Abstract
To evaluate safety, efficacy of drug-eluting beads with irinotecan (DEBIRI) on local response and survival of patients affected by colorectal liver metastases (CRLM) progressing during or after second line was evaluated. Sixty-two patients, with colorectal liver metastases, not suitable for surgery or thermal ablation treatments, progressing during or within 6 month from the end of second-line chemotherapy, were treated with DEBIRI chemoembolization between February 2009 and July 2014. CRLM were histologically confirmed. Exclusion criteria were considered. The DEBIRI technique consists in intrahepatic embolization of metastases with non-absorbable beads (75–150 μm and 100–300 μm) preloaded with irinotecan, carried near tumour using a selective catheterization of the right or of the left hepatic artery. To control pain associated with treatment, we use a specific schedule. Efficacy of treatment, defined as lack of disease progression and reduction in size of metastasis according to RECIST 1.1 criteria, was evaluated after two treatments with contrast-enhanced computed tomography (CT) at 4 months. If necessary, more treatments are repeated. A total of 191 procedures were performed. No intra-/peri-procedural death occurred. Pain and post-embolization syndrome were generally controlled by medications. Overall, the efficacy of treatment, evaluated in terms of stability and remission of the disease, was 37.1%. In our experience, DEBIRI technique results as a safe and effective procedure, with good intra- and peri-procedural tolerability.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Transcatheter and percutaneous treatments for primary liver tumours are well established, but liver is also a prime site of metastases, particularly from colorectal cancer (CRC). At the time of first diagnosis of CRC, 20–50% of patients already present synchronous colorectal liver metastases (CRLM) and another 60% will develop liver metastases during or after treatment [1, 2].
Although resection is the only potentially curative treatment for colorectal cancer liver metastases (CRLM), offering 5-year survival rates of 30–50% and long-term cure rates of 20%, only about 15% of patients with liver metastases will be suitable for complete resection at the time of diagnosis [3, 4].
Currently, the standard first-line treatment of CRLM is a combination of infusional 5-FU, folinic acid with either irinotecan (FOLFIRI) or oxaliplatin (FOLFOX) with a response rate of 50%.
In second-line therapy, the response rate is much lower with a response rate of 6% to FOLFIRI and 21% with FOLFOX [5, 6].
Without treatment, the median survival of patients with colorectal liver metastases is 6–12 months; in inoperable liver metastases, not responding to systemic chemotherapy, the reported median survival ranged between 12 and 21 months [7]; hepatic insufficiency is often the principal cause of death.
On the other hand, in CRLM patients with liver-dominant disease hepatic locoregional intra-arterial chemoembolization might be an alternative treatment option.
In recent years, new techniques were developed to support chemotherapy, which in this setting, used alone, fails to control the progression of CRLM; particularly, the use of drug-eluting beads (DEBs), which can be loaded with irinotecan (DEBIRI), allows drug release after the DEBs are trapped in the tumoural circulation, and was first reported for the treatment of CRLM in 2006 [8].
There is an increasing body of data from clinical trials that confirmed DEBIRI as safe, reliable, in patients with unresectable colorectal liver metastases in progression with systemic chemotherapy, controlling disease and resultant hepatic insufficiency [9,10,11,12,13,14,15,16,17,18].
In particular, the approach resulted in a significantly better response rate and progression-free survival, highlighting the benefit of local–regional intra-arterial infusion treatment [12, 13].
Our study enrolled colorectal cancer patients with main location of the disease in the liver, not suitable for surgery or thermo-ablation treatments in order to evaluate the feasibility, safety, tolerance and efficacy of DEBIRI in the treatment of CRLM refractory to chemotherapy in patients with liver-dominant disease.
One of the main problems of the treatment DEBIRI that sometimes precluded subsequent procedures because of patient’s refusal is the intra- and post-procedural pain; therefore, it has also been referred to patients a visual analogue scales (VASs) for assessing the tolerance of treatment.
