Abstract
Alzheimer’s disease (AD) is a neurodegenerative disorder characterized by extracellular deposits of fibrillary β-amyloid (Aβ) plaques in the brain that initiate an inflammatory process resulting in neurodegeneration. The neuronal loss associated with AD results in gross atrophy of affected regions causing a progressive loss of cognitive ability and memory function, ultimately leading to dementia. Growing evidence suggests that vasoactive intestinal peptide (VIP) could be beneficial for various neurodegenerative diseases, including AD. The study investigated the effects of VIP on 5xFAD, a transgenic mouse model of AD. Toward this aim, we used 20 5xFAD mice in two groups (n = 10 each), VIP-treated (25 ng/kg i.p. injection, three times per week) and saline-treated (the drug’s vehicle) following the same administration regimen. Treatment started at 1 month of age and ended 2 months later. After 2 months of treatment, the mice were euthanized, their brains dissected out, and immunohistochemically stained for Aβ40 and Aβ42 on serial sections. Then, plaque analysis and stereological morphometric analysis were performed in different brain regions. Chronic VIP administration in 5xFAD mice significantly decreased the levels of Aβ40 and Aβ42 plaques in the subiculum compared to the saline treated 5xFAD mice. VIP treatment also significantly decreased Aβ40 and Aβ42 plaques in cortical areas and significantly increased the hippocampus/cerebrum and corpus callosum/cerebrum ratio but not the cerebral cortex/cerebrum ratio. In summary, we found that chronic administration of VIP significantly decreased Aβ plaques and preserved against atrophy for related brain regions in 5xFAD AD mice.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Alzheimer’s disease (AD), clinically characterized by progressive memory loss and cognitive decline, is the most common neurodegenerative disorder. Senile plaques and neurofibrillary tangles are the pathological hallmarks of AD. Senile plaques consist of extracellular deposits of insoluble, aggregated Aβ peptide surrounded by microglia, reactive astrocytes, and dystrophic neurites. Aβ peptide is constitutively produced during cell metabolism by sequential proteolytic cleavage of the amyloid precursor protein (APP) by β-secretase and presenilin-dependent γ-secretase to yield Aβ42 and Aβ40 (Bayer et al. 2001). The amyloid cascade hypothesis of AD maintains that the accumulation of Aβ protein, due to an imbalance between its production and clearance, is the critical event in disease pathogenesis (Hardy 2002). Accumulation of aggregated amyloid fibrils, which are toxic form of the protein responsible for disrupting the cell’s calcium ion homeostasis, induce apoptosis. Furthermore, severe inflammation develops around the extracellular Aβ deposits (Meraz-Ríosv et al. 2013). The Aβ plaques activate microglia and astrocytes that, when activated, release proinflammatory cytokines, chemokines, and other toxic material, including free oxygen radicals and proteases (Solito and Sastre 2012; Gonzales-Reyes et al. 2017). Over time, this inflammatory process contributes to in neurodegeneration. The disease primarily affects the hippocampus and neocortex, causing progressive loss in cognitive ability and memory function, finally leading to dementia. The neuronal loss associated with AD results in the gross atrophy of the affected regions. Currently, there are no treatments to halt or reverse the progression of AD. Therefore, therapeutic agents that target these inflammatory processes could present great potential against AD pathophysiology.
One of the strongest arguments for the amyloid hypothesis derives from genetic studies that brought to light many familial AD (FAD) cases that resulted from inherited APP or PS1 mutations leading to increased deposition of Aβ in plaques (Bertram et al. 2010). Moreover, age-dependent pathology, which is developed by transgenic mouse models of AD containing the human APP gene with FAD mutations, is similar to that seen in AD (Philipson et al. 2010). The 5xFAD mouse model of AD is a double transgenic APP/PS1 mouse model that co-expresses five FAD mutations leading to faster plaque formation and increased AβX-42 production (Oakley et al. 2006). 5xFAD mice generate Aβ42 almost exclusively and rapidly accumulate massive cerebral Aβ deposits. In these mice, myloid deposition starts at 1–2 months age and reaches a very large load, particularly in the subiculum and cortical areas (Oakley et al. 2006). Aβ is typically generated throughout life, but the physiological roles of this peptide remain unknown. However, Aβ production and secretion is stimulated by synaptic activity which is the most unique and usual role of the nervous system. Therefore, the generation of the small Aβ peptide is not naturally toxic and might even play an important physiological role, while amyloid plaques composed of a multitude of extremely aggregated Aβ fibrils symbolizes an abnormal pathological lesion (Gouras et al. 2015).
