcinoma. Dig Endosc. 1999;11:137–43.
Goletti O, Lencioni R, Armillotta N, Puglisi A, Lippolis PV, Lorenzetti L, Cioni D, Musco B, Bartolozzi C, Cavina E. Laparoscopic radiofrequency thermal ablation of hepatocarcinoma: preliminary experience. Surg Laparosc Endosc Percutan Tech. 2000;10:284–90.
Podnos YD, Henry G, Ortiz JA, Ji P, Cooke J, Cao S, Imagawa DK. Laparoscopic ultrasound with radiofrequency ablation in cirrhotic patients with hepatocellular carcinoma: technique and technical considerations. Am Surg. 2001;67:1181–4.
Hsieh CB, Chang HM, Chen TW, et al. Comparison of transcatheter arterial chemoembolization, laparoscopic radiofrequency, and conservative treatment for decompensated cirrhotic patients with hepatocellular carcinoma. World J Gastroenterol. 2004;10:505–8.
Ballem N, Berber E, Pitt T, Siperstein A. Laparoscopic radiofrequency ablation of unresectable hepatocellular carcinoma: long-term follow-up. HPB. 2008;10:315–20.
Casaccia M, Adorno E, Nardi I, et al. Laparoscopic US-guided radiofrequency ablation of unresectable hepatocellular carcinoma in liver cirrhosis: feasibility and clinical outcome. J Laparoendosc Adv Surg Tech. 2008;18:797–801.
Hirooka M, Kisaka Y, Uehara T, et al. Efficacy of laparoscopic radiofrequency ablation for hepatocellular carcinoma compared to percutaneous radiofrequency ablation with artificial ascites. Dig Endosc. 2009;21:82–6.
Panaro F, Piardi T, Audet M, et al. Laparoscopic ultrasound-guided radiofrequency ablation as a bridge to liver transplantation for hepatocellular carcinoma: preliminary results. Transplant Proc. 2010;42(4):1179–81.
Tesche LJ, Newton KN, Unger J, Semelka RC, Gerber DA. Efficacy and tolerability of laparoscopic-assisted radiofrequency ablation of hepatocellular carcinoma in patients above 60 years of age. Surg Laparosc Endosc Percutan Tech. 2010;20:404–9.
Simo KA, Sereika SE, Newton KN, Gerber DA. Laparoscopic-assisted microwave ablation for hepatocellular carcinoma: safety and efficacy in comparison with radiofrequency ablation. J Surg Oncol. 2011;104:822–9.
Yoon YS, Han HS, Cho JY, Yoon CJ, Kim JH. Laparoscopic approach for treatment of multiple hepatocellular Carcinomas. Surg Endosc. 2012;26(11):3133–40.
Seleem MI, Gerges SS, Elkhouly A, El-wakeel B, Hassany M. Laparoscopic radiofrequency thermal ablation of hepatocellular carcinoma in liver cirrhosis patients. Gastroenterol Res. 2012;5:232–5.
Herbold T, Wahba R, Bangard C, et al. The laparoscopic approach for radiofrequency ablation of hepatocellular carcinoma-indication, technique and results. Langenbecks Arch Surg. 2013;398:47–53.
Swan RZ, Sindram D, Martinie JB, Iannitti DA. Operative microwave ablation for hepatocellular carcinoma: complications, recurrence, and long-term outcomes. J Gastrointest Surg. 2013;17:719–29.
Iida H, Aihara T, Ikuta S, Yamanaka N. A comparative study of therapeutic effect between laparoscopic microwave coagulation and laparoscopic radiofrequency ablation. Hepatogastroenterology. 2013;60:22–5.
Jiang K, Zhang W, Su M, et al. Laparoscopic radiofrequency ablation of solitary small hepatocellular carcinoma in the caudate lobe. EJSO. 2013;39:1236–42.
Jiang K, Su M, Zhao X, et al. ‘‘One-off’’ complete radiofrequency ablation of hepatocellular carcinoma adjacent to the gallbladder by a novel laparoscopic technique without gallbladder isolation. Cell Biochem Biophys. 2014;69:605–17.
De la Serna S, Vilana R, SanchezCabus S, Calatayud D, Ferre J, Molina V, Fondevila C, Bruix J, Fuster J, Garcia Valdecasas JC. Results of laparoscopic radiofrequency ablation for HCC Could the location of the tumour influence a complete response to treatment? A single European Centre Experience. HPB. 2015;17:387–93.
Murakami K, Naka S, Shiomi H, et al. Initial experiences with MR Image-guided laparoscopic microwave coagulation therapy for hepatic tumors. Surg Today. 2015;45:1173–8.
Tang Z, Zhu Y, Tang K, et al. Laparoscopic combined with percutaneous ablation for hepatocellular carcinoma under liver capsule: a single Chinese center experience of thirty patients. J Cancer Res Ther. 2016;12:143–7.
Baker EH, Thompson K, McKillop IH, et al. Operative microwave ablation for hepatocellular carcinoma: a single center retrospective review of 219 patients. J Gastrointest Oncol. 2017;8:337–46.
Santambrogio R, Barabino M, Bruno S, Costa M, Pisani Ceretti A, Angiolini MR, Zuin M, Meloni F, Opocher E. Long-term outcome of laparoscopic ablation therapies for unresectable hepatocellular carcinoma: a single European center experience of 426 patients. Surg Endosc. 2016;30:2103–13.
Gruttadauria S, Pagano D, Tropea A, Cintorino D, Castellana L, Bonsignore P, Ricotta C, Vizzini G, Luca A. Laparoscopic approach for thermoablation microwave in the treatment of hepatocellular carcinoma: a single center experience. J Laparosc Adv Surg Tech. 2016;26(10):808–11.
