Abstract
Serum miRNAs (miRs) have gained consideration as encouraging molecular markers for cancer diagnosis and prediction of prognosis. The authors aimed to identify the exact role of miR-17-5p, miR-125b, and miR-221 among glioblastoma multiforme (GBM) patients before and after standard treatment, and correlate their expression with survival pattern. The study included 25 GBM patients and 20 healthy controls. Serum miR-17-5p, miR-125b, and miR-221 expression were analyzed before and after treatment using quantitative real-time polymerase chain reaction (qPCR). The diagnostic efficacy for the tested miRs was evaluated using the receiver operating characteristic (ROC) curve, and the relation of miRs expression versus clinical criteria for GBM was assessed. Patients’ survival patterns were examined versus miRs expression levels. A significant difference was reported between miRs expression among the enrolled individuals. Both miR-17-5p and miR-221 reported significant elevations in GBM patients who: are above 60 years old, underwent biopsy resection, have a non-frontal lesion, with tumor size above 5 cm, and with performance status equals 2 according to the Eastern Cooperative Oncology Group (ECOG) Performance Status. With regard to miR-125b, a significant difference was detected according to surgery strategy, primary lesion of the tumor, and ECOG status. MiRs levels were significantly decreased for GBM patients after treatment. Survival patterns demonstrated an increase in miR-17-5p, miR-125b, and miR-221 in GBM patients with worse progression-free survival and among those with worse overall survival. Detection of serum miR-17-5p, miR-125b, and miR-221 aids in the prediction of prognosis and response to treatment strategy for GBM patients.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Glioblastoma multiforme (GBM) is a fatal type of cancer that affects the central nervous system and has no curative treatment (Dahlrot et al. 2013, Zeng et al. 2017). Age is recorded as a risk factor for GBM (Vartanian et al. 2014) and the reported median survival for GBM patients is 12 to 15 months after diagnosis (Li et al. 2017). Proliferation and invasive angiogenesis are the most common features of GBM (Zhang et al. 2017). GBM is detected by conventional neuroimaging. Nevertheless, it is considered as an invasive and expensive process that has an unwarrantable accuracy (Mabray et al. 2015, Shiroishi et al. 2016). Due to the fact of infiltrative growth in GBM, surgical resection is only used as a palliative therapy (Mitchell et al. 2005). It is worth mentioning also that GBM patients might suffer from resistance to chemotherapy (Stupp et al. 2009).
The miRNAs (miRs) are present in blood, and recently they are being viewed as an imperative tool to overcome invasive detection techniques and resistance to chemotherapy. They are commonly considered to be perfect biomarkers for clinical use (Pichler and Calin 2015). MiRs are a large class of 18–25 nuclear non-coding RNAs that are endogenously expressed (Rolle 2015, Shea et al. 2016). These molecules can link to RNA and cause transnational silencing or degradation, hence inhibiting gene expression (Zeng, Yin, Li et al. 2018a). Several studies have examined miRs in GBM with regard to their expression levels and roles, in order to gain fresh insight into how to treat this disease (Zeng, Yin, Wang et al. 2018b). MiRs have been identified as obviously specified markers that can be identified readily by means of microarrays or polymerase chain reactions (PCR) in peripheral blood (Dong et al. 2014).
Among the oncogenic miRs are miR-125b, miR-17-5p, and miR-221-3p. With regard to miR-125b, its molecular dysfunction is related to cancer-associated inflammation (Tili et al. 2013). It is involved in the proliferation, apoptosis, and invasion of cancer cells, and is considered a significant drug resistance modulator (Sun et al. 2013). These proliferative and anti-apoptotic effects influence nuclear factor kappa B (NF-kB) activity, which in turn affects DNA, cytokines, and response to temozolomide (TMZ) in GBM patients (Haemmig et al. 2014).