Vasoactive intestinal peptide (VIP) is a basic 28-amino acid peptide that contributes to numerous tissue protective processes such as antioxidant, antiapoptotic, antiglutamatergic, anti-inflammatory, microglial, and astrocytic cell regulation, and has neurotrophic and neuroprotective properties (Deng and Jin 2017). In addition to these features, VIP can cross the blood–brain barrier (BBB) by unsaturated diffusion transport (Dogrukol-Ak et al. 2003). Based on its multidimensional abilities, VIP could be a good candidate for drug design research for various neurodegenerative diseases, including AD. However, there is limited data on the effects of VIP/VIP analogues on AD pathology. In vitro treatment with an analogue of VIP completely prevented cell death from Aβ toxicity (Gozes et al. 1996). Additionally, in the same study, the authors showed that intranasal or intracerebroventricular treatment with the VIP analogue in a rat model with a cholinergic deficit prevented the spatial learning and memory impairment associated with that model (Gozes et al. 1996). In another study, the protective effects of VIP against Aβ deposition on the APP/PS1 AD model were also reported (Song et al. 2012). However, as far as we know, there is no report showing the in vivo effect of chronic VIP administration on a model that well-mimics FAD, such as 5xFAD with its five different familial gene mutations. Thereby, we aimed to test the effects of chronic VIP application against Aβ pathology in the 5xFAD mouse model of AD.
Methods
Mice
5xFAD transgenic mice, developed by Oakley (Oakley et al. 2006), co-express human APP and PS1 genes harboring multiple mutations related to FAD [APP K670N/M671L (Swedish) + I716V (Florida) + V717I (London) and PS1 M146L + L286V] with neuronal expression driven by the Thy-1 promoter. The breeders, used in this study, were purchased from Jackson Laboratory. Only female mice were used in the present study (n = 10 mice per group). All animal experiments were conducted in accordance with the NIH Guide for the Care and Use of Laboratory Animals and were approved by the local animal care committee (251-J-031011).
Groups and Drug Protocol
We used 20 5xFAD mice in two groups: 1, 5xFAD mice that were exposed to VIP (Sigma-Aldrich) treatment (25 ng/kg i.p. injection, three times per week), and 2, 5xFAD mice that were exposed to saline injection (i.p. three times per week). Treatments started at 1 month of age just after weaning and continued for 2 months until 3 months of age.
Tissue Collection
Mice, at 3 months of age, were euthanized and their brains were removed. The brains were post-fixed with 4% paraformaldehyde solution for 24 h and cryoprotected in a graded series of 10% and 20% glycerol/2% DMSO solution. Only the right hemisphere was used for all procedures and analyses.
Immunohistochemistry
The cryoprotected brains were serially cut in coronal sections of 50 μm on a freezing microtome (Thermo HM450). Serial sections (7200 μm apart) encompassing the entire anterior to posterior brain were immunostained with antibodies against Aβ40 and Aβ42 (Invitrogen, Grand Island, NY, USA #44-348A, #44-344) to illuminate Aβ deposits. Immunohistochemical procedures were performed as previously described (Kowall et al. 2000). Briefly, free-floating sections were incubated overnight in primary antibody followed by PBS (phosphate-buffered saline) washes, incubation in peroxidase-conjugated secondary antibody, and development using 3,3′-diaminobenzidine tetrahydrochloride (DAB) as a chromagen.
Quantitative Analysis of Aβ Deposits
Plaque analysis was made with the use of the density probe included in the ImageJ software (NIH, Bethesda, MD, USA). Slides were photographed, and the area of interest was cropped using GIMP (GNU Image Manipulation Program). The cropped images were analyzed, and the densities were determined (pixel value in the selected area) with ImageJ.