Na BG, Kim JM, Oh DK, et al. Clinical outcomes of laparoscopic radiofrequency ablation of single primary or recurrent hepatocellular carcinoma (≤3 cm). Ann Surg Treat Res. 2017;92:355–60.
Ding H, Su M, Zhu C, Wang L, Zheng Q, Wan Y. CT-guided versus laparoscopic radiofrequency ablation in recurrent small hepatocellular carcinoma against the diaphragmatic dome. Sci Rep. 2017;7:44583.
Eun HS, Lee BS, Kwon IS, et al. Advantages of laparoscopic radiofrequency ablation over percutaneous radiofrequency ablation in hepatocellular carcinoma. Dig Dis Sci. 2017;62:2586–600.
Wang T, Zhang XY, Lu X, Zhai B. Laparoscopic microwave ablation of hepatocellular carcinoma at liver surface: technique effectiveness and long-term outcomes. Technol Cancer Res Treat. 2019;18:1–9.
Cillo U, Bertacco A, Fasolo E, et al. Videolaparoscopic microwave ablation in patients with HCC at a European high-volume center: results of 815 procedures. J Surg Oncol. 2019;120:956–65.
Lo CM, Lai ECS, Liu CL, Fan ST, Wong J. Laparoscopy and laparoscopic ultrasonography avoid exploratory laparotomy in patients with hepatocellular carcinoma. Ann Surg. 1998;227:527–32.
Kokudo N, Bandai Y, Imanishi H, et al. Management of new hepatic nodules detected by intraoperative ultrasonography during hepatic resection for hepatocellular carcinoma. Surgery. 1996;119:634–40.
Takigawa Y, Sugawara Y, Yamamoto J, Shimada K, Yamasaki S, Kosuge T, Makuuchi M. New lesions detected by introperative ultrasound during liver resection for hepatocellular carcinoma. Ultrasound Med Biol. 2001;27:151–6.
Torzilli G, Olivari N, Moroni E, et al. Contrast-enhanced intraoperative ultrasonography in surgery for hepatocellular carcinoma in cirrhosis. Liver Transpl. 2004;10:S34–S3838.
Lai ECH, Tang CN, Ha JPY, Tsui DKK, Li MKW. The evolving influence of laparoscopy and laparoscopic ultrasonography on patients with hepatocellular carcinoma. Am J Surg. 2008;196:736–40.
Ido K, Nakazawa Y, Isoda N, et al. The role of laparoscopic US and laparoscopic US-guided aspiration biopsy in the diagnosis of multicentric hepatocellular carcinoma. Gastrointest Endosc. 1999;50:523–6.
Klegar EK, Marcus SG, Newman E, Hiotis SP. Diagnostic laparoscopy in the evaluation of the viral hepatitis patient with potentially resectable hepatocellular carcinoma. HPB. 2005;7:204–7.
Reddy MS, Smith L, Jaques BC, et al. Do laparoscopy and intraoperative ultrasound have a role in the assessment of patients with end-stage liver disease and hepatocellular carcinoma for liver transplantation? Transpl Proc. 2007;39:1474–6.
Brunello F, Cantamessa A, Gaia S, Carucci P, Rolle E, Castiglione A, Ciccone G, Rizzetto M. Radiofrequency ablation: technical and clinical long-term outcomes for single hepatocellular carcinoma up to 30 mm. Eur J Gastroenterol Hepatol. 2013;25:842–9.
Lee DH, Lee JM, Lee JY, Kim SH, Yoon JH, Kim YJ, Han JK, Choi BI. Radiofrequency ablation of hepatocellular carcinoma as first-line treatment: long-term results and prognostic factors in 162 patients with cirrhosis. Radiology. 2014;270:900–9.
Chinnaratha MA, Chuang MA, Fraser RJ, Woodman RJ, Wigg AJ. Percutaneous thermal ablation for primary hepatocellular carcinoma: a systematic review and meta-analysis. J Gastroenterol Hepatol. 2016;45:1230–5.
Poulou LS, Botsa E, Thanou I, Ziakas PD, Thanos L. Percutaneous microwave ablation vs radiofrequency ablation in the treatment of hepatocellular carcinoma. World J Hepatol. 2015;7:1054–63.
Kim JW, Shin SS, Heo SH, Hong JH, Lim HS, Seon HJ, Hur YH, Park CH, Jeong YY, Kang HK. Ultrasound-guided percutaneous radiofrequency ablation of liver tumors: how we do it safely and completely. Korean J Radiol. 2015;16:1226–399.
Montorsi M, Santambrogio R, Bianchi P, Dapri G, Spinelli A, Podda M. Perspectives and drawbacks of minimally invasive surgery for hepatocellular carcinoma. Hepatogastroenterology. 2002;49:56–61.
Mulier S, Mulier P, Ni Y, et al. Complications of radiofrequency coagulation of liver tumors. Br J Surg. 2002;89:1206–22.
Gillams AR. Radiofrequency ablation in the management of liver tumors. EJSO. 2003;29:9–16.
Montorsi M, Santambrogio R, Bianchi P, et al. Laparoscopy with laparoscopic ultrasound (L-LUS) for the pre-treatment staging of hepatocellular carcinoma: a prospective study. Gastrointestinal Surg. 2001;5:312–5.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Santambrogio, R., Barabino, M., D’Alessandro, V. et al. Laparoscopic thermoablation for hepatocellular carcinoma in patients with liver cirrhosis: an effective procedure for tricky tumors. Med Oncol 37, 32 (2020). https://doi.org/10.1007/s12032-020-1342-5
Received:
Accepted:
Published:
DOI: https://doi.org/10.1007/s12032-020-1342-5