Materials and methods
Study design and patient population
This retrospective study included 62 patients (39 males and 23 females; 61.7 median age) with unresectable liver metastases from colorectal adenocarcinoma (27/62: unilobar disease; 35/62: bilobar disease), not suitable for surgery or thermo-ablation treatments, in progression during or after second-line chemotherapy with usual conventional protocol of FOLFOX and FOLFIRI in combination with biological agents bevacizumab or cetuximab according to the kras/nras/braf status, submitted to liver chemoembolization with DEBIRI technique.
All patients were required to have histologically confirmed colorectal liver metastases.
A tumour board, composed of oncologists, hepatobiliary surgeons and interventional radiologists, evaluated all patients.
Patient’s clinical data are reported in Table 1.
In all patients, biological systemic chemotherapy was stopped 3 days before DEBIRI and restart 4 days after procedure.
Indications for DEBIRI treatment were:
-
Complete resection/treatment of the primary tumour.
-
Histological confirmed hepatic-dominant metastatic colorectal cancer, non-suitable to surgical or thermo-ablation.
-
Progressive disease during or within 6 month from the end of second-line chemotherapy, irrespective of eventual maintenance treatment with bevacizumab.
Exclusion criteria were:
-
Patients with multiple systemic metastasis from colorectal cancer.
-
Liver metastatic involvement more than 50%.
-
Severe concomitant disease such as uncontrolled hypertension, congestive heart failure, uncontrolled diabetes.
In the pre-treatment work-up, a routine physical examination, laboratory tests and imaging studies were performed in order to evaluate inclusion/exclusion criteria: in particular, all patients underwent contrast-enhanced computed tomography (CT) (Innova 64Slides GE) within the 2 weeks preceding enrolment in order to confirm lesions and studying vascular supply to metastases.
The required minimum number of procedures was two, performed with a 4-week time interval.
The decision to repeat TACE was taken depending on tumour response according to the response evaluation criteria in solid tumours, evaluated with contrast-enhanced computed tomography (CT) after two treatments by two expert radiologists.
The ethics committee approved the study, and all patients signed a written informed consent prior to the procedure.
DEBIRI treatment
DEBIRI treatment was performed in an angiography suite (Artis Zee, Siemens) with monitoring of vital signs and anaesthesia care, by interventional radiologists with years of experience in interventional procedures at the time of beginning of this study.
The beads were previously preloaded with 200 mg of irinotecan by the pharmaceutical service in a sterile environment under a controlled atmosphere hood.
In order to reduce and control the pain related to DEBIRI that sometimes precluded subsequent procedures because of patient’s refusal, we adopted a specific pharmacological pain protocol.
4 h before treatment, the protocol provides 20 mg of morphine, 30 mg ketorolac and 100 mg of ranitidine infused by i.v. 24 h protracted continuous infusion plus 1,000 mg of paracetamol and 8 mg ondansetron hydrochloride 1 h before procedure.
After sterile covering of the inguinal region and injection of a local anaesthetic (lidocaine 1%), the right common femoral artery was punctured in standardized Seldinger technique and a 4-F sheath (Introducer 2VR, Terumo, Tokyo Japan) was introduced.
Using pre-procedure CT images as a reference, we catheterized with a 4 Fr catheter (Cobra 2 or Simmons 1 or 2 curves) the superior mesenteric artery or the coeliac trunk to reach the lesion afferent vessels. In the coeliac trunk, we advanced the catheter beyond the cystic artery. Then a diagnostic angiography was obtained to confirm our positions and visualize tumour’s vascularization as well as exclude any arteriovenous fistulae.
After positioning the catheter in the hepatic tumour-supplying vessel in superselective technique with a 2.7-Fr microcatheter (Progreat; Terumo, Tokyo, Japan), drug-eluting bead (75–150 μm and 100–300 μm) was slowly infused until the complete expected dose and stasis of the blood flow was observed.
The tumour vessels were occluded. After embolization, devascularization was confirmed with additional angiography from the common hepatic artery.
To control intraprocedural pain, at the beginning of the release of preloaded DC beads 3 ml i.v. bolus of morphine and ondansetron (Zofran) were infused; if necessary, we repeat from 2 ml up to maximum 10 ml morphine boluses and 2 ml of midazolam hydrochloride (midazolam) up to maximum 5 mg.