Stereology
The aim of the stereological procedures was to obtain unbiased comparable numerical data from the brain sections. The evaluations were made using a Leica DM3000 stereomicroscope coupled to MBF’s Stereoinvestigator (MicroBrightField Inc., USA) unit. To standardize the quantification, an area of interest was determined for every evaluation area. For cortex estimations, a horizontal line beginning from the lowest portion of the medial cortex was drawn and the cortical area over the line was evaluated. For hippocampus estimations, Paxinos’s stereotaxic mouse brain atlas was used to determined sections corresponding to the diagrams between − 0.94 and − 3.80 mm. For brain volume estimations, the whole section area was evaluated. To estimate the volume of the fields of interest, the Cavalieri probe from the Stereoinvestigator software was used. Sections were selected by systematic randomized sampling (section thickness 50 μm). The first section in the series was randomly chosen from the first two sections. This section and every 12th section thereafter were analyzed for a total of seven sections. An unbiased counting frame with 300-μm-grid spacing was used with a randomized angle. The software calculated the total volume of the regions of interest using the following equation:
- V :
-
Volume (of area of interest)
- Q − :
-
Total counted number of points hitting area of interest
- a :
-
The unit area represented by each grid point (300 μ × 300 μ = 90,000 μ2)
- t :
-
The distance between two sections
Immunohistochemically stained plaque volumes were analyzed with the same method described above. A higher magnification and a counting frame of 150-μm-grid spacing were used. The sections were blindly evaluated as the researcher using the stereology unit was not aware of the codes related to the groups.
Statistical Analysis
Data are presented as the means and standard errors (mean ± SEM) of each group, and p < 0.05 was considered statistically significant. Statistical evaluation of the Aβ plaque intensities/volumes and brain volumes were performed using a t test, followed by the Mann–Whitney U test for comparisons by GraphPad Prism 6.0 statistical software.
Results
Two months of chronic VIP administration in 5xFAD mice significantly decreased Aβ40 (Fig. 1a, b, e; p < 0.01) and Aβ42 (Fig. 1c, d, f; p < 0.001) plaque density in the subiculum relative to saline-treated control animals (Fig. 1). VIP treatment also significantly decreased Aβ40 (Fig. 2a, b, e; p < 0.001) and Aβ42 (Fig. 2c, d, f; p < 0.05) plaque density in the cortex (Fig. 2).
Effect of VIP treatment (25 ng/kg, i.p.) on Aβ40 and Aβ42 pathology in the subiculum of 5xFAD mice. Plaque analysis was employed to quantify the density of Aβ plaques. Photomicrographs displaying Aβ1–40 immunohistochemical staining in 5xFAD-saline (a) and 5xFAD-VIP (b) representative sections; Aβ1–42 immunohistochemical staining for 5xFAD-saline (c) and 5xFAD-VIP (d) representative sections. Chronic VIP administration in 5xFAD mice significantly decreased Aβ40 (e) and Aβ42 (f) plaque load in the subiculum (**p < 0.01; ***p < 0.001; magnification × 20)
Effect of VIP treatment (25 ng/kg, i.p.) on Aβ40 and Aβ42 pathology in the cortex of 5xFAD mice. Plaque analysis was used to quantify the density of Aβ plaques. Photomicrographs displaying Aβ1–40 immunohistochemical staining in 5xFAD-saline (a) and 5xFAD-VIP (b) representative sections; Aβ1–42 immunohistochemical staining in 5xFAD-saline (c) and 5xFAD-VIP (d) representative sections. Chronic VIP administration in 5xFAD mice significantly decreased Aβ40 (e) and Aβ42 (f) plaque load in the cortical areas (*p < 0.05; ***p < 0.001; magnifications × 20)
Section interval and number was not sufficient to perform an accurate stereological estimation of plaque volume in the subiculum. However, chronic VIP administration significantly decreased the total cortical Aβ40 (Fig. 3a) and Aβ42 (Fig. 3b) plaque volume to cerebral cortex ratio.
Effect of VIP treatment (25 ng/kg, i.p.) on estimated total plaque volumes of Aβ40 and Aβ42 in cerebral cortex to cerebral cortex ratio in 5xFAD mice. Stereological methods were employed to quantify estimated volumes of plaques. Chronic VIP administration in 5xFAD mice significantly decreased total cortical Aβ40 (a) and Aβ42 (b) plaque volumes to cerebral cortex ratio (*p < 0.05). Cx cerebral cortex, Vv volume in volume)
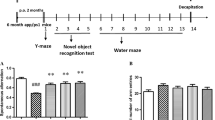
Chronic VIP administration did not have an effect on cerebellar volume (Fig. 4a) but significantly increased the cortical (Fig. 4b) and hippocampal (Fig. 4c) volumes in the treated 5xFAD mice. While the cerebral cortex to cerebrum ratio did not change (Fig. 4d), the hippocampus to cerebrum ratio significantly increased (Fig. 4e) after VIP treatment. Taken together, these data indicate that chronic VIP treatment prevents brain atrophy in the 5xFAD murine model of AD.