The miR-17-92 cluster is composed of seven mature miRs (miR-17-5p, miR-19a, miR-92-1, miR-17-3p, miR- 20a, miR-18a, and miR-19b) that affect multiple regulatory pathways (Coller et al. 2007, Ernst et al. 2010). Relative to its expression in the normal brain, miR-17-5p is unique in secondary GBM (Sasaki et al. 2010). It has been previously demonstrated that miR-17-5p inhibits GBM cell proliferation. Accordingly, the survival of patients with higher miR-17-5p is longer than those with lower miR-17-5p expression levels (Zeng, Yin, Wang et al. 2018b). This could be attributed to the ability of miR-17-5p to target PTEN (Xie et al. 2014) that is known to suppress tumors (Morales et al. 2014).
On the other hand, miR-221 and miR-222 are very comparable. They are often present as a gene cluster (miR-221/222), and have been widely studied for numerous human disorders (Song et al. 2017). MiR-221 was upregulated in GBM and is reported to induce cell death. It has been shown to be overexpressed in glioma cells leading to an increase in DNA damage markers (Quintavalle et al. 2013). In the current study, we aimed at assessing the role of serum miR-17-5p, miR-221, and miR-125b as prospective non-invasive instruments to diagnose GBM, and examining their function in response lto therapy and survival in GBM patients.
Materials and methods
Ethical approval and consent to participate
After obtaining approval from the Medical Ethical Committee from National Research Centre (ID 17111) on the study and after all individuals had signed their written informed consent; blood samples were collected from all individuals.
Study population
Our study involved 25 patients (16 males, 9 females) diagnosed with GBM from the Clinical Oncology Department, Faculty of Medicine, Ain Shams University, Egypt, in addition to 20 healthy volunteers. Serum samples were withdrawn at diagnosis and after completion of the treatment protocol for those who fulfilled the inclusion criteria as newly diagnosed GBM cancer patients with age more than 18 years and a performance score less than or equal 2 according to the Eastern Cooperative Oncology Group (ECOG) Performance Status. Any GBM patient who did not fulfill the inclusion criteria was excluded from the study. GBM patients then received their standardized treatment protocols, which included radiotherapy (total dose of 60 Gy, given in 30 fractions over 6 weeks) with concomitant temozolomide (TMZ) chemotherapy (75 mg/day for 45 days), followed by six cycles of TMZ treatment at a dose of 150 mg/sq.m body surface area. After the last cycle of the treatment strategy, other blood samples were collected from GBM patients, who were followed up at regular intervals and evaluated clinically and radiologically by MRI with contrast.
Sample processing
Blood samples were taken from study subjects (3 ml each) into polymer gel tubes with clot activator (Greiner Bio-One GmbH, Australia). Clotting took place over 30 min at room temperature, followed by centrifugation at 10,000×g for 10 min at 4 °C. Serum was stored at −80 °C in aliquots for further analysis of miRs.
RNA isolation
MiRNA extraction was performed using miRNeasy Mini kit (Catalog # 217004, Qiagen, USA). Briefly; the lysis reagent was added to thawed serum (1:5) then left for 5 min at room temperature; afterwards, a volume of chloroform was added to the tubes (1:1). Samples were then centrifuged at 12,000×g for 15 min at 4 °C (13-18KS, Sigma, Germany), and after removing the upper aqueous phase to a new tube, 1.5 volumes of 100% ethanol were added. Samples were transferred into an RNeasy Mini spin column in 2-ml collection tubes and centrifuged for 15 s at ≥ 8000×g at room temperature. The RWT buffer (700 μl) was added to the RNeasy Mini spin columns. After centrifugation, the flow-through was discarded, RPE buffer (500 μl) was added, columns were then centrifuged and the flow-through was discarded. RNase-free water (30 μl) was directly added onto the RNeasy Mini spin column membranes, and centrifugation was done for 1 min at ≥ 8000×g. The purity and the concentration of the purified miRs were detected using spectrophotometer Nano-drop (Quawell, Q-500, Scribner, USA), and samples were stored at −80 °C till further assessments.