In this way, the pain was relieved, disappearing within 60 min from the procedure.
None of these patients needed an anaesthetic sedation.
After the endovascular treatment, all patients were observed with monitoring of central venous blood pressure, arterial pressure, heart rate and peripheral oxygen saturation.
Follow-up
The morphologic tumour response during the follow-up (number, location and size) was evaluated with contrast-enhanced computed tomography (CT), using RECIST 1.1 criteria by two expert radiologists.
The first follow-up imaging was performed 4 months after the second treatment: according to the evaluated response, further treatments were planned.
Subsequent follow-up contrast-enhanced computed tomography (CT) was performed at 8, 12 months and then once a year, until progression of the disease or patient death.
With the same frequency were carried out blood tests to assess liver and kidney function.
Definitions and end points
Technical success of DEBIRI was defined as the ability to catheterize the hepatic tumour-supplying vessel and delivers the planned dose (200 mg of irinotecan-loaded beads) until the stasis of blood flow.
Objective of our study was to assess the feasibility, safety, efficacy of chemoembolization with DEBIRI technique, in patients refractory to conventional scheduled FOLFOX and FOLFIRI chemotherapy.
Primary end points were evaluating morphologic tumour response during the follow-up (number, location and size) by contrast-enhanced computed tomography (CT) using RECIST 1.1 criteria as the sum of objective responses and stable diseases, and procedure’s tolerance, defined as a visual analogue scale (VAS) <7.
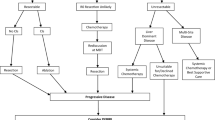
The secondary end point was to assess the medium and long-term survival, defined as the time between the start of treatment and the death from any cause, of patients receiving DEBIRI liver chemoembolization as third-line treatment for metastatic colorectal cancer (Figs. 1, 2, and 3).
Case N°1. a CT scan, single focal liver metastasis from colorectal cancer in the VIII segment, b selective embolization of the VIII segment, c final check with selective catheterization of the hepatic artery at the end of treatment DEBIRI: embolization of branches of VIII segment with stopping the flow, and d CT scan performed at 26 months follow-up demonstrates significant reduction of lesion
Case N°3. a CT scan, recurrent single focal liver metastasis from colorectal cancer in the VIII segment, previously treated with RF thermoablation, b selective embolization and DEBIRI treatment of the segment VIII, and c CT scan after 32 months demonstrates a hypodense necrotic metastasis in VIII segment
Results
Between October 2009 and January 2014, 192 chemoembolization (average 3.1 per patient, range 2–7) were performed with a 100% of technical success: all patients received the full dose planned.
Median hospitalization for DEBIRI was 72 h.
Treatment with TACE for liver metastases, in our experience, presents an efficacy of 37.1% defined as the sum of objective responses and stable diseases; in particular, to date, using RECIST 1.1 criteria, 7 patients were in remission of disease and 16 present stable disease.
No intra-/peri-procedural (within 30 days) death occurred.
All patients have had a post-embolization syndrome; in particular, 30 patients present nausea–vomiting and 15 present hypertransanaemia during the 3 days after the procedure (Table 2).
The assessment of the VAS, which indicates procedure’s tolerance, was performed 24 h after the procedure; for each single treatment; 58 patients (93.5%) declared TACE as tolerable procedure, with an intra- and post-operative pain acceptable (VAS < 7).
At 51 months, survival of patients subjected to DEBIRI liver chemoembolization was 27.5%.
Patients with KRAS wild-type and single-lobe metastases have a better prognosis; in particular, patients with KRAS wild-type presents median survival of 35 months respect a median survival of 23 months for KRAS mutated-type.
Discussion
Colorectal liver metastases represent the fourth most common malignant tumour entity and the second most common cause of cancer-related death in Western countries.
The presence and extent of liver metastases are a major prognostic factor for the overall survival. Actually resection is the only potentially curative therapy, but at diagnosis, only few patients will be candidates to surgery.