Effect of VIP treatment (25 ng/kg, i.p.) on estimated volumes of cerebrum (a), cerebral cortex (b), and hippocampus (c) in 5xFAD mice. Stereological methods were employed to quantify estimated volumes in the fields of interest. Chronic VIP administration in 5xFAD mice did not affect cerebrum volume (a) but significantly increased cortical and hippocampal volumes relative to saline-injected controls. While, cerebral cortex/cerebrum ratio did not change (d), hippocampus/cerebrum ratio significantly increased (e) after VIP treatment (*p < 0.05; **p < 0.01). Hip hippocampus, Cx cortex, Cr cerebrum
Discussion
The results of this study indicated that chronic VIP administration significantly decreased Aβ40 and Aβ42 plaques in the subiculum and cortex of 5xFAD mice. In addition to plaque inhibition, VIP also prevented brain atrophy in the 5xFAD mice.
Plaque aggregation in AD results from multifaceted cellular responses that include the activation of microglia and astrocytes contiguous with the amyloid plaque (Kalaria 1999; McGeer and McGeer 1999; Delgado et al. 2008). Many studies which describe elevated levels of inflammatory cytokines and chemokines and the occurrence of several acute-phase products in the AD brain (McGeer and McGeer 1998, 1999; Villoslada et al. 2008) support the participation of inflammatory factors in the pathophysiology of AD. Raised levels of Aβ in the AD brain stimulate microglial activation and the release of proinflammatory cytokines and other potentially neurotoxic elements, which cumulatively result in the neurodegeneration seen in many in vivo and in vitro experiments (McDonald et al. 1998; Weldon et al. 1998; Xie et al. 2002; Delgado et al. 2008; Choi et al. 2014; Carreras et al. 2013). Microglial activation and the neuroinflammatory changes detected in AD pathology are consequently assumed to contribute to the neuronal loss and dementia characteristic of this progressive disease. This supports the idea that anti-inflammatory substances can prevent Aβ accumulation and thus AD pathology. In a study by Delgado et al. (2008), VIP prevented Aβ-induced neurodegeneration in vitro by indirectly inhibiting the production of inflammatory and neurotoxic agents by activated microglia cells. The inhibitory effect of VIP appears to be mediated by blocking signaling through the p38 MAPK, p42/p44 MAPK, and NFκB cascades, which are the three transcription pathways responsible for the production of inflammatory mediators and free radicals in Aβ-activated microglia cells. In another study carried out on APP/PS1 mice by Song and colleagues, VIP promoted microglial phagocytosis of Aβ and suppressed the Aβ-induced release of microglial neurotoxins. In addition, inflammation and attenuated amyloidosis in the APP/PS1 transgenic mouse model of AD were reduced by the constitutive overexpression of VIP in the hippocampus (Song et al. 2012).
While there are limited research investigating the effects of VIP on AD pathology, the effects of another molecule, pituitary adenylyl cyclase-activating peptide (PACAP) on AD pathology may help inform the analysis our findings. Discovered almost three decades ago, PACAP is a 38-amino acid hypothalamic neuropeptide that is 70% identical to VIP. The actions of VIP and PACAP are mediated by three heterotrimeric G protein-linked receptors, termed PAC1, VPAC1, and VPAC2 (Harmar et al.1998), each with their own unique expression pattern. Of these, PAC1 binds PACAP exclusively with high affinity, whereas VPAC1 and VPAC2 can bind to either VIP or PACAP with the same affinity. An in vitro study using PC12 cells found that PACAP was more effective than VIP in terms of reducing Aβ42 toxicity and resulted in a significant increase in the activity of the PAC1 gene (Onoue et al. 2002). However, these results are limited due the use of PC12 cells, which are not reflective of the complex multicellular neural environment. However, a previous study by the same researchers showed that VIP may also act on the PAC1 receptor of PC12 cells (Onoue et al. 2001). In vivo, PACAP has a 1000-fold higher affinity for PAC1 receptors than VIP. In a study using both human primary neuronal cells and a 3xTG mice model of AD that has Tau and Aβ pathology, PACAP gene expression decreased in parallel with AD pathology. PACAP administration protected neurons against Aβ toxicity through the mitochondrial Sitrulin 3 (Sirt3) pathway (Han et al. 2014). A study in humans indicated that PACAP levels were decreased in AD patients (Han et al. 2014). A relationship was also reported between PACAP deficiency and the mild cognitive impairment dementia stage of AD (Han et al. 2015). In another study using APP-transgenic mice, long-term intranasal PACAP administration was shown to promote APP processing, to increase pro-neuronal BDNF and anti-apoptotic Blc2 levels, and to sharply reduce mRNA levels of the Aβ transporter receptor for advanced glycation end products (RAGE) (Rat et al. 2012). VIP also stimulated the same pathways as BDNF and Blc2 and reduced the Aβ plaque burden and volume in the present study.