Reverse transcription and cDNA preparation
Synthesis of complementary DNA (cDNA) was done using MiScript II reverse transcription kit (Cat number # 218160, Qiagen, USA). A total volume of 20 μl of reverse transcription reaction components as follows: 4 μl MiScript HiFlex buffer, 2 μl nucleic mixture, 2 μl MiScript RT mixture, and RNase-free water and template of purified miRNA with adjusted concentration 100 ng/reaction were used. The PCR tubes were then placed in the thermal cycler (SureCycler 8800, Agilent, USA), and the transcription profile was adjusted for 60 min at 37 °C and then 5 min at 95 °C to inactivate miScript reverse transcriptase mixture. Purity and concentration of cDNA were detected using spectrophotometer Nano-drop (Quawell, Q-500, Scribner, USA) and it was stored at −20 °C till performing quantitative real-time PCR (qPCR).
Quantitative real-time PCR (qPCR)
Quantification of the investigated miRs was performed using miScript SYBR Green PCR kit (# 218073, Qiagen, USA) following the manufacturer’s protocol using the following primers; miR-17-5p (Hs_miR_17_2 miScript Primer Assay, MS00029274), miR-125b (Hs_miR-125b_1 miScript Primer Assay MS00006629) and miR-221 (Hs_miR_221_2 miScript Primer Assay, MS00003857). Normalization of the expression levels of the investigated miRs was performed using RNU6–2 (Hs_RNU6–2_11 miScript Primer Assay: MS00033740) as an endogenous control. The concentration of cDNA was adjusted at 2 ng/ml, and a total volume of 20 μl was used for the assay. Assay steps were carried out as per the manufacturer’s protocol. Simply, reactions were incubated in a 96-well plate at 95 °C for 15 min. A total of 40 cycles were performed where each cycle was as follows; 15 s at 94 °C, 30 s at 55 °C and 34 s at 70 °C. The acquired fluorescence was measured by Stratagene Real-time PCR System (Max3005P qPCR System, Stratagene, Agilent Biotechnology, USA).
Calculations of fold changes were performed following the ΔCt method, where ΔCt’s represented the differences in the cycle threshold numbers between the investigated miRs and the endogenous control RNU6–2. The change in the differences between the examined miRs among the GBM patients and the healthy controls was represented by ΔΔCt (Livak and Schmittgen 2001).
Statistical analysis
Data were analyzed using SPSS (version 24 SPSS, Inc., Chicago USA), and p-values were two-tailed and considered significant if <0.05. The fold change in investigated miRs was calculated using the equation of 2-ΔΔCT. Chi-square tests were used to detect the variations between categorical variables. The association between the clinicopathological and demographic factors with investigated miRs was determined by ANOVA. A receiver operating characteristic (ROC) curve was plotted between GBM patients and healthy individuals to detect the sensitivities and the specificities for the miRs, and their clinical efficacy (Zweig and Campbell 2014). Progression-free survival (PFS) was reported as the time from the first receival of the neoadjuvant treatment strategy to distal, regional, or local recurrence. Overall survival (OS) was measured from the date of first diagnosis to the date of last follow-up or death of the patient, both of which were analyzed using the Kaplan–Meier statistical method, and compared by a log-rank test.
Results
In the current prospective study, a total of 45 individuals were enrolled; 20 individuals served as healthy controls, and 25 individuals were diagnosed with GBM. Both groups were of matched ages and followed the inclusion criteria. No significant differences were reported among the enrolled individuals regarding their gender status as 12 cases were females (26.7%), three of them were control, and the rest were GBM patients. Males were 33 (73.3%); 17 participants were control, and the rest were patients with GBM. With regard to the age of individuals, 30 were below 60 year-old (17 controls and 13 GBM patients), and 15 were above or equal to 60 year-old (three controls and 12 GBM patients) as reported in Table 1.
Expression of assessed miRs among the enrolled individuals
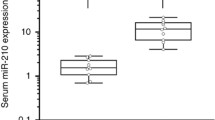
Plotting the ROC curve revealed the following sensitivities and specificities; 96%, 95% with AUC 0.988 [SE = 0.015], 92%, 100% with AUC 0.992 [SE = 0.013], and 88%, 100%, with AUC 0.956 [SE = 0.03] for miR-17-5p, miR-125b, and miR-221 respectively as depicted in Fig. 1. Statistical significance was achieved between miRs levels in control individuals versus GBM cases as plotted in Fig. 2a-c.
