Abstract
RENAL score has been validated on predicting adverse events and relapses in percutaneous treatments of renal lesions. To better fit interventional issues a modified score (mRENAL) has been introduced, but the only difference from the RENAL score is on the dimensional parameter. However, it remains of surgical derivation while a specific interventional score is missing. This study aims to obtain a specific score (ABLATE) to better quantify the risk of complications and relapses in percutaneous kidney ablation procedures compared to the existing surgical scores. Taking inspiration from previous papers, a score was built to quantify the real difficulties faced in percutaneous treatment of renal lesions. The ABLATE score was used on 71 cryoablations to evaluate its predictivity of complications and relapses. Logistic regression was used to predict complication incidence; Cox-regression was used for relapses; ROC analysis was used to evaluate the accuracy of the different scores. Between January 2014 and November 2019, 71 lesions in 68 patients were treated. Overall, malignant histology was found in 62 lesions (87.3%). Mean and median RENAL, mRENAL, and ABLATE scores were 7.04 and 7, 7.19 and 7, and 5.11 and 4, respectively. Out of 71 treatments, we experienced 3 bleeding with anemia (4.2%), only 2 of which needed further treatment (2.82%). The mean and median RENAL, mRENAL, and ABLATE scores in those with complications were 7.66 and 7.01 (p = 0.69), 8.0 and 7.1 (p = 0.54), and 6.6 and 5.0 (p = 0.38), respectively. Out of 62 malignant lesions, we experienced 2 persistent and 6 recurrent lesions (3.2% and 8.4%, respectively). At Cox-regression analyses, mABLATE score outperformed both RENAL and mRENAL scores in predicting recurrences (HR 1.48; p < 0.001 vs. 1.41; p = 0.1 vs. 1.38: p = 0.07, respectively). The ABLATE score showed to be a better predictor of relapses than RENAL and mRENAL. The small number of complications conditioned a lack of statistic power on complications for all the scores. At the moment to quantify the risks in percutaneous kidney ablation procedures, surgical scores are used. A specific score better performs this task.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Local ablative therapies have become an established treatment option in interventional oncology. Percutaneous thermal ablation of renal masses is a minimally invasive procedure that has proven to be an effective and safe treatment for selected patients [1, 2].
The American Urological Association consensus guidelines include percutaneous ablation as an acceptable treatment option in selected patients since 2013 and this concept was reiterated in the 2017 version, even if only for cT1a renal masses < 3 cm [3]. However, T1b tumors are also included in numerous studies.
Although nephrectomy remains the reference standard for renal tumor treatment, physician acceptance and patient interest in percutaneous ablation are growing as intermediate- and long-term outcome data become available; for example, Whitson et al. [4] compared 7704 nephron-sparing surgeries and 1114 renal ablations using data from the surveillance, epidemiology, and end results cancer registry and showed very similar 5-year disease-specific survival rates (98.3% vs 96.6%).
In the last years, improved ablation devices have widened the range of renal lesions that can be successfully and safely treated.
Over the years, several scores attempted to predict relapses and complications in renal lesion treatments.
The RENAL nephrometry score, developed for surgical resection, is a standardized method to assess the complexity of renal masses 5. In some studies, this score predicts treatment success [5, 6] and complications [5,6,−7] for percutaneous treatments. But there are other studies disagreeing these results: one in particular reported diameter > 3 cm (and not RENAL) predicts treatment failure [8], whereas other studies have not identified any factors predictive of treatment success [9]. As a result, a modified RENAL (mRENAL) nephrometry score was proposed to predict relapses for radiofrequency ablations [10]. Hence, mRENAL is also a surgical-born score and was validated to better predict complications than RENAL score only 2 years later [11].
Taking inspiration from a study that describes a planning algorithm for renal ablation [12], we tried to build a specific interventional score to predict the complication and recurrence rate in percutaneous treatment of renal lesions.
Materials and methods
Between January 2014 and November 2018, all consecutive patients submitted to renal cryoablation for renal mass were included in our prospective database. For each procedure, Galil Medical (© 2018 Galil Medical Inc, 4364 Round Lake Road Arden Hills, MN 55112 USA) cryoprobes and cryostat were used. A total of 115 icerods, 25 icespheres, and 3 iceseeds were used with a mean of 2.01 cryoprobes for each procedure. The number and the type of probes used for each treatment were decided in the preprocedural evaluation according to size, shape, and characteristics of the lesion to be treated. This evaluation aimed to achieve the best cryoball to cover the lesion, minimizing the involvement of healthy structures, as each type of probe provides cryoballs of different shape and size.