In AD, after deterioration of neuronal physiology, the connection between neurons fail, injured neurons die, and, finally, many brain regions begin to shrink, thus causing the considerable loss of brain volume. Although plaque accumulation in 5xFAD mice arises very quickly and at young ages (1.5–2 months), dense neuronal loss and memory deficits are traditionally observed at about 9 months of age (Oakley et al. 2006). Therefore, hypothetically, at the beginning of the experiment, we did not expect to see any significant dimensional change after VIP treatment, because the pathology was at the level of the plaque formation. However, contrary to our hypothetical expectations, and despite the early age of disease progression in the 5xFAD mice, chronic injection of VIP significantly increased the volume of both the cortical and hippocampal regions. Similarly, a morphometric study in a PDAPP mice model of AD revealed that hippocampal and cortical atrophy was present at very early ages, even prior to plaque formation, although the characteristic feature of the model was late plaque deposition and neuronal loss (Redwine et al. 2003). An MRI study on non-demented AD patients revealed that atrophy begins in its early stages in the subiculum, which causes mild memory dysfunction in non-demented individuals (Lindberg et al. 2017).
Our previous studies indicated that VIP increases gamma-aminobutyric acid (GABA) and glutamate levels in the brain of parkinsonian rats; these findings are of importance as increased GABA and glutamate can induce neuronal repair (Yelkenli et al. 2016). A major inhibitory neurotransmitter in the adult brain, GABA, has critical roles involved in multiple steps of adult neurogenesis. GABA regulates the development of neural stem/precursor cells (NSPCs) and their neuronal progeny in the adult brain. GABA plays a potential role as a sensor of neuronal activity and as a key regulator of the speed and extent of adult mammalian neurogenesis, as well (Ge et al. 2008). Tonic GABA release promotes the neuronal differentiation of NSPCs. Additionally, VIP induces VPAC receptors that promote the survival of proliferating nestin-expressing precursors and promotes their differentiation into a neurogenic fate (Nunan et al. 2014; Zaben et al. 2009). Thus, it is possible that VIP prevents brain atrophy in 5xFAD mice by increasing neurogenesis.
VIP is neurotrophic and induces neuronal plasticity in parkinsonian rats (Korkmaz et al. 2012). During mouse embryogenesis and within the process of the neonatal development of rats, VIP-mediated axonal and dendritic growth and synaptogenesis have been described (Hill et al. 1994; Zhang et al. 2002; Hill et al. 2007). VIP-stimulated glial cells trigger neurotrophic and synaptogenic activity through activity-dependent neurotrophic factor (ADNF), NAP, and other similar peptides (Brenneman and Gozes 1996; Brenneman 1988; Smith- Swintosky et al. 2005; Incerti et al. 2010). ADNF-9 and NAP treatment increased synaptophysin expression, representative of an augmentation in synapse formation, in hippocampal and cortical cell cultures (Smith-Swintosky et al. 2005). It has been reported that VIP applications after excitotoxic damage resulted neuroprotective effects mediated by BDNF (Rangon et al. 2006). Furthermore, VIP stimulates the release of BDNF in primary cultures of cortical neurons and astrocytes (Pellegri et al. 1998). BDNF and other neurotrophins are not only vital to healthy neuronal development and neuro-protection but they also play major roles in synaptic plasticity and dendritic morphology (Jan and Jan 2003; Incerti et al. 2010; Magarinos et al. 2011). Stranahan and colleagues (Stranahan 2011) demonstrated that BDNF expression is positively correlated with the number of dendritic spines in the dentate granular neurons of mice (Aytan et al. 2018). Therefore, the VIP-induced stimulation of neurotrophic factors might be another mechanism underlying the pro-survival effect of VIP on 5xFAD mice.