Expression level of the investigated miRs among the enrolled individuals. a Expression level of miR-17-5p at mean 85 for control individuals and 186 for GBM (F = 44, p < 0.0001). b Expression level of miR-125b at mean 15 for control individuals and 171 for GBM (F = 61, p < 0.0001). c Expression level of miR-221 at mean 5.7 for control individuals and 38.6 for GBM (F = 27.8, p < 0.0001)
Mean levels of the investigated miRs among clinical criteria
As summarized in Table 2, increased level of miR17-5p was statistically significant with GBM patients over 60 years of age, tumor size above 5 cm, non-frontal lesions, GBM patients who underwent biopsy sample resection as a surgical protocol, and patients with ECOG equal to 2. Moreover, the level of the aforementioned miR was higher in female patients relative to their male counterparts; however, the difference has not achieved statistical significance. For miR-125b, a significant increase was demonstrated among patients who underwent biopsy resection of the tumor, and those with ECOG equal to 2. Meanwhile, the relationship between miR-125b and the site of the primary tumor lesion reported a p value of 0.049. Regarding miR-221, significant changes in its expression level were reported in relation to all clinical characteristics apart from gender status as summarized in Table 2.
Relation between miRs expression and treatment strategy
The investigated miRs were measured among GBM patients before and after treatment. The results are as follows; 182 ± 24.7 versus 24.7 ± 1.6 at F = 45.5, p < 0.001 for miR-17-5p; 171.8 ± 17.8 versus 65 ± 8 at F = 29.5, p < 0.001 for miR-125b; and 38.2 ± 5.4 versus 7.2 ± 1.8 at F = 28.8, p < 0.001 for miR-221.
Impact of miRs expression on response to treatment
Mean levels of the investigated miRs were reported with different response categories [complete response (CR), partial response (PR), stable disease (SD), and progressive disease (PD)] in Table 3. When patients were categorized as responders (CR, PR, and SD) and non- responders (PD), the results revealed sensitivity and specificity for miR-17-5p as 50.5% and 100%, for miR-125b as 52.9% and 100%, for miR-221 as 76.5% and 100% respectively. Significant differences were reported in miR-17-5p and miR-221 levels, and response to treatment as shown in Table 3.
Prediction power of miRs in survival patterns
By using the mean level for miR-17-5p as 186-fold change, miR-125b as 171.8-fold change, and miR-221 as 139-fold change, the GBM patients were divided into those above or below the mean level of miR expression. As shown in Fig. 3a-c, a significant difference was reported between miR-17-5p, miR-125b, and miR-221 with PFS. GBM patients with low expression levels reported better PFS as compared to their counterparts with high expression levels. Similarly, expression of miR-17-5p, miR-125b, and miR-221 reported significant differences with OS, where GBM patients with better OS showed significantly lower expression level (Fig. 4a-c).
Discussion
Recently, endogenous circulating miRs have comprised a widespread research interest not only for being stable against harsh conditions (Sohel 2016), but also due to the potential of newer techniques, for example nanotechnology-based methods to detect their levels, providing a sensitive tool capable of overcoming the limitations of the currently implicated techniques (Chaudhary et al. 2018, Zhang et al. 2019). The authors have previously studied the expression of some miRs in several types of cancer (Swellam, El Magdoub et al. 2018a, Swellam, Hashim et al. 2018b, Swellam and Ramadan 2019) among which was GBM (Swellam, Ezz El Arab et al. 2019), and reported their usefulness as molecular markers for early detection and prediction of prognosis. In the current study, the authors examined the expression levels of miR-17-5p, miR-125b, and miR-221. Previous studies have reported the role of these miRs in carcinogenesis being categorized as oncomiRs (Bobbili et al. 2017, Jiang et al. 2018, Kong et al. 2018, Kiener et al. 2019).