During last decade treatment, algorithms and survival expectations for these patients have changed, mainly as a consequence of the availability of new active drugs (oxaliplatin, irinotecan), molecularly targeted agents (bevacizumab, cetuximab/panitumumab) and new locoregional treatment of liver metastases (surgery or ablation), but their clinical outcome remains poor. Actually there is no standard third-line therapy for patients with metastatic colon cancer and even the use of regorafenib is debatable because of high costs for limited clinical benefit.
In this multimodal approach, the interventional radiologist has increasingly assumed a central role in the management of these patients.
Due to its specific architecture, normal liver parenchyma is largely supplied by the portal vein, whereas hepatic arterial branches predominantly supply malignant liver tumours [14].
Transarterial drug delivery into the liver allows, therefore, a considerably increased local therapeutic concentration compared with intravenously applied systemic chemotherapeutics. At the same time, healthy non-affected liver parenchyma can be spared with selective or superselective transarterial chemoembolization (TACE), and the liver toxicity that is observed after systemic applications is avoided or at least minimized.
The aim and efficacy of locoregional therapy of the liver are well known; however, its several side effects (biliary stenosis, catheter displacement and consequent systemic leakage) may undermine its application [15, 16].
In a multi-institutional study, Fiorentini et al. randomly assigned 74 patients to receive DEBIRI versus systemic irinotecan, fluorouracil and leucovorin; they compare DEBIRI versus systemic therapy in patients with non-resectable liver metastases from colorectal cancer and indicate that DEBIRI therapy prolonged the median survival (22 vs. 15 months). This suggests a benefit of DEBIRI treatment over standard chemotherapy [17].
DEBIRI can be performed also after several previous line of therapy, provided that an adequate supportive therapy is guaranteed. This point is crucial as the duration of hospitalization may be limited and tolerability of treatment (less abdominal pain, discomfort, serum transaminases level elevation) may be improved.
Intraoperative pain is one of the main causes of discomfort in patients treated with DEBIRI technique irinotecan; the chemotherapy infusion via intra-arterial is painful.
Our study, although presents some limitation as it is monocentric-retrospective approach, confirms that patients undergoing DEBIRI have a higher overall survival compared to data in the literature of untreated patients.
Favourable factors for overall survival were KRAS wild-type and unilobar metastases disease; these data also fit with the present literature.
Until 2009, peri- and intraprocedural pain was a strong issue for patients who, after an initial treatment, refused additional procedures DEBIRI. Therefore, in accordance with the tumour board, we tried to elaborate an analgesic protocol that would improve pain control.
The improvement of such protocol in use today at our hospital greatly reduces the patient’s discomfort: the number of patients who had strong peri-procedural pain was limited (18%) compared to the total number of treatments.
To better assess the actual tolerability of the procedure, the patients have completed a VAS after 24 h of treatment: a high percentage of treated patients (93.5%) have confirmed that the proposed analgesic protocol makes DEBIRI pain related acceptable, with a VAS <7.
Conclusion
During the last decades, interventional oncology is contributing towards the management of patients with liver metastases from colorectal cancer, in both palliative and adjunctive setting. Even though our study is limited by its retrospective design and small patient sample, in our experience DEBIRI of mCRLM in patients with liver-dominant disease appears an effective, safe, well-tolerated treatment and allowed to increase the survival rate of patients not responded at second-line chemotherapy.
References
Gruber-Rouh T, et al. Transarterial chemoembolization of unresectable systemic chemotherapy-refractory liver metastases from colorectal cancer: Long-term results over a 10-year period. Int J Cancer. 2014;134:1225–31.
Iezzi R, et al. Trans-arterial chemoembolization with irinotecan-loaded drug-eluting beads (DEBIRI) and capecitabine in refractory liver prevalent colorectal metastases: a phase II single-center study. Cardiovasc Intervent Radiol. 2015;38(6):1523–31. doi:10.1007/s00270-015-1080-9.
Abdalla EK, Adam R, Bilchik AJ, Jaeck D, Vauthey JN, Mahvi D. Improving resectability of hepatic colorectal metastases: expert consensus statement. Ann Surg Oncol. 2006;13:1271–80.