Conclusions
In summary, in the present study, chronic VIP treatment significantly decreased Aβ40 and Aβ42 plaques in the subiculum and cortex of 5xFAD mice. In addition to plaque inhibition, VIP also prevented atrophy in the 5xFAD mice. We thus conclude that VIP and its analogues represent very promising therapeutic approaches for the treatment of AD.
References
Aytan N, Choi JK, Carreras I, Crabtree L, Nguyen B, Lehar M, Blusztajn JK, Jenkins BG, Dedeoglu A (2018) Protective effects of 7,8-dihydroxyflavone on neuropathological and neurochemical changes in a mouse model of Alzheimer's disease. Eur J Pharmacol 3 828:9–17
Bayer TA, Wirths O, Majtényi K, Hartmann T, Multhaup G, Beyreuther K, Czech C (2001) Key factors in Alzheimer's disease: beta-amyloid precursor protein processing, metabolism and intraneuronal transport. Brain Pathol 11(1):1–11, 1
Bertram L, Lill CM, Tanzi RE (2010) The genetics of Alzheimer disease: back to the future. Neuron 68(2):270–281
Brenneman DE (1988) Regulation of activity-linked neuronal survival by vasoactive intestinal peptide. Ann NYAcad Sci 527:595–597
Brenneman DE, Gozes I (1996) A femtomolar-acting neuroprotective peptide. J Clin Invest 97(10):2299–2307
Carreras I, McKee AC, Choi JK, Aytan N, Kowall NW, Jenkins BG, Dedeoglu A (2013) R-flurbiprofen improves tau, but not Aß pathology in a triple transgenic model of Alzheimer’s disease. Brain Res 1541:115–127
Choi JK, Carreras I, Aytan N, Jenkins-Sahlin E, Dedeoglu A, Jenkins BG (2014) The effects of aging, housing and ibuprofen treatment on brain neurochemistry in a triple transgene Alzheimer’s disease mouse model using magnetic resonance spectroscopy and imaging. Brain Res 1590:85–96
Delgado M, Varela N, Gonzalez-Rey E (2008) Vasoactive intestinal peptide protects against beta-amyloid-induced neurodegeneration by inhibiting microglia activation at multiple levels. Glia 56(10):1091–1103
Deng G, Jin L (2017) The effects of vasoactive intestinal peptide in neurodegenerative disorders. Neurol Res 39(1):65–72
Dogrukol-Ak D, Banks WA, Tuncel N, Tuncel M (2003) Passage of vasoactive intestinal peptide across the blood-brain barrier. Peptides 24(3):437–444
Ge S, Sailor KA, Ming GL, Song H (2008) Synaptic integration and plasticity of new neurons in the adult hippocampus. J Physiol 586(16):3759–3765
Gonzales-Reyes R, Nava-Mesa MO, Vargas-Sanches K, Ariza-Salamanca D, Mora-Munoz L (2017) Involvement of astrocytes in Alzheimer’s disease from a neuroinflammatory and oxidative stress perspective. https://doi.org/10.3389/fnmol.2017.00427
Gouras GK1, Olsson TT, Hansson O (2015) β-Amyloid peptides and amyloid plaques in Alzheimer’s disease. Neurotherapeutics 12(1):3–11
Gozes I, Bardea A, Reshef A, Zamostiano R, Zhukovsky S, Rubinraut S, Fridkin M, Brenneman DE (1996) Neurobiology neuroprotective strategy for Alzheimer disease: intranasal administration of a fatty neuropeptide. Proc Natl Acad Sci U S A 93:427–432
Han P, Caselli RJ, Baxter L, Serrano G, Yin J, Beach TG, Reiman EM, Shi J (2015) Association of pituitary adenylate cyclase-activating polypeptide with cognitive decline in mild cognitive impairment due to Alzheimer disease. JAMA Neurol 72(3):333–339
Han P, Tang Z2, Yin J et al. (2014) Pituitary adenylate cyclase-activating polypeptide protects against β-amyloid toxicity. Neurobiol Aging ;35(9):2064–2071
Hardy J (2002) Testing times for the “amyloid cascade hypothesis”. Neurobiol Aging 23(6):1073–1074
Harmar AJ, Arimura A, Gozes I, Journot L, Laburthe M, Pisegna JR, Rawlings SR, Robberecht P, Said SI, Sreedharan SP, Wank SA, Waschek JA (1998) International Union of Pharmacology. XVIII. Nomenclature of receptors for vasoactive intestinal peptide and pituitary adenylate cyclase-activating polypeptide. Pharmacol Rev 50(2):265–270