Hereby, we reported a significantly higher expression level of the investigated miRs in GBM patients as compared to healthy individuals. From a clinical standpoint, aberrant expression of miRs has been readily identified in biological fluids in cancer patients, highlighting the importance of their stability, and offering a rationale for improving efficient liquid biopsy molecular markers for cancer diagnosis. In the current study, no significant difference among the enrolled individuals (n = 45) with regard to their gender or age was reported.
The mean expression levels of the indicated miRs were examined in relation to the clinical criteria of GBM patients. A significant difference is hereby reported between miR-17-5p and miR-221 on one hand and patient age on the other, as those above 60 years of age have demonstrated an increased expression of the two miRs. These results point out the characteristic dysregulated molecular profile of elderly GBM patients (Crespo et al. 2015). The higher, yet insignificant level of miR-17-5p in female patients versus male ones requires further probing, especially in light of previous studies negating any significant gender-based differences in the level of this miR in other types of cancer (Chen et al. 2013, Mooney et al. 2015). Currently, a study with a larger number of GBM patients is in progress, which could possibly negate or confirm the observed difference.
Patients were classified into two groups based on the site of primary lesion as tumor at the frontal site (n = 12) versus other non-frontal sites (n = 13). An increased expression level of the investigated miRs was detected among those with non-frontal site lesion. Increased expression of these oncomiRs denotes the aggressiveness of their tumors (Delangle et al. 2019). Hence, it was demonstrated that miR-17-5p and miR-221 expression levels in relation to the site of tumor play a role as predictors of prognosis, that is, because a decreased expression level was reported among GBM patients with frontal site lesions, which predisposed those patients to complete surgical resection (Paldor et al. 2016). These data are in accord with our results, as the expression level of the investigated miRs was significantly lower in those who underwent a complete resection with better prognosis, indicating the usefulness of these miRs as a potential reliable tool for the prediction of GBM prognosis. Moreover, a survival analysis of 106 patients has demonstrated a poor prognosis, with high levels of miR-17-5p (Zhao et al. 2017). However, it should be noted that some other investigators have demonstrated contradictory findings, where a high level of this miR was associated with a better outcome in GBM patients who underwent surgical treatment (Yuan et al. 2017).
Moreover, the results of the current work elucidate a significant relation with ECOG, a useful indicator for tumor performance (Lee et al. 2018). This could be explained in light of the fact that the investigated miRs have shown significantly lower levels with ECOG less than 2, indicating the possible role of those liquid biopsy samples as predictors for better prognosis.
It is believed nowadays that liquid biopsies are likely to become an additional standard for monitoring progressive genomic alterations over tumor evolution, and the enrollment of liquid biopsy samples for the diagnosis, prognostication, and prediction of treatment response is becoming of great importance (Hench et al. 2018). Significant reductions in the expression levels of the three investigated miRs (miR-17-5p, miR-125b, and miR-221) were reported after treatment, as shown in Table 3. Furthermore, those with CR reported a significantly inferior expression level, as shown in Table 4, indicating the possible role of miRs as potential predictors of response to treatment and presuming the prognostication status of GBM patients.
After GBM patients had received their standard care of treatment, they were subject to further follow-up, and MRIs were re-analyzed to reduce intra-observer variability and offer consistency. Accordingly, and as plotted in Figs. 3 and 4, miRs expression levels revealed significant differences, where statistically significant lower expression levels were reported among patients with better PFS and OS. These results emphasize the crucial clinical role of the investigated miRs for prediction of survival behavior in GBM patients.
Conclusion
Assessment of miRs expression in liquid biopsy samples for detection of solid tumors, prediction of response to treatment, and survival pattern is of great interest, not only because of its minimal/non-invasive nature, but also because miRs are stable and can be used in monitoring patients’ responses to treatment in a cost-effective manner compared to conventional traditional techniques.