Arthur J. Richardson transarterial chemoembolization with irinotecan beads in the treatment of colorectal liver metastases: systematic review. J Vasc Interv Radiol. 2013;24:1209–17.
Tournigand C, André T, Achille E. FOLFIRI followed by FOLFOX6 or the reverse sequence in advanced colorectal cancer: a randomized GER-COR study. J Clin Oncol. 2004;22:229–37.
Prenen H, Van Cutsem E. Oncological manage- ment of unresectable liver metastases. Dig Dis. 2012;30(Suppl 2):137–42.
Konopke R, Roth J, Volk A, et al. Colorectal liver metastases: an update on palliative treatment options. J Gastrointestin Liver Dis. 2012;21:83–91.
Aliberti C, Tilli M, Benea G, Fiorentini G. Trans-arterial chemoembolization (TACE) of liver metastases from colorectal cancer using irinotecan-eluting beads: preliminary results. Anticancer Res. 2006;6:2795–3793.
Civalleri D, Esposito M, Fulco RA, Vannozzi M, Balletto N, DeCian F, et al. Liver and tumor uptake and plasma pharmacokinetic of arterial cisplatin administered with and without starch microspheres in patients with liver metastases. Cancer. 1991;68:988–94.
Soulen MC. Chemoembolization of hepatic malignancies. Oncology. 1994;8:77–84.
Martin RC, Joshi J, Robbins K, Tomalty D, Bosnjakovik P, Derner M, et al. Hepatic intra-arterial injection of drug- eluting bead, irinotecan (DEBIRI) in unresectable colorectal liver metastases refractory to systemic chemotherapy: results of multi- institutional study. Ann Surg Oncol. 2011;18:192–8.
Kemeny NE, et al. Hepatic arterial infusion versus systemic therapy for metastases from colorectal cancer: a randomized trial of efficacy, quality of life and molecular markers (CALGB 9481). J Clin Oncol. 2006;24:1395–403.
Martin RC, et al. Hepatic intra-arterial injectionof drug-eluting bead, irinotecan (DEBIRI) in unresectable colorectal liver metastases refractory to systemic chemotherapy: results of multi-institutional study. Ann Surg Oncol. 2011;18:192–8.
Breedis C, Young G. The blood supply of neoplasms in the liver. Am J Pathol. 1954;30(5):969–77.
Therasse P, Arbuck SG, Eisenhauer EA, et al. New guidelines to evaluate the response to treatment in solid tumors European organization for research and treatment of cancer, national cancer institute of the United States, national cancer institute of Canada. J Natl Cancer Inst. 2000;92:205–16. doi:10.1093/jnci/92.3.205.
Bruix J, Sherman M, Llovet JM, Beaugrand M, Lencioni R, et al. Clinical management of hepatocellular carcinoma conclusions of the Barcelona-2000 EASL conference. European Association for the Study of the Liver. J Hepatol. 2001;35:421–30. doi:10.1016/S0168-8278(01)00130-1.
Fiorentini G, et al. Intra-arterial infusion of irinotecan-loaded drug-eluting beads (DEBIRI) versus intravenous therapy (FOLFIRI) for hepatic metastases from colorectal cancer: final results of a phase III study. Anticancer Res. 2012;32:1387–96.
Scevola G, et al. DEBIRI handbook, rational, technique and case reports. Cap.9 Metastasis from colon rectum: treatment with DEBIRI and chemotherapy. Ed. 2012.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Ethical approval
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki Declaration and its later amendments or comparable ethical standards.
Informed consent
Informed consent was obtained from all individual participants included in the study.
Additional information
An erratum to this article is available at http://dx.doi.org/10.1007/s12032-017-0925-2.
Rights and permissions
About this article
Cite this article
Scevola, G., Loreni, G., Rastelli, M. et al. Third-line treatment of colorectal liver metastases using DEBIRI chemoembolization. Med Oncol 34, 37 (2017). https://doi.org/10.1007/s12032-017-0890-9
Received:
Accepted:
Published:
DOI: https://doi.org/10.1007/s12032-017-0890-9