Hill JM, Hauser JM, Sheppard LM, Abebe D, Spivak-Pohis I, Kushnir M, Deitch I, Gozes I (2007) Blockage of VIP during mouse embryogenesis modifies adult behaviour and results in permanent changes in brain chemistry. J Mol Neurosci 31(3):183–200
Hill JM, Mervis RF, Politi J, McCune SK, Gozes I, Fridkin M, Brenneman DE (1994) Blockade of VIP during neonatal development induces neuronal damage and increases VIP and VIP receptors in brain. Ann N Y Acad Sci 739:211–225
Incerti M, Vink J, Roberson R, Benassou I, Abebe D, Spong CY (2010) Prevention of the alcohol-induced changes in brainderived neurotrophic factor expression using neuroprotective peptides in a model of fetal alcohol syndrome. Am J Obstet Gynecol 202(5):457 e1–4
Jan YN, Jan LY (2003) The control of dendrite development. Neuron 40(2):229–242
Kalaria RN (1999) Microglia and Alzheimer’s disease. Curr Opin Hematol 6(1):15–24
Korkmaz O, Ay H, Ulupinar E, Tunçel N (2012) Vasoactive intestinal peptide enhances striatal plasticity and prevents dopaminergic cell loss in Parkinsonian rats. J Mol Neurosci 48(3):565–573
Kowall NW, Hantraye P, Brouillet E, Beal MF, McKee AC, Ferrante RJ (2000) MPTP induces alpha-synuclein aggregation in the substantia nigra of baboons. Neuroreport 11(1):211–213
Lindberg O, Mårtensson G, Stomrud E, Palmqvist S, Wahlund LO, Westman E, Hansson O (2017) Atrophy of the posterior subiculum is associated with memory impairment, tau- and Aβ pathology in non-demented individuals. Front Aging Neurosci 9:306
Magarinos AM, Li CJ, Gal TJ et al (2011) Effect of brain-derived neurotrophic factor haploinsufficiency on stress-induced remodelling of hippocampal neurons. Hippocampus 21(3):253–264
McDonald DR, Bamberger ME, Combs CK, Landreth GE (1998) Beta-amyloid fibrils activate parallel mitogen-activated protein kinase pathways in microglia and THP1 monocytes. J Neurosci 18(12):4451–4460
McGeer EG, McGeer PL (1998) The importance of inflammatory mechanisms in Alzheimer disease. Exp Gerontol 33(5):371–378
McGeer EG, McGeer PL (1999) Brain inflammation in Alzheimer disease and the therapeutic implications. Curr Pharm Des 5(10):821–836
Meraz-Ríosv MA, Toral-Rios D, Franco-Bocanegra D, Villeda-Hernández J, Campos-Peña V (2013) Inflammatory process in Alzheimer’s disease. Front Integr Neurosci 7:59
Nunan R, Sivasathiaseelan H, Khan D, Zaben M, Gray W (2014) Microglial VPAC1R mediates a novel mechanism of neuroimmune-modulation of hippocampal precursor cells via IL-4 release. Glia 62(8):1313–1327
Oakley H, Cole SL, Logan S, Maus E, Shao P, Craft J, Guillozet-Bongaarts A, Ohno M, Disterhoft J, Van Eldik L, Berry R, Vassar R (2006) Intraneuronal beta-amyloid aggregates, neurodegeneration, and neuron loss in transgenic mice with five familial Alzheimer's disease mutations: potential factors in amyloid plaque formation. J Neurosci 26(40):10129–10140
Onoue S, Endo K, Ohshima K, Yajima T, Kashimoto K (2002) The neuropeptide PACAP attenuates beta-amyloid (1-42)-induced toxicity in PC12 cells. Peptides 23(8):1471–1478
Onoue S, Waki Y, Nagano Y, Satoh S, Kashimoto K (2001) The neuromodulatory effects of VIP/PACAP on PC-12 cells are associated with their N-terminal structures. Peptides 22(6):867–872
Pellegri G, Magistretti PJ, Martin JL (1998) VIP and PACAP potentiate the action of glutamate on BDNF expression in mouse cortical neurones. Eur J Neurosci 10(1):272–280
Philipson O, Lord A, Gumucio A, O'Callaghan P, Lannfelt L, Nilsson LN (2010) Animal models of amyloid-beta-related pathologies in Alzheimer’s disease. FEBS J 277(6):1389–1409