References
Bobbili MR, Mader RM, Grillari J, Dellago H (2017) OncomiR-17-5p: alarm signal in cancer? Oncotarget 8(41):71206–71222
Chaudhary V, Jangra S, Yadav NR (2018) Nanotechnology-based approaches for detection and delivery of microRNA in healthcare and crop protection. J Nanobiotechnology 16(1):40
Chen Q, Si Q, Xiao S, Xie Q, Lin J, Wang C, Chen L, Wang L (2013) Prognostic significance of serum miR-17-5p in lung cancer. Med Oncol 30(1):353
Coller HA, Forman JJ, Legesse-Miller A (2007) "Myc'ed messages": myc induces transcription of E2F1 while inhibiting its translation via a microRNA polycistron. PLoS Genet 3(8):e146
Crespo I, Vital AL, Gonzalez-Tablas M, Patino Mdel C, Otero A, Lopes MC, de Oliveira C, Domingues P, Orfao A, Tabernero MD (2015) Molecular and genomic alterations in glioblastoma multiforme. Am J Pathol 185(7):1820–1833
Dahlrot RH, Hermansen SK, Hansen S, Kristensen BW (2013) What is the clinical value of cancer stem cell markers in gliomas? Int J Clin Exp Pathol 6(3):334–348
Delangle R, De Foucher T, Larsen AK, Sabbah M, Azais H, Bendifallah S, Darai E, Ballester M, Mehats C, Uzan C, Canlorbe G (2019) The use of microRNAs in the management of endometrial cancer: a meta-analysis. Cancers 11(6):832
Dong L, Li Y, Han C, Wang X, She L, Zhang H (2014) miRNA microarray reveals specific expression in the peripheral blood of glioblastoma patients. Int J Oncol 45(2):746–756
Ernst A, Campos B, Meier J, Devens F, Liesenberg F, Wolter M, Reifenberger G, Herold-Mende C, Lichter P, Radlwimmer B (2010) De-repression of CTGF via the miR-17-92 cluster upon differentiation of human glioblastoma spheroid cultures. Oncogene 29(23):3411–3422
Haemmig S, Baumgartner U, Gluck A, Zbinden S, Tschan MP, Kappeler A, Mariani L, Vajtai I, Vassella E (2014) miR-125b controls apoptosis and temozolomide resistance by targeting TNFAIP3 and NKIRAS2 in glioblastomas. Cell Death Dis 5:e1279
Hench IB, Hench J, Tolnay M (2018) Liquid biopsy in clinical management of breast, lung, and colorectal cancer. Front Med 5:9–9
Jiang Y, Luan Y, Chang H, Chen G (2018) The diagnostic and prognostic value of plasma microRNA-125b-5p in patients with multiple myeloma. Oncol Lett 16(3):4001–4007
Kiener M, Chen L, Krebs M, Grosjean J, Klima I, Kalogirou C, Riedmiller H, Kneitz B, Thalmann GN, Snaar-Jagalska E, Spahn M, Kruithof-de Julio M, Zoni E (2019) miR-221-5p regulates proliferation and migration in human prostate cancer cells and reduces tumor growth in vivo. BMC Cancer 19(1): 627
Kong W, Cheng Y, Liang H, Chen Q, Xiao C, Li K, Huang Z, Zhang J (2018) Prognostic value of miR-17-5p in cancers: a meta-analysis. Onco Targets Ther 11:3541–3549
Lee J, Park SH, Kim YZ (2018) Prognostic evaluation of neurological assessment of the neuro-oncology scale in glioblastoma patients. Brain Tumor Res Treat 6(1):22–30
Li S, Zeng A, Hu Q, Yan W, Liu Y, You Y (2017) miR-423-5p contributes to a malignant phenotype and temozolomide chemoresistance in glioblastomas. Neuro-Oncol 19(1):55–65
Livak KJ, Schmittgen TD (2001) Analysis of relative gene expression data using real-time quantitative PCR and the 2(−Delta Delta C(T)) method. Methods 25(4):402–408
Mabray MC, Barajas RF Jr, Cha S (2015) Modern brain tumor imaging. Brain Tumor Res Treat 3(1):8–23
Mitchell P, Ellison DW, Mendelow AD (2005) Surgery for malignant gliomas: mechanistic reasoning and slippery statistics. Lancet Neurol 4(7):413–422