Using the same acronym, we added some modifications to the ABLATE algorithm [12] creating the ABLATE score, structured as follows (summary in Fig. 1):
A (axial tumor diameter)
Literature shows how small lesions are easier to be treated with a lower risk of complication and recurrence [13,14,15,16,−17].
1 point was assigned for each centimeter of maximum diameter, starting from 0.
B (bowel proximity)
Close proximity of the renal mass to the bowel increases the complexity of the ablation procedure and increases the complication rate for the chance to cause a thermal damage to the bowel [18, 19].
Maneuvers to minimize the risk of bowel injury include simple changes in patient position and/or injection of either gas (pneumodisplacement) [20] or fluid hydrodisplacement) [21, 22] between the tumor and bowel for mechanical displacement.
Points for this parameter were assigned as follows:
0 if the lesion is farther than 15 mm from the bowel,
1 if it is between 5 and 15 mm, and
3 if bowel and lesion are closer than 5 mm.
L (location within the kidney)
Historically only tumors located on the posterior and lateral aspect of the kidney, far from the bowel and other critical structures, were considered amenable for percutaneous ablation.
With growing experience, renal masses in more challenging locations started to be treated with this technique.
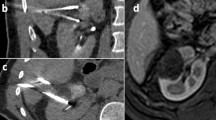
In case of anterior masses, we assigned 3 points, but only 1 point if the anterior mass did not have anteriorly interposed bowel loops (Fig. 2).
2 points in case of medial masses.
1.5 points if the mass was located in the upper pole.
1 point if the mass was located in the right kidney and a transhepatic approach was feasible, because despite appearances this is a relatively easy and safe approach.
0 points for every other location within the kidney.
A (angle)
This parameter is innovative compared to the ABLATE algorithm paper12 because it introduces an exclusive concept for the TC-guided percutaneous renal treatment.
Every single angle different from the axial path increases the difficulty of the procedure.
0 points in case of pure axial path.
0.5 points in case of an antero-posterior angle > 10°.
1 point in case of a cranio-caudal angle > 10°.
2 points in case of both antero-posterior and cranio-caudal angles > 10°.
0.5 points for each probe with a different approach: this means no extra points in case of 2 or more needles if all of them have parallel paths.
T (touching)
This parameter has similar title but wider meaning than that of the ABLATE algorithm paper [12] as in our score we assigned points for each structure than could be touched by the lesion, except for the bowel, already described.
3 points if the lesion was closer than 5 mm from ureter or renal pelvis.
2 points if the lesion touches the renal sinus fat because this increases the local recurrence rate more than the percentage of endophytic or exophytic lesion, as described in a recent work [23]. This is easily explained with the so-called heat sink effect [13]. These points are not added to those of ureter or renal pelvis contact because it is assumed that if a lesion affects the renal pelvis or the ureter it also touches renal sinus fat.
1.5 points if the lesion was closer than 5 mm from the collecting system, the adrenal glands or the diaphragm, because of the risk of complications in these cases.
1 point if the lesions touched the abdominal wall or the spleen for the need of hydrodissection.
E (extra)
Unlike the ABLATE algorithm paper [12], we didn’t consider whether a lesion was endophytic or exophytic because this condition was indirectly considered in previous points.
We left this last point for extra conditions.
2 points in case the mass was a relapse lesion, because this condition is a single predictor for complication and relapse rate increase.
We gave 1 extra point if a lesion was surrounded by cysts because this increases the complication and the relapse rate. The first for the incremented chance of bleeding, the latter for the heat (or cold) sink effect.
Statistical analyses
We tested the ABLATE score on our population for prediction of both complications occurrence and prediction of relapse during follow-up. The accuracy of the new score was compared to the RENAL and the mRENAL scores.
First, mean values of the 3 scores were compared between patients who experienced complications and those who did not using the t test. Second, univariable logistic regression analyses were performed in order to predict post-operative complications according to the 3 scores.
Third, mean values of the 3 scores were compared between patients who experienced disease relapse and those who did not using the t test.
Finally, Cox-regression analyses were performed in order to predict disease recurrence according to the 3 scores.
Results
Between January 2014 and November 2018, 71 lesions in 68 patients were treated. Table 1 shows pre-operative patients’ characteristics. Mean age was 69.6 years among which 47 and 21 were males and females, respectively. Mean and median maximum lesion diameters were 22.1 and 22 mm, respectively. Most lesions were primary (87.3%) while only 9 (12.7%) were secondary. Nearly all lesions were subjected to percutaneous biopsy simultaneously to the ablative procedure; the lesions that weren’t subjected to biopsy were the relapsed ones that already had a histological characterization from the previous surgery/ablation. The majority of the lesions were found to harbor clear cell carcinoma (n = 46; 64.7%). Overall, a malignant histology was found in 62 lesions (87.3%). In one case, the biopsy was inconclusive. Mean and median RENAL, mRENAL, and ABLATE scores were 7.04 and 7, 7.19 and 7, and 5.11 and 4, respectively.