Rangon CM, Dicou E, Goursaud S et al (2006) Mechanisms of VIP induced neuroprotection against neonatal excitotoxicity. Ann N Y Acad Sci 1070:512–517
Rat D1, Schmitt U, Tippmann F et al. (2012) Neuropeptide pituitary adenylate cyclase-activating polypeptide (PACAP) slows down Alzheimer’s disease-like pathology in amyloid precursor protein-transgenic mice. FASEB J 25(9):3208–3218
Redwine JM, Kosofsky B, Jacobs RE, Games D, Reilly JF, Morrison JH, Young WG, Bloom FE (2003) Dentate gyrus volume is reduced before onset of plaque formation in PDAPP mice: a magnetic resonance microscopy and stereologic analysis. Proc Natl Acad Sci U S A 100(3):1381–1386
Smith-Swintosky VL, Gozes I, Brenneman DE, D'Andrea MR, PlataSalaman CR (2005) Activity-dependent neurotrophic factor-9 and NAP promote neurite outgrowth in rat hippocampal and cortical cultures. J Mol Neurosci 25(3):225–238
Solito E, Sastre M (2012) Microglia function in Alzheimer’s disease. Front Pharmacol 3:14
Song M, Xiong JX, Wang YY, Tang J, Zhang B, Bai Y (2012) VIP enhances phagocytosis of fibrillar beta-amyloid by microglia and attenuates amyloid deposition in the brain of APP/PS1 mice. PLoS One 7(2):e29790
Stranahan AM (2011) Physiological variability in brain-derived neurotrophic factor expression predicts dendritic spine density in the mouse dentate gyrus. Neurosci Lett 9;495(1):60-62
Villoslada P, Moreno B, Melero I et al (2008) Immunotherapy for neurological diseases. Clin Immunol 128(3):294–305
Weldon DT, Rogers SD, Ghilardi JR, Finke MP, Cleary JP, O'Hare E, Esler WP, Maggio JE, Mantyh PW (1998) Fibrillar beta-amyloid induces microglial phagocytosis, expression of inducible nitric oxide synthase, and loss of a select population of neurons in the rat CNS in vivo. J Neurosci 18(6):2161–2173
Xie Z, Wei M, Morgan TE, Fabrizio P, Han D, Finch CE, Longo VD (2002) Peroxynitrite mediates neurotoxicity of amyloid beta-peptide1-42- and lipopolysaccharide-activated microglia. J Neurosci 22(9):3484–3492
Yelkenli IH, Ulupinar E, Korkmaz OT, Şener E, Kuş G, Filiz Z, Tunçel N (2016) Modulation of corpus striatal neurochemistry by astrocytes and vasoactive intestinal peptide (VIP) in parkinsonian rats. J Mol Neurosci 59(2):280–289
Zaben M, Sheward WJ, Shtaya A, Abbosh C, Harmar AJ, Pringle AK, Gray WP (2009) The neurotransmitter VIP expands the pool of symmetrically dividing postnatal dentate gyrusprecursors via VPAC2 receptors or directs them toward a neuronal fate via VPAC1 receptors. Stem Cells 27(10):2539–2551
Zhang QL, Liu J, Lin PX, Webster HD (2002) Local administration of vasoactive intestinal peptide after nerve transection accelerates early myelination and growth of regenerating axons. J Peripher Nerv Syst 7:118–127
Acknowledgements
The authors thank to Lokman Hossain for animal husbandry.
Funding
This research is supported by grants from NIA (R01AG031896, RF1AG056032) and the Department of Veteran Affairs (Merit Award; 5I01BX001875-03) to A. Dedeoglu and P30AG013846 to NW Kowall, and Scientific and Technical Research Council of Turkey (TUBITAK, 1059B190900502) to O.T. Korkmaz.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of Interest
The authors declare that they have no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Korkmaz, O.T., Ay, H., Aytan, N. et al. Vasoactive Intestinal Peptide Decreases β-Amyloid Accumulation and Prevents Brain Atrophy in the 5xFAD Mouse Model of Alzheimer’s Disease. J Mol Neurosci 68, 389–396 (2019). https://doi.org/10.1007/s12031-018-1226-8
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12031-018-1226-8