Mooney C, Raoof R, El-Naggar H, Sanz-Rodriguez A, Jimenez-Mateos EM, Henshall DC (2015) High throughput qPCR expression profiling of circulating MicroRNAs reveals minimal sex- and sample timing-related variation in plasma of healthy volunteers. PLoS One 10(12):e0145316
Morales LD, Casillas Pavon EA, Shin JW, Garcia A, Capetillo M, Kim DJ, Lieman JH (2014) Protein tyrosine phosphatases PTP-1B, SHP-2, and PTEN facilitate Rb/E2F-associated apoptotic signaling. PLoS One 9(5):e97104
Paldor I, Pearce FC, Drummond KJ, Kaye AH (2016) Frontal glioblastoma multiforme may be biologically distinct from non-frontal and multilobar tumors. J Clin Neurosci 34:128–132
Pichler M, Calin GA (2015) MicroRNAs in cancer: from developmental genes in worms to their clinical application in patients. Br J Cancer 113(4):569–573
Quintavalle C, Mangani D, Roscigno G, Romano G, Diaz-Lagares A, Iaboni M, Donnarumma E, Fiore D, De Marinis P, Soini Y, Esteller M, Condorelli G (2013) MiR-221/222 target the DNA methyltransferase MGMT in glioma cells. PLoS One 8(9):e74466
Rolle K (2015) miRNA multiplayers in glioma. From bench to bedside. Acta Biochim Pol 62(3):353–365
Sasaki K, Kohanbash G, Hoji A, Ueda R, McDonald HA, Reinhart TA, Martinson J, Lotze MT, Marincola FM, Wang E, Fujita M, Okada H (2010) miR-17-92 expression in differentiated T cells - implications for cancer immunotherapy. J Transl Med 8:17
Shea A, Harish V, Afzal Z, Chijioke J, Kedir H, Dusmatova S, Roy A, Ramalinga M, Harris B, Blancato J, Verma M, Kumar D (2016) MicroRNAs in glioblastoma multiforme pathogenesis and therapeutics. Cancer Med 5(8):1917–1946
Shiroishi MS, Boxerman JL, Pope WB (2016) Physiologic MRI for assessment of response to therapy and prognosis in glioblastoma. Neuro-Oncol 18(4):467–478
Sohel MH (2016) Extracellular/circulating MicroRNAs: release mechanisms, functions and challenges. Achiev Life Sci 10(2):175–186
Song J, Ouyang Y, Che J, Li X, Zhao Y, Yang K, Zhao X, Chen Y, Fan C, Yuan W (2017) Potential value of miR-221/222 as diagnostic, prognostic, and therapeutic biomarkers for diseases. Front Immunol 8:56
Stupp R, Hegi ME, Mason WP, van den Bent MJ, Taphoorn MJ, Janzer RC, Ludwin SK, Allgeier A, Fisher B, Belanger K, Hau P, Brandes AA, Gijtenbeek J, Marosi C, Vecht CJ, Mokhtari K, Wesseling P, Villa S, Eisenhauer E, Gorlia T, Weller M, Lacombe D, Cairncross JG, Mirimanoff RO (2009) Effects of radiotherapy with concomitant and adjuvant temozolomide versus radiotherapy alone on survival in glioblastoma in a randomised phase III study: 5-year analysis of the EORTC-NCIC trial. Lancet Oncol 10(5):459–466
Sun YM, Lin KY, Chen YQ (2013) Diverse functions of miR-125 family in different cell contexts. J Hematol Oncol 6:6
Swellam M, Ramadan A (2019). Clinical significance of blood-based miRNAs as diagnostic and prognostic nucleic acid markers in breast cancer: comparative to conventional tumor markers. J Cell Biochem 120(8): 12321–12330
Swellam M, El Magdoub HM, Hassan NM, Hefny MM, Sobeih ME (2018a) Potential diagnostic role of circulating MiRNAs in breast cancer: implications on clinicopathological characters. Clin Biochem 56:47–54
Swellam M, Hashim M, Mahmoud MS, Ramadan A, Hassan NM (2018b) Aberrant expression of some circulating miRNAs in childhood acute lymphoblastic leukemia. Biochem Genet 56(4):283–294
Swellam M, Ezz El Arab L, Al-Posttany AS, Said SB (2019) Clinical impact of circulating oncogenic MiRNA-221 and MiRNA-222 in glioblastoma multiform. J Neuro-Oncol 144(3):545–551