We experienced a total of three periprocedural complications (3/71 = 4.2%) but only 2 of them needed further treatment (2/71: 2.82%): 1 renal bleeding treated conservatively (no blood infusion nor embolization), 1 intrarenal pseudoaneurysm successfully treated by a transarterial embolization, and 1 bleeding in the site of embolization treated with blood infusion and transarterial embolization. The mean RENAL, mRENAL, and ABLATE scores in those with complications were 7.66 and 7.01 (p = 0.69), 8.0 and 7.1 (p = 0.54), and 6.6 and 5.0 (p = 0.38), respectively. Moreover, univariable logistic regression analyses did not show any association between the three scores and the presence of post-operative complications, probably related to the low number of events considered.
Mean and median follow-up after treatment were 22.3 and 24.5 months, respectively.
Recurrence analyses were performed only on lesions with malignant histology. In 2 lesions of the malignant group (2/62 = 3.2%) the first post-operative MRI performed within the first 6 months after treatment showed persistence of disease. During follow-up, 6 (6/62 = 8.4%) additional lesions showed radiological signs of recurrence. We chose, for statistical reasons, to combine the persistence of the disease with disease recurrence.
Therefore, the total number of relapses during follow-up was 8 (12.9%), and 1- and 3-year recurrence-free survival rates were 85 and 77%, respectively.
Figure 3 shows the ability of the three evaluated scores to discriminate between lesions with and without recurrence at follow-up. Mean ABLATE score for recurrent tumors was 8.13 vs. 4.73 for non-recurrent lesions (p < 0.0001).
Finally, at Cox-regression analyses, ABLATE score outperformed both RENAL and mRENAL scores in predicting recurrences (HR 1.48; p < 0.001 vs. 1.41; p = 0.1 vs. 1.38: p = 0.07, respectively).
Discussion
Surgical or surgical modified scores are currently used to quantify risks in percutaneous kidney ablations.
In our clinical practice in kidney ablation, we found that these scores are unreliable in describing the real difficulties; sometimes, we found a lesion with a small score difficult to be approached with percutaneous ablative techniques, and sometimes, a lesion with a high score proves to be easily approached with these techniques.
This is why we strongly believe, and demonstrated, that a specific interventional score performs this task much better than a surgical one.
Using surgical scores, lesions are assigned the same score regardless of the treatment technique. Our score tests the procedure, not the lesion, and provides different values according to the therapeutic strategy, varying according to the number of needles or their angle. This is potentially very important because the interventional radiologist can plan different strategies for each lesion and choose the one with the lowest score and, consequently, the one that provides the least risk of relapses or complications.
One study limitation was the exclusive use of cryoablation in our institution. Further analyses should be carried out to assess m ABLATE scoring system for other ablative techniques.
Furthermore, another limitation was the small number of complications obtained in our population, which didn’t allow the statistical strength for the score to be considered effective in predicting complications. Hence, a larger population should be analyzed to address this topic.
Notwithstanding the limitations aforementioned, in our preliminary experience, ABLATE has proven to be a reliable scoring system in predicting relapses.
Therefore, we believe the ABLATE score has the potential to be used as a strong base, which is capable of being improved relying on evidences from the scientific world.
References
Yin X, Cui L, Li F, Qi S, Yin Z, Gao J. Radiofrequency ablation versus partial nephrectomy in treating small renal tumors: a systematic review and meta-analysis. Medicine. 2015;94(50):e2255.
Olweny EO, Park SK, Tan YK, Best SL, Trimmer C, Cadeddu JA. Radiofrequency ablation versus partial nephrectomy in patients with solitary clinical T1a renal cell carcinoma: comparable oncologic outcomes at a minimum of 5 years of follow-up. Eur Urol. 2012;61(6):1156–61.
Campbell S, Uzzo RG, Allaf ME, Bass EB, Cadeddu JA, Chang A, Clark PE, Pierorazio PM, Davis BJ, Derweesh IH, Giambarresi L, Gervais DA, Hu SL, Lane BR, Leibovich BC. Guidelines Committee of the American Urological Association. Renal Mass and Localized Renal Cancer: AUA Guidelines.
Whitson JM, Harris CR, Meng MV. Population-based comparative effectiveness of nephron-sparing surgery vs ablation for small renal masses. BJU Int. 2012;110:1438–43.
Kutikov A, Uzzo RG. The RENAL nephrometry score: a comprehensive standardized system for quantitating renal tumor size, location and depth. J Urol. 2009;182(3):844–53.
Mouli SK, McDevitt JL, Su Y-K, Ragin AB, Gao Y, Nemcek AA Jr, Lewandowski RJ, Salem R, Sato KT. Analysis of the RENAL and mRENAL scores and the relative importance of their components in the prediction of complications and local progression after percutaneous renal cryoablation. JVIR. 2017;28(6):860–7.
Sisul DM, Liss MA, Palazzi KL, Briles K, Mehrazin R, Gold RE, Masterson JH, Mirheydar HS, Jabaji R, Stroup SP, L'Esperance JO, Wake RW, Rivera-Sanfeliz G, Derweesh IH. RENAL nephrometry score is associated with complications after renal cryoalbation: a multicenter analysis. Urology. 2013;81:775–80.
Kim EH, Tanagho YS, Bhayani SB, Saad NE, Benway BM, Figenshau RS. Percutaneous cryoablation of renal masses: Washington University experience of treating 129 tumours. BJU Int. 2013;111(6):872–9.
Vricella GJ, Haaga JR, Adler BL, Nakamoto D, Cherullo EE, Flick S, Ponsky LE. Percutaneous cryoablation of renal masses: impact of patient selection and treatment parameterson outcomes. Urology. 2011;77:649–54.
Gahan JC, Richter MD, Seideman CA, Trimmer C, Chan D, Weaver M, Olweny EO, Cadeddu JA. The performance of a modified RENAL nephrometry score in predicting renal mass radiofrequency ablation success. Urology. 2015;85:125–9.
Mouli SK, McDevitt JL, Su YK, Ragin AB, Gao Y, Nemcek AA Jr, Lewandowski RJ, Salem R, Sato KT. Analysis of the RENAL and mRENAL scores and the relative importance of their components in the prediction of complications and local progression after percutaneous renal cryoablation. J Vasc Interv Radiol. 2017;28:860–7.
Schmit GD, Kurup AN, Weisbrod AJ, Thompson RH, Boorjian SA, Wass CT, Callstrom MR, Atwell TD. ABLATE: a renal ablation planning algorithm. AJR Am J Roentgenol. 2014;202:894–903.
Gervais DA, McGovern FJ, Arellano RS, McDougal WS, Mueller PR. Radiofrequency ablation of renal cell carcinoma: part 1, Indications, results, and role in patient management over a 6-year period and ablation of 100 tumors. AJR. 2005;185:64–71.
Varkarakis IM, Allaf ME, Inagaki T, et al. Percutaneous radio frequency ablation of renal masses: results at a 2-year mean followup. J Urol. 2005;174:456–60.
Zagoria RJ, Traver MA, Werle DM, Perini M, Hayasaka S, Clark PE. Oncologic efficacy of CT-guided percutaneous radiofrequency ablation of renal cell carcinomas. AJR. 2007;189:429–36.
Best SL, Park SK, Youssef RF, et al. Long-term outcomes of renal tumor radio frequency ablation stratified by tumor diameter: size matters. J Urol. 2012;187:1183–9.
Ferakis N, Bouropoulos C, Granitsas T, Mylona S, Poulias I. Long-term results after computed tomography-guided percutaneous radiofrequency ablation for small renal tumors. J Endourol. 2010;24:1909–13.
Atwell TD, Carter RE, Schmit GD, et al. Complications following 573 percutaneous renal radiofrequency and cryoablation procedures. J Vasc Interv Radiol. 2012;23:48–544.
Silverman SG, Tuncali K, vanSonnenberg E, et al. Renal tumors: MR imaging-guided percutaneous cryotherapy—initial experience in 23 patients. Radiology. 2005;236:716–24.
Allaf ME, Lang E. Bowel separation before percutaneous renal cryoablation. J Urol. 2008;180:721.
Bodily KD, Atwell TD, Mandrekar JN, et al. Hydro-displacement in the percutaneous cryoablation of 50 renal tumors. AJR. 2010;194:779–83.
Farrell MA, Charboneau JW, Callstrom MR, Reading CC, Engen DE, Blute ML. Paranephric water instillation: a technique to prevent bowel injury during percutaneous renal radiofrequency ablation. AJR. 2003;181:1315–7.
Eiken PW, Atwell TD, Kurup AN, Boorjian SA, Thompson RH, Schmit GD. Imaging following renal ablation: what can we learn from recurrent tumors? Abdom Radiol (NY). 2018;43:2750–5.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflicts of interest.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Papa, M., Suardi, N., Losa, A. et al. ABLATE: a score to predict complications and recurrence rate in percutaneous treatments of renal lesions. Med Oncol 37, 26 (2020). https://doi.org/10.1007/s12032-020-01351-3
Received:
Accepted:
Published:
DOI: https://doi.org/10.1007/s12032-020-01351-3