Tili E, Michaille JJ, Croce CM (2013) MicroRNAs play a central role in molecular dysfunctions linking inflammation with cancer. Immunol Rev 253(1):167–184
Vartanian A, Singh SK, Agnihotri S, Jalali S, Burrell K, Aldape KD, Zadeh G (2014) GBM's multifaceted landscape: highlighting regional and microenvironmental heterogeneity. Neuro-Oncol 16(9):1167–1175
Xie Q, Yan Y, Huang Z, Zhong X, Huang L (2014) MicroRNA-221 targeting PI3-K/Akt signaling axis induces cell proliferation and BCNU resistance in human glioblastoma. Neuropathology 34(5):455–464
Yuan GQ, Wei NL, Mu LY, Wang XQ, Zhang YN, Zhou WN, Pan YW (2017) A 4-miRNAs signature predicts survival in glioblastoma multiforme patients. Cancer Biomark 20:443–452
Zeng AL, Yan W, Liu YW, Wang Z, Hu Q, Nie E, Zhou X, Li R, Wang XF, Jiang T, You YP (2017) Tumour exosomes from cells harbouring PTPRZ1-MET fusion contribute to a malignant phenotype and temozolomide chemoresistance in glioblastoma. Oncogene 36(38):5369–5381
Zeng A, Yin J, Li Y, Li R, Wang Z, Zhou X, Jin X, Shen F, Yan W, You Y (2018a) miR-129-5p targets Wnt5a to block PKC/ERK/NF-kappaB and JNK pathways in glioblastoma. Cell Death Dis 9(3):394
Zeng A, Yin J, Wang Z, Zhang C, Li R, Zhang Z, Yan W, You Y (2018b) miR-17-5p-CXCL14 axis related transcriptome profile and clinical outcome in diffuse gliomas. Oncoimmunology 7(12):e1510277
Zhang C, Cheng W, Ren X, Wang Z, Liu X, Li G, Han S, Jiang T, Wu A (2017) Tumor purity as an underlying key factor in glioma. Clin Cancer Res 23(20):6279–6291
Zhang Y, Li M, Gao X, Chen Y, Liu T (2019) Nanotechnology in cancer diagnosis: progress, challenges and opportunities. J Hematol Oncol 12(1):137
Zhao H, Shen J, Hodges TR, Song R, Fuller GN, Heimberger AB (2017) Serum microRNA profiling in patients with glioblastoma: a survival analysis. Mol Cancer 16(1):59–59
Zweig PL, Campbell RA (2014) Response to "drug shortages and the burden of access to care: a critical issue affecting patients with cancer". Clin J Oncol Nurs 18(2):143–145
Acknowledgments
The instruments listed in the current study were purchased through a grant from Science and Technology Development Fund (STDF) through Capacity Building Grant Fund (CBG) [No. 4940].
Author information
Authors and Affiliations
Contributions
Study conception and design: MS; NMB; HME; MSH and LRE. Provision of samples and clinical follow-up: LRE. Acquisition of data: NMB; HME; MSH and LRE. Analysis and interpretation of data: MS; NMB; HME and MSH. Drafting of manuscript: MS; NMB; HME and MSH. Critical revision: MS; NMB; HME; MSH and LRE.
Corresponding author
Ethics declarations
Conflict of interests
Authors confirmed that there is nothing to declare.
Ethical approval and consent to participate
were obtained from Medical Ethical Committee from National Research Centre (ID 17111), and all individuals signed their written informed consent.
Consent for publication
Authors agreed to publish work after finalizing the manuscript.
Availability of supporting data
No availability of sharing of data.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Swellam, M., Bakr, N.M., El Magdoub, H.M. et al. Emerging role of miRNAs as liquid biopsy markers for prediction of glioblastoma multiforme prognosis. J Mol Neurosci 71, 836–844 (2021). https://doi.org/10.1007/s12031-020-01706-5
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12031-020-01706-5